Cardiac tamponade is a syndrome in which there is a sharp dysfunction of the heart and a disturbance of general hemodynamics, provoked by the accumulation of transudate, gas or blood in the pericardial sac and a sharp change in intrapericardial pressure. This syndrome is often caused by diseases and injuries of the pericardium and heart: pericarditis, myocardial infarction, tumors and injuries of the chest and heart.
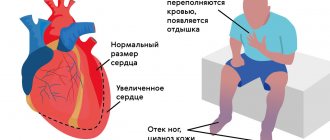
Compression of the cavities of the heart leads to difficulty in contracting the chambers of the heart, diastolic filling of the ventricles and a significant decrease in cardiac output. These pathological changes can cause the development of severe disturbances in general hemodynamics, microcirculation in organs and tissues and severe metabolic disorders that provoke increasing heart failure, shock and complete cardiac arrest.
Cardiac tamponade can be acute or chronic. With the rapid development of this syndrome, its clinical picture develops rapidly, and the outcome is unpredictable.
Causes
Most often, cardiac tamponade is caused by the following factors:
- hemopericarditis due to damage to the integrity of the sternum and heart;
- rupture of dissecting aortic aneurysm;
- heart rupture due to myocardial infarction;
- hemorrhages during cardiac surgery;
- long-term course of chronic diseases (pericarditis, hemopericarditis, lymphoma, myxedema, systemic lupus erythematosus, cancer of the breast, lungs, etc.);
- renal failure developing during hemodialysis;
- taking anticoagulants;
- irradiation, etc.
Treatment
Exudative pericarditis with cardiac tamponade is treated in a hospital. It is advisable to take into account the nature of the disease. Non-steroidal anti-inflammatory drugs prescribed in moderate dosages are an effective treatment. This treatment is also carried out for dry pericarditis. Glucocorticosteroids are also sometimes used. Prednisolone is effective in a dose of up to 60 mg/day, it is taken for 5 to 7 days, then the dose is slowly reduced. Thanks to this drug, the effusion quickly resolves. If during 2 weeks of treatment with glucocorticosteroids (GC) there is no expected effect, a large amount of effusion is present, then a pericardial puncture is performed with the introduction of GC into the cavity of the cardiac sac. The management of the patient also depends on the volume of fluid in the pericardial cavity. If the amount of fluid is small, no therapy is required.
To improve hemodynamics in case of hypotension, liquid is administered - plasma, colloidal or saline solutions in an amount of 400-500 ml intravenously. The effectiveness of these measures is monitored by increasing systolic pressure and systolic ejection. Whatever type of cardiac tamponade is detected, it is necessary to puncture the pericardium in a timely manner. Often this is what helps to significantly improve the patient’s condition.
Signs and symptoms
The severity of clinical manifestations of cardiac tamponade depends on the decrease in cardiac output, pumping function of the heart and the value of pericardial pressure.
The patient has complaints about:
- the appearance of discomfort in the chest;
- increasing shortness of breath;
- shallow breathing;
- anxiety and fear of death;
- increasing weakness;
- dizziness and lightheadedness;
- the appearance of cold sweat and pale skin;
- increased heart rate.
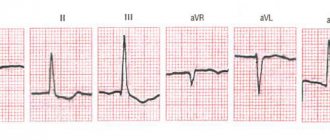
When tamponade occurs as a result of a clearly defined cause (heart injury, etc.), the patient develops the classic Beck triad:
- a sharp drop in blood pressure;
- decreased venous pressure;
- low mobility of the heart, manifested by dull tones.
In most cases, the development of the clinical picture of cardiac tamponade occurs progressively and resembles in its course the symptoms of heart failure:
- shortness of breath, which increases with physical activity or in a horizontal position and forces the patient to take a semi-sitting or sitting position;
- loss of appetite;
- increasing weakness;
- pain in the right hypochondrium;
- swelling of the jugular veins;
- cyanosis;
- increase in liver size;
- an increase in the size of the abdomen due to the accumulation of fluid in the abdominal cavity.
With prolonged stagnation in the systemic circulation, a patient with chronic cardiac tamponade may develop shock.
