What is SVC Syndrome?
SVC syndrome ( Wolf - Parkinson - White syndrome or WPW syndrome) is a rare congenital heart defect characterized by abnormalities in the heart's electrical system. In people with WPW syndrome, there is an abnormal alternative electrical pathway (accessory pathway) between the atrium and ventricle, resulting in an abnormal heartbeat (arrhythmia) and an increased heart rate (tachycardia).
The heart of a normal, healthy person has four chambers. The two upper chambers are the atria, the two lower chambers are the ventricles.
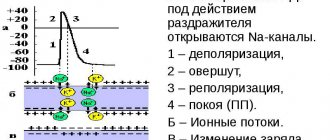
In the right atrium of a normal heart there is a natural pacemaker (sinoatrial node, Kis-Flac node), which initiates and controls the heartbeat. When the Kis-Flaca node fires, electrical activity spreads through the right and left atria, causing them to contract. Impulses travel to the atrioventricular node (AV node, Aschoff–Tawar node), which is the bridge that allows impulses to travel from the atria to the ventricles. The impulse then passes through the walls of the ventricles, causing them to contract. The regular pattern of the heart's electrical impulses causes the heart to fill with blood and contract normally.
The extra electrical pathway in people with SVC syndrome bypasses the normal pathway and causes the ventricles to beat earlier than normal (pre-excitation) and may allow electrical impulses to be conducted in both directions (i.e., from the atria to the ventricles and from the ventricles to the atria).
WPW syndrome - what is it?
According to statistics, heart rhythm disturbances due to WPW syndrome are detected only in 0.15–2% of cases.
The disease is more common among men and usually appears between 10 and 20 years of age. It leads to severe heart rhythm disturbances, requires a special approach to diagnosis and treatment, and can pose a threat to the patient’s life. Classification of WPW syndrome
In cardiology, a distinction is made between the phenomenon of SVC and SVC syndrome. The first is characterized by electrocardiographic signs of cardiac impulse conduction through additional connections and overexcitation of the ventricles. In this case, there are no clinical manifestations of AV reciprocal tachycardia. WPW heart syndrome is a combination of ventricular overexcitation with symptoms of tachycardia.
Taking into account the morphological substrate, scientists identify the following anatomical types of SVC syndrome:
1. With additional muscle AV fibers. Muscle fibers can:
- pass through the accessory right/left parietal AV junction;
- go from the right/left atrial appendage;
- be associated with a sinus of Valsalva/middle vein vein aneurysm;
- go through the fibrous aortic-mitral junction;
- be paraseptal, septal superior/inferior.
2. With bundles of Kent (muscle AV fibers) originating from rudimentary tissue:
- and entering the myocardium of the right ventricle;
- and entering the right bundle branch (atrio-fascicular).
According to the nature of the manifestation they are classified:
- Manifesting WPW syndrome. Characterized by the constant presence of a delta wave, episodes of atrioventricular reciprocal tachycardia and sinus rhythm;
- Transient WPW syndrome (also known as intermittent WPW syndrome). The ECG diagnoses sinus rhythm, transient ventricular preexcitation, verified atrioventricular reciprocal tachycardia;
- Hidden WPW syndrome. Described by retrograde conduction along the bundle of Kent. The ECG reveals episodes of atrioventricular reciprocal tachycardia (at rest, the anomaly is not diagnosed using an ECG). Manifested by attacks of tachycardia.
According to the location, Keta bundles can be:
- left-sided (go from the left atrium to the left ventricle);
- right-sided (go from the right atrium to the right ventricle);
- paraseptal (go near the cardiac septum).
The location of the additional pathway is taken into account by cardiologists-arrhythmologists when choosing the most effective surgical access technique (through a vein or through the femoral artery).
SVC syndrome and pregnancy
SVC syndrome, which does not manifest itself clinically, does not require additional treatment. But during pregnancy, the disease can manifest itself with paroxysmal heart rhythm disturbances. Then a consultation with a cardiologist and selection of effective treatment is necessary.
