- How common is Hodgkin's disease?
- What causes Hodgkin's disease and can it be prevented?
- How is Hodgkin's disease diagnosed?
- How is the stage of Hodgkin's disease determined?
- Treatment of Hodgkin's disease
- What happens after treatment for Hodgkin's disease?
Hodgkin's disease (HD), also called Hodgkin's lymphoma or lymphogranulomatosis, is a type of malignant tumor that develops from lymph tissue, including the lymph nodes and other organs that form part of the body's defense system (spleen, thymus, bone marrow).
Hodgkin's disease was named after Thomas Hodgkin, who first described it in 1832. Since lymphatic tissue is found in many parts of the body, HD can occur almost anywhere. The disease leads to enlargement of the lymph nodes and compression of nearby tissues and organs. Tumor cells can spread through lymphatic or blood vessels to any part of the body.
Forms
The morphological substrate of the tumor is Berezovsky-Stenberg-Reed cells, however, their number in the tumor tissue rarely exceeds 10%. The second variant of cells is Hodgkin cells, which are a provariant of the Berezovsky-Stenberg-Reed cell. Depending on how the tumor tissue looks under a microscope, there are five forms of Hodgkin lymphoma.
- The variant of Hodgkin's disease with lymphocytic predominance accounts for 5-6% of all cases of HL. There are very few Berezovsky-Stenberg-Reed cells.
- The mixed cell variant is diagnosed in three quarters of patients. Berezovsky-Stenberg-Reed cells and Hodgkin cells are found in sufficient numbers.
- Lymphocytic depletion is the most rare morphological variant of the tumor (less than 1%).
- The most common variant of Hodgkin's lymphoma is nodular sclerosis.
- With nodular lymphoid predominance, the lymph node tissue is completely or partially replaced by an infiltrate of a nodular structure, often combined with zones of diffuse growth.
Why does lymphogranulomatosis occur?
The exact causes of the disease have not been established. There are several triggers for Hodgkin's disease:
- genetic predisposition, when the disease is hereditary;
- previously suffered severe infectious diseases;
- spontaneous change in lymphocytes, provoked by exposure to viruses or taking medications that suppress the immune system.
Factors that provoke the disease include:
- the effect of radiation;
- working with harmful substances - pesticides, herbicides, solvents, benzenes;
- living in regions with poor ecology.
Since the exact causes of this type of lymphoma are unknown, there is no special prevention.
Clinical stages
Clinical stage is determined according to the Ann Arbor classification (1971), supplemented by the Cotswold recommendations (1989):
Stage I - damage to one or two groups of lymph nodes (I) or one non-lymphatic organ (or tissue) - (IE);
Stage II - involvement of two or more lymphatic areas on one side of the diaphragm (II) or involvement of one non-lymphatic organ (or tissue) and one (or more) lymphatic areas on one side of the diaphragm (IIE), involvement of the spleen (IIS);
Stage III - involvement of the lymphatic system on both sides of the diaphragm (III), which may be combined with localized involvement of one non-lymphatic organ or tissue (IIIE), or involvement of the spleen (IIIS), or involvement of both (IIIES);
Stage IV - widespread damage to one or more non-lymphatic organs (lungs, pleura, pericardium, bone marrow, bones, etc.) with or without involvement of the lymph nodes.
In Fig. Figure 1 shows the affected areas in Hodgkin lymphoma.
Rice. 1. Affected areas in Hodgkin's disease
Causes of the disease
Hodgkin's lymphoma is a cancer that affects the lymphatic system.
This disease is also called lymphogranulomatosis. It has a certain feature that distinguishes it from non-Hodgkin lymphomas; it is characterized by the formation of special Reed-Sternberg cancer cells. This diagnosis is more often given to men than to women. This cancer occurs very rarely in children under 10 years of age. The causes of Hodgkin lymphoma are still unknown. Experts are confident that pathological viruses and bacteria can provoke its occurrence:
- Epstein-Barr virus;
- Mycobacterium tuberculosis;
- HIV;
- herpes virus type 6.
Scientists suggest that the tendency to develop the disease is inherited. It has also been established that the likelihood of Hodgkin lymphoma increases:
- in the presence of immunodeficiency syndromes;
- for autoimmune diseases (multiple sclerosis, rheumatoid arthritis);
- after transplantation;
- after taking phenytoin, radiation or chemotherapy;
- as a result of working in the woodworking industry.
