Hypertension is a serious disease that leads to serious complications of the cardiovascular system. Since it often affects the working population, various classifications have been developed, including special scales for assessing cardiovascular risk. In this article we will tell you what hypertension is, stage 2, risk 3.
Causes of stage 2 hypertension
Narrowing of the lumens of blood vessels and slowing of blood flow are traditionally diagnosed in middle-aged and elderly people. But it is not only the passing years that cause the violation. Hypertension occurs against the background of factors contributing to the development of the disease. This:
- heredity (the more close relatives suffer from high blood pressure, the higher the likelihood that you will encounter this problem);
- lack of physical activity (physical inactivity “relaxes” the blood vessels, making them inelastic and fragile, worsens cardiac activity);
- bad habits, which include not only smoking and alcohol abuse, but also excessive consumption of salt, which retains fluid in the body;
- atherosclerosis (such a disease can be not only the cause of hypertension, but also its consequence);
- hormonal changes (pregnancy and menopause are periods during which women most often experience symptoms characteristic of arterial hypertension for the first time);
- endocrine diseases;
- kidney and genitourinary diseases;
- osteochondrosis;
- vascular disorders;
- malignant and benign tumors;
- stress of a regular nature.
Obesity is the cause of the development of hypertension (every extra kilogram is a load on the heart, blood vessels, and internal organs)
Symptoms
The main symptomatic manifestations of the disease appear at the beginning of the development of hypertension (at stage 1). Blood pressure periodically rises, headaches, a feeling of nausea, tinnitus and black spots before the eyes appear, problems with sleep begin, and the heartbeat quickens from any exertion.
But if at stage 1 of the disease the upper pressure only sometimes rises to 140-159 mm Hg, and the lower to 90-99 mm Hg, then stage 2 hypertension is a pressure of 160-180/100-110 mm Hg .st. It becomes almost permanent, causing a person a lot of inconvenience and depriving him of the opportunity to live a full life without the help of medications. At the second stage, new symptoms are added to the general symptoms characteristic of phase 1 hypertension. This:
What is a hypertensive crisis
- feeling of chronic fatigue, including immediately after waking up;
- low threshold of emotional excitability;
- nausea, during a crisis turning into vomiting;
- pulsation in the head area;
- heart failure;
- increased sweating;
- hyperemia of the skin of the face and upper body;
- deterioration of vision, development of fundus pathologies;
- swelling of the face, worsening in the morning;
- chills, numbness of fingers and upper extremities;
- albumin proteins appear in the urine (microalbuminuria);
- arterioles narrow;
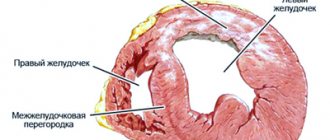
- the walls of the ventricle become denser, trying to resist blood flow;
- if the disease has caused pathological changes in the functioning of the kidneys, symptoms such as uncontrollable urination at night, swelling of the feet after sleep, cloudy urine or a pink color appear.
At this stage, hypertensive crises occur, during which the pressure rises by 59 units. Attacks last for several hours and threaten serious consequences in the form of a heart attack, cerebral, pulmonary edema or stroke. Signs of damage to target organs (brain, heart, eyes, kidneys) become obvious. Treatment should begin immediately after the first manifestations of the disease are detected. This will help cope with further destruction of organs and systems and improve the patient’s well-being.
Important! The diagnosis of arterial hypertension of the 2nd stage can also be made in patients whose blood pressure falls within the pressure range at stage 1 of the disease. Doctors focus not only on the tonometer readings, but also on the degree of target organ damage. If the brain, heart, eye vessels, kidneys are damaged, the disease progresses to stage 2.
Arterial hypertension 2 degrees: features of the course, causes of development and characteristic signs
Hypertension is a severe pathological condition of blood vessels and the heart, when elevated blood pressure cannot be stabilized with medications. Arterial hypertension of the 2nd degree - stable high blood pressure in the range of 160-180 mm Hg.
The risk of complications is high. The phenomenon is life-threatening and can lead to myocardial necrosis, heart attack, hemorrhagic stroke in case of serious damage to the vascular wall, inability of the tone to correspond to the level of blood supply.
Risk factors
There are 4 degrees of hypertension, taking into account possible complications that pose a threat to the health and life of patients. The stage is determined taking into account:
- age of patients;
- stress on the heart;
- lifestyle;
- hereditary history;
- the presence of characteristic signs, obesity, bad habits.