With very frequent attacks of tachycardia against the background of WPW syndrome, pregnancy is contraindicated. This is explained by the fact that the disease at any period can develop into a life-threatening rhythm disorder. In addition, tachycardia often provokes insufficient blood circulation in organs and tissues, which negatively affects not only the condition of the mother, but also the development of the fetus.
Signs and symptoms
Symptoms associated with SVC syndrome vary greatly from case to case. Some patients do not have any heart rhythm disturbances or associated symptoms (ie, asymptomatic disease). Although the disorder is present at birth, symptoms may not appear until adolescence or early adulthood.
People with Wolff-Parkinson-White syndrome may have one or more irregular heartbeats, especially episodes of abnormally fast heartbeats that occur over the ventricles (supraventricular tachycardia). These episodes often start and end suddenly and can last from a few minutes to several hours. The frequency of episodes varies from case to case. Some people experience episodes every week, others only a few sporadic episodes.
During these episodes, a variety of symptoms may occur, including:
- cardiopalmus;
- difficulty breathing (shortness of breath);
- dizziness;
- chest pain;
- decreased tolerance to physical activity;
- anxiety;
- dizziness.
In some cases, victims lose consciousness (fainting).
Some people with WPW syndrome may experience atrial flutter, in which the atrium beats regularly at an extremely high rate, or atrial fibrillation, in which there is a rapid, irregular twitching of the muscle wall.
In extremely rare cases, affected people may develop ventricular fibrillation, a serious condition in which the heart's normal electrical activity is disrupted, resulting in uncoordinated heartbeats and failure of the heart's main pumping chambers (ventricles). Although rare in WPW syndrome, ventricular fibrillation can potentially lead to cardiac arrest and sudden death.
Symptoms of Wolff-Parkinson-White syndrome
If during tachycardia the heart rate does not exceed 200 beats per minute, the syndrome usually occurs without characteristic symptoms, and the person does not even suspect that he has a congenital anomaly. Pathology is detected only with cardiographic diagnosis.
If the heart rate is more than 200 beats per minute, a person has a feeling that the heart is about to “jump out”, dizziness occurs, a pre-fainting state appears, even to the point of loss of consciousness. An attack can also provoke severe hemodynamic disturbances and cardiac arrest.
Causes and risk factors
Most cases of SVC syndrome occur randomly in the general population for no apparent reason (sporadic) and are not inherited. Some cases of SVC syndrome are inherited and may be inherited as an autosomal dominant trait.
Genetic diseases are determined by two genes, one of which a person receives from his father and the other from his mother. Dominant genetic disorders occur when only one copy of the abnormal (defective) gene is needed to cause the disease. The abnormal gene may be inherited from either parent or result from a new mutation (gene change) in the person affected by the disease. The risk of passing an abnormal gene from an affected parent to offspring is 50% in each pregnancy, regardless of the sex of the unborn child.
No specific genetic mutation has been identified in individuals with isolated WPW syndrome, and the exact role of genetics in the development of the syndrome is not fully understood. However, a rare autosomal dominant disorder known as familial Wolff-Parkinson-White syndrome has been linked to chromosome 7. Scientists have determined that mutations in the regulatory subunit of the AMP-activated protein kinase gene gamma 2 (PRKAG2), located on the long arm (q) of the chromosome 7 (7q36) cells cause this disorder, which includes features of WPW syndrome, progressive conduction block, and excessive growth of part of the heart (cardiac hypertrophy).
Some scientists believe that familial SVC syndrome is a glycogen storage disorder, a group of disorders in which stored glycogen, normally broken down into glucose to supply the body with energy, accumulates in various organs. SVC syndrome is known to occur as part of other glycogen storage disorders, particularly Pompe disease or Danon disease.
Approximately 7 to 20% of patients with WPW syndrome have a congenital heart defect such as Ebstein's anomaly, a condition that causes abnormality of the tricuspid valve. The tricuspid valve connects the right atrium to the right ventricle.