Etiology
The causes of cardiac tamponade can be:
- tuberculosis
- acute pericarditis (viral or idiopathic)
- influence of radiation
- malignant tumors
- systemic connective tissue diseases (SLE, rheumatoid arthritis)
- injury
- Dressler syndrome
- postpericardiotomy syndrome
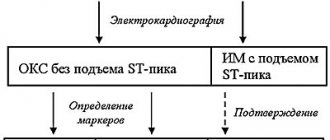
Any disease that affects the pericardium can lead to the accumulation of fluid in its cavity. Acute cardiac tamponade can occur as a result of trauma, including iatrogenic injury during pacemaker installation, aortic rupture during dissection of its aneurysm, or cardiac rupture during myocardial infarction (MI). Subacute cardiac tamponade, as a rule, appears as a consequence of pericarditis (idiopathic or viral), with uremia or a tumor in the pericardium. In most cases, doctors cannot determine the cause of exudative pericarditis, even when surgery is performed.
Emergency care and treatment
Cardiac tamponade is a life-threatening condition in which urgent pericardiocentesis or surgical intervention is indicated for emergency evacuation of transudate from the pericardial sac. In cases of tamponade caused by trauma or postoperative complications, the decision is always made to perform pericardiotomy or subtotal pericardiectomy.
Pericardial puncture is performed under constant monitoring of echocardiography or radiography and monitoring of blood pressure, heart rate and central venous pressure. Local anesthesia is used to numb this procedure. The resulting fluid is sent for bacteriological and cytological examination, and antibacterial, hormonal or sclerosing drugs can be injected into the pericardial sac (depending on the indications).
If necessary, a special catheter can be installed in the pericardial cavity to ensure normal outflow of transudate that continues to accumulate. At the next stage, the patient receives maintenance infusion therapy with nootropic drugs or plasma substitutes and treatment of the disease that provoked cardiac tamponade.
If there is a high risk of recurrent tamponade, pericardiotomy or subtotal pericardiectomy is performed. Also, these emergency surgical interventions are performed when there is compression of the heart caused by rupture of the myocardium or aorta. During pericardiotomy, the surgeon makes a hole in the pericardial wall (pericardial window), which ensures the outflow of transudate and allows inspection of its internal surface to identify foci of hemorrhage or tumor.
When performing a subtotal pericardectomy, which is performed for scar changes, calcification of the pericardium and chronic progressive exudative pericarditis, the pericardium is resected and only a small area of the pericardium adjacent to the posterior surface of the heart is left. After removal of the scarred pericardium, the heart is covered with pleural sacs or mediastinal tissue.
Pathogenesis
According to the norm, between the layers of the pericardium there can be from 20 to 50 ml of fluid, which makes it easier for them to slide relative to each other. This liquid corresponds to blood plasma in its electrolyte and protein composition. If there is more than 120 ml of fluid there, this increases intrapericardial pressure, reduces cardiac output and provokes arterial hypotension.
Clinical manifestations correlate with the rate of fluid accumulation, its quantity, and characteristics of the pericardium. Symptoms of cardiac tamponade occur if fluid quickly accumulates and reaches an amount of 200 ml. If the rate of accumulation is slow, then symptoms may not appear, even if the fluid is already 1-2 liters. Increased intrapericardial pressure with fluid accumulation up to 5-15 mm Hg. is considered moderate, and more than this amount is considered pronounced. Diastolic filling of the ventricle due to increased pressure inside the pericardium is accompanied by an increase in pressure in the chambers of the heart and pulmonary artery, a decrease in stroke volume of the heart and hypertension.
Symptoms of cardiac tamponade and first aid
Contents
hide
1 Symptoms of cardiac tamponade and first aid
2 Cardiac tamponade
3 Symptoms of cardiac tamponade
4 First aid for cardiac tamponade 4.1 Related posts:
The symptoms of cardiac tamponade are caused by the accumulation of fluid in the pericardium. This is a very serious disease that threatens human life. However, timely diagnosis of cardiac tamponade and taking appropriate measures will prevent cardiac arrest and death. Therefore, knowledge about it is very important and useful. It is also worth knowing what first aid should be for cardiac tamponade.
Every person's heart is contained within a sac-like membrane called the pericardial sac. Its job is to protect the heart from injury. The pericardial cavity is located between the outer and inner plates of the pericardium. This is where a small amount of serous fluid accumulates. But if it is exceeded, cardiac tamponade occurs. Then the work of this most important organ of every person is disrupted and requires rapid medical intervention.