8
24/7
With arterial hypertension, the risk of stage 2 development in men who abuse alcohol (smoking) and neglect physical activity is 3 times higher than in women. The main factors for the development of type 2 hypertension:
- elderly age;
- left ventricular myocarditis;
- modification of the heart wall, brain against the background of constantly high blood pressure;
- myocardial hypertrophy;
- pathology of muscle tissue;
- circulatory disorders;
- tissue necrosis;
- proteinuria.
In case of arterial hypertension of the 2nd degree, the target organs are:
- eyes;
- kidneys;
- heart;
- vessels;
- brain.
Pressure indicators increase by 15-20%. Additional provoking factors:
- age - men over 55 years old, women over 65 years old;
- obesity;
- physical inactivity;
- passive lifestyle;
- smoking;
- high levels of cholesterol in the blood, above 6.5 mmol/l;
- the appearance of atherosclerotic plaques in small vessels;
- failure of the kidney filters;
- kidney dysfunction;
- violation of coronary circulation;
- sustained cardiac ischemia.
With stage 2 arterial hypertension, the risk of developing regressive changes in the heart is 2 times higher than at stage 1.
Provoking factors for stage 2 arterial hypertension are not absolute parameters. They only make it possible to assume the likelihood of possible complications developing.
It is no longer possible to change the diagnosis. However, timely treatment and adherence to preventive measures can minimize complications and progression of the underlying disease.
Types of pathology
Types of arterial hypertension:
- Renovascular. Provoking factors are vascular atherosclerosis, kidney tumors, vasculitis.
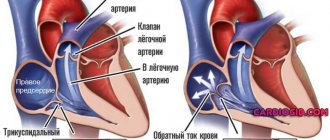
- Pulmonary essential hypertension is a rare phenomenon, but poses a health threat. The reason is slow blood flow, increased vascular resistance in the lungs.
- Labile arterial pathology is a form of hypertension in which blood pressure levels periodically normalize. The condition is not considered pathological.
- Malignant (at a blood pressure level of 220/130 mm Hg) - the optic disc swells, the fundus of the eye changes. Only timely detection guarantees a favorable outcome of therapy.
Hypertension can be benign or malignant with rapid progression of symptoms and development of complications in the nervous and cardiovascular systems.
8
24/7
Causes
Stage 2 hypertension is more often diagnosed in older people. With age, blood vessels lose their elasticity and atherosclerotic plaques form in them. The muscle tissue of the heart undergoes pathological changes. Main reasons:
- hereditary factor, when blood relatives suffered from high blood pressure;
- passive lifestyle;
- complicated course of pregnancy, changes in hormonal levels;
- frequent stress, psychosis;
- complication of primary mild form of hypertension;
- diseases of the urinary system;
- non-compliance with a balanced diet, consumption of foods high in cholesterol;
- development of a tumor of any origin;
- failure of the kidneys, slowing down the removal of excess fluid and salts from the body.
Patients with minor pressure surges on the tonometer do not always turn to doctors at an early stage. The discomfort is minor, the body gradually adapts and gets used to new stress. But constantly high levels of pressure suppress many vital systems. Sooner or later, pulmonary and cerebral edema, stroke, myocardial infarction, and hypertensive crisis may develop.
Symptoms
Manifestations of arterial hypertension of the 2nd degree disturb patients from their usual rhythm of life. At first, vague, not bright, periodic symptoms appear:
- swelling of the hands, eyelids, face;
- the appearance of a capillary network on the skin;
- weakness, weakness;
- throbbing pain in the back of the head, temples;
- darkening, flickering of spots, black dots before the eyes;
- redness of the eyes;
- decreased vision;
- dizziness;
- emotional overexcitation.
During diagnosis, thickening of the walls of the heart and left ventricle is observed. Patients develop problems with urination.
Diagnostics
Physical and instrumental examination methods help to identify stage 2 arterial hypertension. The following are taken into account:
- symptoms;
- patient's well-being;
- blood pressure indicators during 2-week monitoring - indicators are measured 2 times a day (morning, evening).
Physical examination methods:
- listening to the cavity of the lung and heart with a stethoscope;
- visual assessment of the skin;
- pressure measurements.
Instrumental methods:
- Ultrasound of the pancreas, liver, kidneys, endocrine glands to assess the condition of organs and identify possible complications;
- EchoCG for visual examination, determination of left ventricular hypertrophy, assessment of the level of cardiac decompensation;
- electrocardiogram to determine the electrical activity of the heart muscles;
- blood and urine tests;
- Doppler examination to detect renal artery stenosis.