The symptoms of SVC syndrome result from the presence of an alternative electrical pathway. A normal heart has one pathway (the sinoatrial node) that carries electrical impulses from the small chambers of the heart (atria) to the larger chambers (ventricles). These electrical impulses cause the muscles in the atria and then the ventricles to contract and relax, pumping blood throughout the body. Patients with SVC syndrome have a second abnormal conduction pathway called the bundle of Kent, which sends additional electrical impulses from the muscles of the atria to the muscles of the ventricles. These extra electrical impulses bypass the normal route and disrupt the normal rhythm of the heartbeat and cause abnormalities, usually rapid contractions, known as “atrial flutter, atrial fibrillation, or paroxysmal supraventricular tachycardia.” The exact cause of alternative pathways is unknown.
INTERNAL FIRE PIPING
Internal fire water supply
Internal fire water supply
- this is a set of pipelines and technical means that provide water supply to fire hydrants (see FIRE PLUG) [].
Variants of the term from other sources:
ERW (internal fire water supply) -
A set of pipelines and technical means that ensure the supply of fire extinguishing agent to fire shut-off valves of fire hydrants and/or fire shut-off valves of dry pipes.
(SP 10.13130.2020 “Fire protection systems. Internal fire water supply. Design standards and rules”)
Purpose of internal fire water supply
The purpose, goals of design, creation of internal fire-fighting water supply are determined by the need to provide protected construction sites with an effective means of extinguishing fires (see FIRE EXTINGUISHING) at the initial stage of fire development (see FIRE), which, after a short training, practical training, can be used by daytime, shift, duty personnel of organizations.
Rice. 1 Installation of internal fire water supply in the building
The presence of internal fire-fighting water supply at protection facilities (see OBJECT OF PROTECTION) allows you to quickly, with minimal forces and means, eliminate (see FIRE ELIGIBILITY) fires (see FIRE SOCIETY), prevent the spread of fire (see FIRE LOCALIZATION) before the arrival of employees fire departments (see FIRE SERVICE), formations. Fire departments can also use PCs to extinguish fires during fire investigations.
The use of internal fire-fighting water supply at protection facilities - from explosive and fire-hazardous production facilities, warehouse complexes to public, administrative buildings, high-rise apartment buildings - its correct operation, use in emergency situations (see EMERGENCY SITUATION) allows you to save lives, preserve material values and property [ 2].
Classification of internal fire-fighting water supply systems
Internal fire water supply can be:
— special
;
Special
internal fire water supply system performs exclusively the functions of internal fire water supply system and is recommended for high-rise buildings. Only steel pipes should be used in dedicated indoor fire water piping.
— multifunctional.
Multifunctional
The internal fire-fighting water supply can be combined with a household or industrial water supply or with the water supply of automatic fire extinguishing installations (AUP).
Types of water supply network:
— dead end;
Dead-end network
allowed when the number of fire hydrants in the building is no more than 12.
— ring
.
On a ring water supply network
install shut-off devices that make it possible to exclude faulty sections of the network from the water supply scheme, or fire or drinking water risers located in this area. These shut-off devices must allow water to pass in both directions with minimal hydraulic losses [2].
Designation of internal fire water supply
Graphic symbols for internal fire water supply are regulated by GOST 12.4.026-2015. The sign “Fire hydrant” (F02) is used - a schematic drawing of a fire hose with a valve in a square on a red background [5].
Rice. 2 Internal fire water supply designation sign
The plate indicates the letter index PC with the serial number according to the hydraulic circuit, as well as the telephone number of the fire department. Painting of pipes and cabinets is red.
Installation of internal fire-fighting water supply
The internal fire water supply system consists of the following parts:
— valves, instrumentation and automation devices
at the entrance to a building, structure;
— pumping station
, necessary to increase pressure when there is insufficient pressure of water taken from external networks. Placed on the first, technical, basement floors of protection facilities, both in specially designated rooms and in heating units, boiler rooms, heating points;
— water tanks
containing the supply of water necessary to start extinguishing before starting the pumps installed as necessary;
— main vertical
,
distributing horizontal pipelines
of the fire-fighting water supply system;
— internal fire hydrants (PC)
, installed along escape routes, at exits from floors, from the building, at a height of 1.35 m from the floor surface;
— manual
fire nozzles
(see FIRE HOSE)
and hoses
(see FIRE HOSE)
with connecting heads
placed in fire cabinets (see FIRE CABINET) near the shut-off valves of the PC;
— manual call points
, installed on each PC, which serve as a manual start button for fire pumps.