Symptoms
The first and most characteristic symptom of Hodgkin lymphoma is enlarged lymph nodes. Lymph nodes are usually painless, dense, mobile, often in the form of conglomerates (reminiscent of a “bag of potatoes”). The most common enlarged lymph nodes can be seen in the neck (Fig. 2), in the armpits, near the collarbone, in the groin, or in several places at the same time. Lymph nodes can also enlarge where they cannot be felt, for example, in the chest, abdomen, or pelvis.
Rice. 2. Damage to the cervical lymph nodes in Hodgkin lymphoma.
If enlarged lymph nodes are located in the chest (mediastinum) (Fig. 3), coughing attacks or shortness of breath may occur.
Sometimes the liver and spleen become enlarged (in medical practice this is called hepatomegaly and splenomegaly).
Central nervous system involvement can develop in advanced cases of Hodgkin lymphoma.
Bone damage: the vertebrae and hip joints are most often affected.
Bone marrow involvement occurs in 5-10% of cases of Hodgkin's disease.
Children may experience general symptoms of the disease : increased body temperature above 38°C for three days without signs of infectious diseases, severe night sweats, weight loss of more than 10% over the past 6 months for no apparent reason, fatigue, weakness, skin itching all over the body. In medical practice, these symptoms are called B-symptoms and are designated by the letter “B”; they are used in determining the stage of the disease.
For staging, it is necessary to take into account the biological activity of the disease .
It is determined on the basis of two or more of the following indicators: ESR ≥ 30 mm/hour; fibrinogen ≥ 4 g/l; albumin ≤ 40%; SRB (++ and more); leukocyte count ≥ 12x10 /l; alpha-2-globulin ≥ 12%
Why is it worth coming to Germany for treatment of Hodgkin's Lymphoma?
In addition to the general reasons and advantages of treatment in Germany, which we described in this section of the site, in Germany doctors never refuse to treat patients who have already come to their clinic for treatment.
If the doctors agreed to accept you for treatment, then they will not send anyone home, but will fight until they defeat the disease. When deciding on the need to use a particular technique, German doctors proceed from the patient’s condition and the appropriateness of treatment, but never refuse further treatment only because of the patient’s age or condition, as is often the case in post-Soviet countries. If it becomes obvious that it is no longer possible to stop the progression of the disease, the patient is offered a well-thought-out palliative program to alleviate suffering and relieve pain as much as possible. Please follow and like us:
Diagnostics
If, after a thorough examination, the pediatrician finds signs of Hodgkin's lymphoma, then he gives a referral to a specialized hospital (clinic of pediatric oncology and hematology).
The following are carried out in the hospital:
- Examination of the affected tissue . The main method of diagnosing lymphoma is a biopsy (surgical removal of the affected lymph node or tissue and examination of the material under a microscope). Based on the results of examining a tissue sample, it is possible to accurately determine whether a child has Hodgkin lymphoma, and if so, what type of lymphoma.
- Analysis of the prevalence of disease in the body. After making a diagnosis, it is necessary to find out how far the disease has spread throughout the body and what organs it has affected. For this purpose, PET-CT with glucose is performed. According to indications, a bone marrow examination is performed (trephine biopsy of the bone marrow in patients with stages IB, IIB-IV), osteoscintigraphy, and MRI for bone lesions.
- If there is a history of cardiovascular pathology, a heart murmur is listened to, and LVEF (left ventricular ejection function) is performed.
Rice. 3. Damage to the intrathoracic lymph nodes in Hodgkin lymphoma
What is lymphoma?
Lymphoma is a lesion of the immune system and internal organs, in which altered cells accumulate, disrupting tissue function.
The tumor develops in the lymphatic system, which helps us fight infections and other diseases. The lymph circulating in it washes all the cells of the body and delivers the necessary substances to them, taking away waste. In the lymph nodes located throughout its network, dangerous substances are neutralized and removed from the body. The lymphatic system complements the circulatory system and helps fluids move throughout the body. Unlike blood, the speed of which is set by the “pump” - the heart, lymph slowly circulates on its own.
Modern approaches to treatment
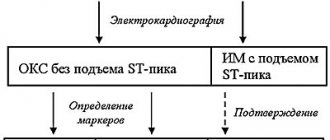
Chemotherapy occupies the main place in the treatment of Hodgkin lymphoma.
Chemotherapy is treatment with drugs (cytostatics) that block the division or kill tumor cells. The maximum effect can be achieved using combinations of cytostatics (polychemotherapy - PCT), which have different effects on cells.
Polychemotherapy is carried out in accordance with the risk group to which the patient was assigned during primary staging, in a specialized hospital.