Arterial hypertension of the 2nd degree quickly progresses in the case of narrowing of one of the vessels. It develops at lightning speed - renin aldosterone is activated as the body's response to pathology.
8
24/7
Treatment at different stages
First of all, it is important for patients:
- reconsider your lifestyle;
- limit intake of table salt (liquid);
- reduce the daily caloric content of foods in case of obesity;
- stop smoking;
- dose the work and rest schedule;
- take courses of physiotherapy, exercise therapy;
- regulate physical activity;
- walk more in the fresh air.
Treatment to reduce high blood pressure is medication. Main drugs:
- beta blockers (Atenolol, Metoprolol, Acebutolol, Oxprenolol, Timolol, Bisoprolol, Sotalol) affect the cardiovascular system, unload the heart, slow down the rate of muscle contraction;
- ARB inhibitors (Valsartan, Candesartan, Irbesartan, Eprosartan) suppress angiotensin receptors, regulate the condition of the myocardium and blood vessels;
- ACE - angiotensin-converting enzyme inhibitors (Fosinopril, Cilazapril, Enalapril, Captopril, Trandolapril, Lisinopril) relieve tension in the blood vessels, reduce the rate of production of the hormone that constricts them;
- Renin inhibitors have nephroprotective and cardioprotective effects and reduce renin activity in the blood.
- diuretics (Thiazide) accelerate the removal of excess fluid from the body;
- calcium channel blockers (Verapamil, Diltiazem, Lacidipine, Amlodipine, Nifedipine).
Special attention is paid to diet. Patients with stage 2 hypertension should avoid:
- fatty fish;
- meat;
- confectionery products;
- spicy and spicy dishes.
Must be included in diet
- dried fruits;
- nuts;
- garlic;
- milk and vegetable soups.
Folk herbs with diuretic properties will help with isolated, periodic surges in blood pressure:
- horsetail;
- valerian officinalis;
- swamp cudweed;
- motherwort;
- Potentilla gossamer;
- buckthorn bark;
- yarrow;
- pharmaceutical camomile.
Forecast
Stage 2 arterial hypertension is considered an incurable condition. The prognosis is favorable if patients:
- maintain blood pressure levels within normal limits;
- lead a healthy lifestyle;
- give up bad habits;
- follow a diet.
Otherwise, hypertension progresses quickly and leads to complications:
- myocardial necrosis;
- hemorrhagic stroke;
- decompensation of vascular insufficiency, heart failure.
Mortality is high in cardiovascular pathologies and persistently high blood pressure levels.
The prognosis is disappointing for patients who neglect the recommendations of doctors, do not control blood pressure readings, and ignore complications. In case of heart failure or stroke, the probability of sudden death is 70%.
In stage 2 arterial hypertension, the risk of stage 3 development is high with severe damage to target organs. At stage 2 arterial hypertension, the risk of stage 4 development is 45-60%.
Prevention
Avoiding the development of arterial hypertension from stage 2 to stage 3 means:
- eat rationally;
- fight excess weight;
- limit salt intake;
- dose physical activity;
- avoid stress and unfavorable psychological conditions in the family;
- keep blood pressure levels under control;
- stop bad habits, addiction to drugs, smoking, alcohol, overeating.
Arterial hypertension of the 2nd degree - a steady increase in blood pressure: diastolic over 89 mm Hg, systolic over 139 mm Hg. Blood pressure can increase in every person, regardless of age and lifestyle. But more often, patients with a hereditary factor suffer from hypertension and even an increase of 9-10 mm Hg. may already indicate the development of serious pathologies.
The disease cannot be cured completely, although it is possible to regulate blood pressure levels and keep them under control. If you identify arterial hypertension at an early stage and undergo a thorough examination, you can achieve stable remission, thereby improving the quality of life.
8
24/7
Consequences of violation
Why is this phase of hypertension dangerous? There are several complications, and complications that pose a real threat to life and health.
- If stage 2 arterial hypertension is diagnosed, the risk of stage 3 and stage 4 of the disease becomes as high as possible.
- The likelihood of developing a hypertensive crisis, which can result in a heart attack and stroke, also increases.
- The heart experiences constant stress, which leads to heart failure and other disorders.
- Almost every hypertensive patient whose disease has progressed to the second stage is diagnosed with atherosclerosis, in which the vessels are clogged with plaques that impede blood flow.
- The mechanism for the development of kidney and liver pathologies associated with poor vascular patency is triggered.
A common complication of hypertension is damage to the blood vessels of the eyes, which lead to deterioration of vision.