All fire cabinets of the protected object are equipped with trunks and hoses connected to them and to the valves of the tap. The cabinets are locked and sealed.
The internal fire water supply system of the building must always be in a fully equipped and operational condition. Indeed, in the event of an emergency, he must ensure liquidation (see FIRE ELIGIBILITY) or localization of the fire FIRE LOCALIZATION
— actions aimed at preventing the possibility of further spread of fire and creating conditions for its elimination using available forces and means. (see FIRE LOCALIZATION), enable people in the building to leave it (see EVACUATION), using evacuation routes (see EMERGENCY ROUTE), exits (see EMERGENCY EXIT).
Requirements for the installation of internal fire water supply
Article 86. Requirements for internal fire water supply
[3].
1. The internal fire-fighting water supply must provide the standard water flow for extinguishing fires in buildings and structures.
2. The internal fire-fighting water supply system is equipped with internal fire hydrants in a quantity that ensures the achievement of fire extinguishing goals.
3. Requirements for internal fire-fighting water supply are established by regulatory documents on fire safety.
The set of rules SP 10.13130.2020 contains precise instructions, which mainly boil down to the requirement for such an indicator as water consumption for internal fire extinguishing. This parameter is almost the same for all types of buildings and is equal to 2.5 l/s.
Also another important parameter is the number of fire trunks. This parameter will depend on the size of the building in question.
For example:
· for residential buildings of 16 floors and below, 1 PC is installed on each floor, but if the length of the corridor exceeds 10 m, then 2 PCs;
· if the number of floors in buildings is between 16 and 25 floors, then there should be two PCs, if the length of the corridor exceeds 10 m - then 3;
· office building with a volume of up to 25,000 m³, 6–10 storeys, 1 PC is installed, with a volume above 25,000 m³ - 2 PCs;
· number of floors above 10, volume up to 25,000 m³ - 2 pcs, the same only with a volume above 25,000 m³ - 3 pcs.
It is also necessary to take into account that the installation of internal fire water supply is not necessary, prohibited or impractical in a number of objects. The list of such objects is presented in clause 4.1.5 of SP 10.13130.2020.
1.4 Internal fire water supply is not required
[]:
-in the buildings of general educational organizations (schools, gymnasiums, lyceums, except boarding schools), preschool educational organizations (kindergartens);
-in the buildings of seasonal cinemas for any number of seats; in baths and saunas;
- in industrial and warehouse buildings of I and II degrees of fire resistance of categories G and D, regardless of their volume, as well as industrial and warehouse buildings of III - V degrees of fire resistance of categories G and D with a volume of no more than 5000 m3;
-in buildings storing roughage, pesticides and mineral fertilizers;
-in industrial buildings for the processing of agricultural products of category B, I and II degrees of fire resistance with a volume of up to 5000 m3;
-in transformer substations and in rooms with electrical power equipment, including pumping stations and ventilation chambers.
Table 7.1 SP 10.13130.2020 establishes the number of fire trunks and the minimum water consumption for internal fire extinguishing [].