First aid for cardiac tamponade
Cardiac tamponade is a medical emergency. The patient cannot help himself without a doctor or other medical assistance. Further prognosis and treatment options depend on timely and correct diagnosis. The only effective first aid method for cardiac tamponade is puncture of the pericardial sac and evacuation of fluid. This procedure is called pericardiocentesis and looks like this:
- performed or under the supervision of an experienced physician in a sterile room,
- the puncture is performed under local anesthesia with a special needle,
- once the sac is reached, a catheter is inserted to remove excess fluid or blood,
- The drainage process itself is done in small portions so as not to cause too much disturbance.
- sometimes the catheter is left in place for several days
- The patient is monitored during the procedure.
The exception to allowing a puncture to be performed outside a sterile environment is when the procedure must be performed immediately for life-saving reasons, such as during resuscitation. Each patient undergoing puncture should be monitored by echocardiography to prevent complications. The most serious complications after puncture of the pericardial sac:
- damage to the heart muscle
- coronary vessel damage,
- heart rhythm disturbances ,
- repeated tamponade,
- pneumothorax.
The second method of treating cardiac tamponade is surgery under general anesthesia in the operating room. This is how recurrent tamponade is usually treated. The choice of treatment method depends on the doctor and the patient's condition. Early symptoms of cardiac tamponade allow immediate treatment and restoration of normal heart function.
Vorobyova Marina
Neurologist of the highest qualification category (work experience 14 years), doctor of neurofunctional diagnostics (work experience 12 years); author of scientific publications on vertebroneurology; participant of scientific conferences on neurology and functional diagnostics of all-Russian and international significance.
Symptoms of cardiac tamponade
The condition of impaired cardiac function, that is, tamponade, is defined by cardiologists as a life-threatening condition. Early recognition of the symptoms of this heart disease prevents cardiogenic shock, cardiovascular arrest, and even death. Based on the time of onset of symptoms of cardiac tamponade, two types are distinguished:
- subacute tamponade - symptoms appear no earlier than after a few hours, and sometimes after 4-5 days,
- Acute tamponade - symptoms appear a few minutes after fluid or blood begins to appear in the pericardial cavity.
If fluid or blood collection occurs quickly and rapidly, the heart cannot adapt to these conditions. The faster the fluid accumulates, the faster the so-called circulatory decompensation, usually called circulatory failure, occurs. The main symptoms of cardiac tamponade include:
- shortness of breath, especially severe when lying down,
- fainting or pre-fainting states,
- increased heart rate,
- sudden cough
- tachycardia (cardiac tachycardia)
- dilation of the jugular veins,
- elusive heartbeat, consisting of a decrease in its tone,
- hypotension (low blood pressure),
- cold, pale skin,
- rapid and frequent fatigue,
- the pulse is “strange”, which is definitely lower during inspiration.
Cardiac tamponade should be suspected in people who have suffered a strong blow to the chest area, especially the sternum. Symptoms of tamponade can lead to so-called venous stasis (blood cannot flow to the heart) and a drop in blood pressure, as well as ischemia of other organs. Doctors identify a classic triad of symptoms characteristic of cardiac tamponade, called Beck's triad. This consists of:
- hypotension, i.e. systolic blood pressure up to 90 mm Hg.
- quiet (muffled) heart sounds,
- filling of the jugular veins.
The presence of these three symptoms together clearly indicates cardiac tamponade. In a hospital setting, this is confirmed by the presence of serous fluid or blood in the pericardial cavity.
About
Cardiac tamponade
Cardiac tamponade indicates that excessive serous fluid or blood is entering the pericardial cavity. The fluid that normally resides in the pericardial sac prevents the heart from rubbing against the sac. Too much fluid or blood causes increased pericardial pressure and pressure from the pericardial sac on the right side of the heart. This is a very dangerous health situation because the flow of blood to and from the heart is disrupted. The norm is up to 30 ml of fluid in the pericardial cavity. As a result of the disease, up to 2 liters of fluid can accumulate. And this is already a serious threat to life. The fluid accumulates gradually or appears suddenly. The gradual accumulation of fluid does not always cause alarming symptoms. It is more dangerous to quickly fill the pericardial cavity. Symptoms of cardiac tamponade may occur with the rapid accumulation of as little as 50 to 100 mL of fluid. The heart cannot adapt to new conditions, such as increased blood pressure and blood pressure, and this disrupts its functioning. Cardiac tamponade is caused by:
- chest injuries,
- pericarditis (bacterial and viral),
- damage to the heart during a heart attack ,
- crayfish,
- acute liver and kidney failure,
- complications after cardiac surgery,
- rupture of an aortic aneurysm.
About