Stage 2 hypertension can develop over years (benign form) or rapidly progress to the next stage (malignant form). In the second case, people sometimes do not have time to take care of their health and stop the process, which leads to irreparable consequences, including death.
Symptoms
Arterial hypertension has no specific symptoms; most often patients complain of:
- headache;
- dizziness;
- nausea;
- weakness;
- drowsiness;
- increased heart rate;
- extraneous noise in the ears;
- reduced performance.
However, most often the increase in pressure does not cause any symptoms and the patient finds out about arterial hypertension by chance. For example, during medical examinations or during medical examinations. In stages 2 and 3 of hypertension, the symptoms of the affected organs come to the fore.
| Target organs | Symptoms |
| Heart |
|
| Vessels |
|
| Kidneys |
|
| Retinal vessels |
|
| Brain |
|
Diagnostic measures
A treatment regimen is drawn up by a cardiologist after a comprehensive examination, identifying pathologies in target organs, determining the form of the disease and the causes that led to the disorder. But the main sign remains the indicators of systolic and diastolic pressure. To determine these data, studies are carried out on:
- pressure stability throughout the day;
- degree of risk of developing complications of the disease;
- exclusion or confirmation of increased blood pressure as a complication of other ailments;
- identification of factors contributing to hypertension;
- identification of pathological changes in other organs and systems.
The first thing the doctor does is measure your blood pressure and give recommendations for self-diagnosis at home. For hypertension, blood pressure is measured 2-3 times a day for a week, recording all data in a special diary. This allows the doctor to make an accurate diagnosis and take into account the peculiarities of the course of the disease. The physical examination is complemented by the collection of data obtained from a patient interview.
Additionally, daily blood pressure monitoring is prescribed using a special device in a hospital setting. An obligatory part of the diagnosis is an electrocardiogram and ultrasound of the heart. The techniques help to see any type of tacharrhythmia and assess the thickness of the ventricular walls. If abnormalities in the functioning of the internal organs are suspected, a magnetic resonance therapy study is carried out, and ultrasonography is prescribed to determine the size of the kidneys.
Diagnostics
Diagnosis of arterial hypertension includes several stages:
- Collection of complaints and medical history.
- Repeated blood pressure measurements at least 2 times during different visits to the doctor.
- Physical examination.
- Laboratory and instrumental examination.
At the first stage, the doctor will find out what symptoms are bothering you and how long ago they appeared. Find out whether you smoke, whether you drink alcohol and in what doses, and whether your relatives have cardiovascular diseases.
Keep a blood pressure diary for 10 days. To do this, it is necessary to measure blood pressure at least 3 times a day. Show your doctor your notes at your next appointment. He will analyze the results obtained and, based on this, decide on the tactics for further examination and treatment.
Physical examination includes auscultation of the heart, determination of its boundaries, and heart rate. The doctor will definitely check your pulse and its tension. Measure your waist circumference, weigh you, and determine your body mass index.
Laboratory diagnostics:
- general blood and urine analysis;
- level of proteinuria and microscopy of urinary sediment;
- biochemical blood test - sugar, ALT, AST, creatinine, K, Na ions, total cholesterol and lipid profile.
Instrumental diagnostics:
- ECG;
- ECG with stress;
- EchoCG;
- Ultrasound of the brachiocephalic arteries;
- Ultrasound of the kidneys;
- chest x-ray;
- Holter monitoring ECG;
- daily blood pressure monitoring;
- consultation with an ophthalmologist, endocrinologist.
Additional examinations that are not included in the standard may be required, for example, a hormonal mirror. In rare cases, hospitalization in a hospital may be required. This is necessary for a more accurate diagnosis. As a result of examinations, the doctor makes a diagnosis and prescribes treatment.
And also read on our website: Does neck exercises help in the treatment of hypertension? Exercise sets
Features of treatment
Every hypertensive person is concerned with the question of whether arterial hypertension can be cured. Traditional methods are powerless here. Treatment is complex and depends on the form of the disease, the condition of the internal organs and concomitant pathologies. Cardiologists prescribe a number of drugs that complement and enhance each other’s effects in order to bring the tonometer readings closer to 130/80 mmHg. This:
- Angiotensin-converting enzyme inhibitors;
- Beta blockers;
- Angiotensin 2 antagonists;
- Calcium channel blockers;
- Diuretics;
- Antagonists of Renin.
Drugs and their dosage are prescribed strictly individually. This takes into account the patient’s age, weight, medical history and blood tests. It is necessary to strictly adhere to the therapeutic regimen, without independently changing one drug for another, canceling treatment or increasing the number of tablets. When taking many antihypertensive drugs, an addiction syndrome occurs, so abrupt withdrawal can lead to a hypertensive crisis.