| Residential, public and administrative buildings | Number of pcs for flow calculation | Minimum flow rate of dictating PC-s, l/s |
| 1. Multi-apartment residential buildings <*> (F1.3), dormitories and apartment-type hotels, including apartments, located in buildings F1.2: with a number of floors from 12 to 16 inclusive (or with a building height of 30 to 50 m inclusive) with a total corridor length of up to 10 m inclusive) | 1 | 2,5 |
| the same for the total length of the corridor over 10 m; | 2 | 2,5 |
| with a number of floors over 16 to 25 inclusive (or with a building height over 50 to 75 m inclusive) <**> regardless of the length of the corridor. | 2 | 2,5 |
| 2. Corridor and non-corridor type buildings: administrative, public, public utilities (F3.5), administrative and residential production enterprises, management bodies, institutions, design organizations, information, editorial and publishing organizations and scientific organizations, banks , offices, offices (F4.3), hotels (F1.2), clinics (F3.4), sports and recreation complexes and sports training institutions (F3.6), buildings of educational institutions of higher professional education (F4.2) : | ||
| with a number of floors from 6 to 10 inclusive (or with a building height of 18 to 30 m inclusive) <**>; | 1 | 2,5 |
| with the number of floors over 10 to 16 inclusive (or with a building height over 30 to 50 m inclusive) <**>. | 2 | 2,5 |
| 3. Buildings of specialized homes for the elderly and disabled (non-residential), hospitals, dormitory buildings of boarding educational institutions (F1.1) regardless of volume: | ||
| with a number of floors up to 3 inclusive (or with a building height up to 8 m inclusive) <**>; | 1 | 2,5 |
| when the number of floors is over 3 (or when the building height is over 8 m) <**>. | 2 | 2,5 |
| 4. Buildings of theaters, cinemas, concert halls, clubs, circuses and other similar institutions with an estimated number of seats for visitors in enclosed spaces (F2.1): | ||
| with an auditorium capacity of up to 300 seats inclusive; | 1 | 2,5 |
| with a capacity of more than 300 seats in the auditorium. | 2 | 2,5 |
| 5. Buildings of libraries and archives (F2.1), sports facilities (F2.1, F3.6), as well as laboratories, workshops, book depositories and archives (F5.1 and F5.2) and other similar institutions with an estimated number of seats places for visitors in enclosed spaces up to 50 m high inclusive: | ||
| with a total area of up to 2.5 thousand m2 inclusive; | 1 | 2,5 |
| with a total area of over 2.5 thousand m2. | 2 | 2,5 |
| 6. Buildings of museums, exhibition halls, dance halls and other similar institutions in enclosed spaces (F2.2), buildings of trade organizations (F3.1): | ||
| with a number of floors up to 3 inclusive (or with a building height up to 8 m inclusive) <**>; | 1 | 2,5 |
| the same for the number of floors more than 3 (or for a building height of up to 28 m inclusive) <**>. | 2 | 2,5 |
| 7. Corridor-type dormitory buildings (F1.2): | ||
| with a number of floors up to 10 inclusive (or with a building height up to 28 m inclusive) <**>; | 1 | 2,5 |
| with the number of floors over 10 to 16 inclusive (or with a building height over 28 m) <**>. | 2 | 2,5 |
Table 7.2 SP 10.13130.2020 establishes the number of fire nozzles and the minimum water consumption for internal fire extinguishing in production and warehouse premises [].
| Fire resistance level of buildings | Category of buildings by fire hazard | Structural fire hazard class | Number of PC-s for calculating flow rate and the minimum flow rate of the dictating PC-s, l/s, for industrial and warehouse buildings with a height of up to 50 m inclusive and volume, thousand m3 inclusive | |
| From 0.5 to 150 | Over 150 | |||
| I and II | A B C | C0, C1 | 2 x 2.5 | 3 x 2.5 |
| III | A B C | C0 | 2 x 2.5 | 3 x 2.5 |
| G, D | C0, C1 | — | 2 x 2.5 | |
| IV | A, B | C0 | 2 x 2.5 | 3 x 2.5 |
| IN | C0, C1 | 2 x 2.5 | 2 x 5 | |
| IN | C2, C3 | 3 x 2.5 | 4 x 2.5 | |
| G, D | C0, C1, C2, C3 | — | 2 x 2.5 | |
| V | IN | Not normal. | 2 x 2.5 | 2 x 5 |
| G, D | Not normal. | 1 x 2.5 | 2 x 2.5 | |
Note
For buildings, the degree of fire resistance and the fire hazard category of which are not indicated jointly in the table, the development of
special technical conditions to justify water consumption is required.