Fig.4
The first cycle of chemotherapy begins immediately after the diagnosis is confirmed and the stage is established; in the case of surgical treatment, polychemotherapy begins 5 days after the operation.
After chemotherapy, radiation therapy (irradiation) is given to the affected areas. Radiation therapy should begin within 14 days of the end of chemotherapy if blood counts are normal.
In Russia today there are two main treatment programs for Hodgkin lymphoma: DAL-HD and SPbHL. Both protocols include polychemotherapy and final radiation therapy. The number of cycles of PCT depends on the stage of the disease and on the choice of therapeutic group in which the patient is treated. Patients usually receive the following program: with favorable options (1st risk group) - 2 cycles of chemotherapy, with an intermediate prognosis (2nd risk group) - 4 cycles of chemotherapy, with unfavorable options (3rd risk group) - 6 cycles of chemotherapy . The division of patients into risk groups has some differences depending on the protocol used.
DAL-HD uses OPPA/OEPA and COPP schemes. The SPbLH protocol contains VBVP and ABVD schemes.
Forecast
Lymphogranulomatosis, which is the most common of the lymphomas, has the most favorable prognosis. When Hodgkin's lymphoma is detected at the first or second stage, clinical recovery after treatment occurs in 70% of patients.
The progression of the disease reduces the rate of favorable outcome. Stage 4 of the disease makes the prognosis unfavorable. However, as always when making predictions in medicine, we must not forget that we are talking about an organism that is unique in its individuality. A simple transfer of statistical indicators cannot be truly decisive in the outcome of the disease.
Non-measurable factors such as faith, hope, perseverance influence the body’s resistance and produce favorable results, increasing the effectiveness of treatment.
Radiation therapy
The final stage of treatment for Hodgkin lymphoma is irradiation of all affected areas of the lymph nodes. As a rule, radiation therapy begins 2 weeks after the end of drug therapy when blood counts are normalized.
The radiation dose depends on the completeness of remission after drug therapy: upon achieving complete remission (disappearance of all clinical and radiological signs of the disease) in the lymphatic zone, according to PET-CT data, the radiation dose is 20 Gy. If the size of the tumor after polychemotherapy has decreased by 75% or more from the original tumor and/or there is a decrease in radiopharmaceutical hyperfixation according to PET-CT to 2-3 according to Deauville, then the radiation dose is 25 Gy. If tumor formations are reduced by less than 75% and/or radiopharmaceutical hyperfixation persists according to PET-CT 4-5 according to Deauville, the radiation dose is increased to 30 Gy.
Fig. 5 Radiation treatment plan. Patient I., 4 years 6 months. Hodgkin's lymphoma stage II. with damage to the cervical, supraclavicular, subclavian lymph nodes on the left, the thymus gland, and the nasopharynx. Condition after 4 courses of PCT, remission. Irradiation of the cervical-supraclavicular lymph nodes on the left with a consolidating purpose, SOD 20 Gy.
Fig.6 Patient M., 11 years old. Hodgkin's lymphoma stage II. with damage to the soft tissues of the neck, lymph nodes of the neck. Condition after 2 courses of chemotherapy. According to the control PET/CT data, no metabolically significant lesions were identified, remission. Conducting radiation therapy of the primary involved areas with a total focal dose of 20.0 Gy for the purpose of consolidation.
Is lymphoma cancer?
Official medicine in Russia and some other countries refers to cancer as malignant tumors - life-threatening neoplasms that develop in epithelial cells contained in the skin or mucous membranes and lining the internal surface of organs.
Lymphoma is not a cancer, but an oncological disease. It is formed from lymphocytes, and its cells are also able to divide uncontrollably, accumulate in tissues, disrupting their work, and create additional foci of disease in various parts of the body.
Criteria for assessing the completeness of remission
Criteria for assessing remission are needed by the doctor to determine the need to continue treatment or intensify therapy programs, or transfer the patient under dynamic observation.
- Complete remission - complete regression of all signs of the disease (clinical, hematological and other manifestations of the disease) according to imaging tests, determined twice with an interval of at least 4 weeks.
- Partial remission is a reduction in the size of tumor formations by at least 50% for a period of 4 weeks in the absence of new lesions.
- Stabilization of the disease is a reduction in the size of tumor formations by less than 50% or an increase in them by no more than 25% of the original volume in the absence of new lesions.
- Progression is the appearance of new lesions during treatment or an increase in previously existing ones by more than 25%, as well as the appearance of symptoms of intoxication.
- Relapse is the appearance of new lesions after achieving complete remission.