Important! The prognosis of therapy is not always favorable. It depends on the characteristics of the course of the disease, concomitant disorders, and the timeliness of treatment started. What are the risks of stage 2 hypertension? Risk 2 is disability.
Prevention
Prevention of hypertension involves lifestyle modification. Its scheme includes:
Increasing physical activity
To maintain health, you need to walk at least 10,000 steps daily at a moderate pace. Or do aerobic exercise for 30-40 minutes 3-4 times a week. Contact a rehabilitation specialist or physiotherapist - they will help you choose a set of physical therapy exercises taking into account your clinical condition.
Diet
The menu for hypertension requires serious revision. Be sure to limit your salt intake to 5 g/day. This means that you will have to give up all industrially produced products: sausages, canned food, smoked meats, salted fish, various snacks, since salt is used as the main preservative in their production.
It is important to eat enough vegetables and fruits, at least 400-500 g per day. Avoid fatty meats and add fish to your diet twice a week.
Weight loss
It has been reliably proven that for every 10 kg of weight lost, the SBP level decreases by 5-10 mmHg.
Rejection of bad habits
You should definitely stop smoking tobacco and drinking alcohol.
Stage 2 hypertension and disability
Manifestations of hypertensive disease are not always completely removable. Especially often, people with a malignant form of the disease face the fact that treatment does not bring the desired effect. In this case, the person loses the ability to work fully and receives the status of a disabled person with a number of restrictions. The patient is prohibited from:
- work in extreme conditions;
- work more than 7 hours a day;
- be at heights and at high temperatures while working;
- experience stress and increased physical activity.
Disability, if the disease does not progress to stages 3 and 4, is temporary and is removed when the patient’s condition improves. If complications do not allow a full recovery, a person can work only in certain conditions that take into account the specifics of the course of the disease, for example, remotely.
Additional recommendations
The risk of relapse of the disease remains high even after recovery. This risk can be minimized by adhering to certain restrictions. The list is small and will be useful not only for hypertensive patients, but also for people who care about their health.
The bathhouse is a taboo for hypertensive patients. A sharp change in temperature can lead to hypertensive crisis and other consequences
Necessary:
- Quit smoking and alcohol, which negatively affect the condition of blood vessels.
- Introduce regular physical activity into your daily routine, as agreed with your doctor.
- Limit salt intake to a minimum.
- Eliminate stressful situations. If this is not possible, it is necessary to take sedatives that calm the nervous system.
- Minimize the amount of salt in your diet. Exceeding the permissible doses of this product leads to fluid retention in the body, which leads to changes in blood pressure and deterioration of the heart and circulatory system.
- Lose weight. Considering that every excess kilogram adds 2 mmHg. to the numbers on the tonometer. This means that losing weight in this case is not a tribute to the fashion for slimness, but taking care of your own health.
- Be sure to take the hypertensive medications prescribed by your doctor. It is important to do this not only during an exacerbation, but also during remission of the disease.
- When creating a menu, you should pay attention to healthy low-calorie foods rich in vitamins, fiber and microelements. The most beneficial for hypertensive patients are: vegetables, fruits, dried fruits, cereals, low-fat dairy and fermented milk products, lean meats and fish. You should avoid fatty meats, butter and margarine, smoked foods, and preserves.
Hypertension is a disease that does not disappear on its own. Only an integrated approach can achieve lasting results and improve the patient’s condition, bringing it closer to normal levels.
Hypertensive crisis
Hypertensive crisis is an unpredictable complication of hypertension. It manifests itself as a rapid increase in blood pressure to high levels, often leading to cardiovascular disasters. Its symptoms:
- pain in the occipital region of the head
- numbness of fingers;
- panic and fear of death;
- pain in the heart area.
And also read on our website: What is nocturnal hypertension?
Symptoms, treatment and prevention of the disease A hypertensive crisis must always be stopped. Patients suffering from hypertension for a long time should be able to cope with it independently.
To do this, you should always have an emergency medicine in your home medicine cabinet, for example:
- Captopril;
- Nifedipine;
- Moxonidine;
- Furosemide.
If a hypertensive crisis is detected for the first time, call an ambulance. Call your doctor immediately if you experience any of the following complications:
- transient ischemic attack;
- stroke;
- acute coronary syndrome;
- preeclampsia and eclampsia in pregnant women.
A hypertensive crisis can lead to cardiovascular disaster. If you can’t stop it on your own, consult a doctor!