Rice. 3 Testing of internal fire water supply for water loss
Tests of internal fire-fighting water supply systems for operability (water yield) and serviceability of fire hydrant valves are carried out in accordance with the “Methodology for testing internal fire-fighting water supply systems” developed by the Federal State Budgetary Institution VNIIPO EMERCOM of Russia [4].
For detailed information about fire-fighting water supply and internal water supply, see the link.
Literature:
1.
SP 10.13130.2020 “Fire protection systems.
Internal fire water supply. Fire safety requirements" 2.
Encyclopedia "Fire Safety", FGU VNIIPO EMERCOM of Russia, 2007.
3. Federal Law of July 22, 2008 No. 123 "Technical Regulations on Fire Safety Requirements"
4.
Educational and methodological manual “Methodology for testing internal fire-fighting water supply systems”, FGU VNIIPO, 2007.
5.
GOST 12.4.026-2015 “System of occupational safety standards (SSBT).
Signal colors, safety signs and signal markings. Purpose and rules of use. General technical requirements and characteristics. Test methods" Copyright holder:
Portal about fire safety propb.ru.
Rules for using materials from the portal (site) PROPB.RU
← PreviousNext →
Return to list
Diagnostics
The diagnosis of SVC syndrome is based on a thorough clinical assessment, a detailed patient history and various specialized tests. Such studies may include:
- electrocardiogram (ECG);
- Holter monitoring;
- electrophysiological study.
An electrocardiogram records the heart's electrical impulses and can reveal abnormal electrical patterns. Holter monitoring is a portable device designed to continuously monitor the electrical activity of the heart. The device is usually worn for 24 hours. During electrophysiology tests, a thin tube (catheter) is inserted into a blood vessel and attached to the heart, where it measures electrical activity. Each of these specialized tests can detect abnormal heart rhythms associated with WPW syndrome.
Some patients with SVC syndrome may be clinically “silent,” meaning they do not have symptoms associated with the disorder, including abnormal results on various cardiac tests.
Prevention of WPW syndrome
There is no specific prevention of the disease. If an ECG reveals a patient with SVC syndrome, he should be regularly examined by a cardiologist (even if the symptoms do not bother him). If signs of pathology appear, you need to immediately choose the right treatment.
Persons who are related to a patient with WPW syndrome are recommended to undergo a routine examination to exclude the development of this pathology in themselves. Diagnostics should include: daily monitoring of the electrocardiogram, electrocardiogram, electrophysiological methods.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Disorders with similar symptoms
Symptoms of the following disorders may be similar to those of SVC syndrome. Comparisons may be useful for differential diagnosis.
Lown-Ganong-Levine syndrome (LGL) is a rare congenital heart defect involving abnormalities in the heart's electrical system. The ventricles receive some or all of their electrical impulses from an irregular pathway (alternative pathway). People with LGL syndrome experience a variety of irregular heartbeats, including atrial flutter, atrial fibrillation, and paroxysmal atrial arrhythmias. Symptoms associated with these irregular heartbeats include weakness, fatigue, rapid heartbeat and nausea. The specific location of the alternative pathway in LGL syndrome is not known.
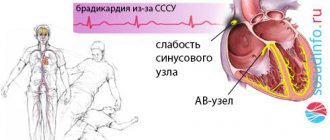
Sick sinus syndrome (SSNS) is a rare heart condition characterized by an irregular heart rhythm (arrhythmia). Patients experience an extremely slow heartbeat (bradycardia) and a fast heartbeat (tachycardia). Additional heart rhythm disturbances may occur, including gradual supraventricular tachycardia, atrial flutter, and atrial fibrillation. Palpitations, weakness, fainting and nausea are common symptoms of this syndrome. Most cases of SSS occur in adults aged 50 years and older. SSSS is caused by a malfunction of the heart's natural pacemaker (Kis-Flac node).
Heart rhythm disturbances associated with SVC syndrome (eg, atrial flutter, supraventricular tachycardia) may occur as separate primary findings or as secondary to structural heart disease. Such alternative causes of cardiac arrhythmia should be distinguished from SVC syndrome.
Treatment of SVC syndrome
Treatment for Wolff-Parkinson-White syndrome may include observation without special intervention (monitoring), the use of various medications, and a surgical procedure known as catheter (radiofrequency) ablation.
Specific therapeutic procedures and interventions may vary depending on many factors, such as:
- type of arrhythmia;
- frequency;
- type and severity of associated symptoms;
- risk of cardiac arrest;
- the person’s age and general health;
- and/or etc. factors.
Decisions regarding the use of specific interventions should be made by physicians and other members of the health care team in careful consultation with the patient, based on:
- features of his case;
- careful discussion of potential benefits and risks;
- patient preferences;
- other relevant factors.
Some asymptomatic patients may not require therapy. Regular follow-up visits are required to monitor heart function.
Various medications are used to control episodes of arrhythmias in some patients with WPW syndrome. Such drugs, known as antiarrhythmics , include:
- Adenosine;
- Procainamide;
- Sotalol;
- Flecainide;
- Ibutilide;
- Amiodarone.
Calcium channel blockers such as verapamil may also be used. Some medications, such as verapamil, may increase the risk of ventricular fibrillation and should be used with caution.
The cardiotonic and antiarrhythmic drug, Digoxin, is contraindicated in adults with SVC syndrome. However, the drug is sometimes used for the prophylactic treatment of children with SVC syndrome who do not have ventricular flutter.
In some cases, medications may not be enough to control episodes of abnormal heartbeats, or individuals may not tolerate medications. In such cases, a surgical procedure known as catheter ablation . This procedure may also be used in patients at high risk for cardiac arrest and sudden death, including some asymptomatic patients.
During catheter ablation, a small, thin tube (catheter) is inserted into the heart and directed toward the abnormal pathway, where high-frequency electrical energy is used to destroy (ablate) the tissue forming the abnormal pathway. This form of therapy has an extremely high success rate and can end the need for drug treatment for many patients.
In the past, open heart surgery was used to treat patients with SVC syndrome. Because of the success of a less invasive procedure, catheter (radiofrequency) ablation, open-heart surgery is rarely performed on patients with this disease.
Forecast
Once WPW syndrome is identified and properly treated, the prognosis is favorable.
Asymptomatic patients with only ventricular pre-excitation on the ECG usually have a very good prognosis. Many develop symptomatic arrhythmia over time, which can be prevented with prophylactic EPS and radiofrequency catheter ablation. Patients with a family history of sudden cardiac death (SCD) or significant symptoms of tachyarrhythmia or cardiac arrest have a worse prognosis. However, after definitive therapy, including curative ablation, the prognosis becomes good again.
Diagnosis of WPW syndrome
Diagnosis of SVC syndrome in children and adults includes a comprehensive clinical and instrumental examination. Conducted:
- Registration of ECG in 12 leads;
- Holter ECG monitoring. Electrodes are attached to the heart area and lead to a portable recorder. The patient walks with them for one day or more. At the same time, he leads a normal life, records all his actions and sensations in a diary;
- Transthoracic echocardiography. A modern method for non-invasive cardiac imaging using reflected ultrasound signals. Allows you to evaluate the morphological and functional structures of the organ;
- Transesophageal pacing. Includes insertion of an electrode into the esophagus, delivery of stimulating electrical impulses, determination of stimulation threshold values, interpretation of ECG information readings;
- Endocardial electrophysiological study of the heart. Aimed at recording and monitoring various indicators of heart function using recording equipment and special sensors. Makes it possible to accurately determine the number and location of additional pathways (Ken's bundles), verify the clinical form of the disease and evaluate the effectiveness of drug therapy or previously performed radiofrequency catheter ablation;
- Ultrasound diagnostics. Allows you to identify concomitant pathologies, heart defects, cardiomyopathy.
Electrocardiographic signs of SVC heart syndrome include:
- shortened PQ interval (does not exceed 0.12 s);
- delta wave;
- deformed confluent QRS complex.
When making a diagnosis, a differential diagnosis of SVC syndrome with bundle branch blocks is required.