Article for the “bio/mol/text” competition: Doctors have long noticed that the occurrence of life-threatening exacerbations of cardiovascular diseases, such as myocardial infarction, stroke, serious attacks of arrhythmia, is often associated with a certain time of day - such complications appear much more often early morning. Having become interested in this feature, doctors conducted numerous studies and found that this phenomenon is closely related to the work of the body’s internal clock, and that when studying cardiovascular diseases, it is necessary to pay attention to the peculiarities of the regulation of the body’s circadian rhythms.
What is circadian rhythm
We live in accordance with the rhythms of nature: after night, day inevitably comes, darkness is necessarily replaced by light. And, in order to adapt to this regular alternation of conditions set by the external environment, our body has developed a very complex and as yet not yet fully understood mechanism of the internal clock - our “built-in chronometer,” which physiologists call the daily or circadian (circadian) rhythm. If literally translated from Latin, “circa” means about, and dia means “day”. That is, the circadian rhythm is a rhythm with a period of about a day. Why was this prefix “about” needed? The fact is that the time of completion of the full cycle of our “built-in chronometer” is still controversial among scientists, since the internal regularity of the body does not fit exactly into the 24 hours that make up our astronomical day.
In 1962, physiologist-researcher Aschoff, as an experiment, sent his sons to a sound- and light-proof bunker, where they lived, focusing only on their internal rhythms, and not on the alternation of light day and dark night. This study showed that the internal chronometers of regular variability in human physiological functions are actually tuned to a 25-hour rhythm [1]. But there is another opinion. For example, the results of an experiment led by the famous speleologist Michel Cifra demonstrated that participants imprisoned in a cave for several months experienced a gradual transition from 24-hour rhythms to 48-hour ones: a person needed 36 hours to be awake and 12 to sleep [2 ].
But, one way or another, there is no doubt that an internal biological clock operates in our body, and it works, as genetic research in recent years has revealed, in every cell of our body. The genetic nature of biological rhythms began to be revealed in 1971, when for the first time in the world the clock gene Per was found in the Drosophila fly - it was called an abbreviation for the word “period” [3]. It was observed that a mutation in this gene caused deviations in the periodicity of the circadian rhythm in flies. These studies laid the foundation for a number of discoveries, as a result of which the modern understanding of the molecular structure of the biological clock was formed.
Aging and longevity
A series of articles conceived as part of the “biomolecules” special project for the Science for Life Extension Foundation.
In this series, we will consider the general problems of aging of cells and organisms, scientific approaches to longevity and prolongation of healthy life, the connection between sleep and aging, nutrition and life expectancy (let’s turn to nutrigenomics), we will talk about organisms with negligible aging, we will cover the topics of (epi)genetics of aging and suspended animation
Of course, the phenomenon of aging is so complex that it is too early to talk about radical successes in the fight against it or even a clear understanding of its causes and mechanisms. But we will try to select the most interesting and serious information about the discovered connections, model objects, developed and already available technologies for the correction of age-related disorders.
A brief summary of the special project is highlighted in the video “To grow old or not to grow old? // Everything is like animals.” You will learn more from our articles.
Stay tuned!
Hierarchy of internal biological clocks
So, how does our internal clock work? Recent studies indicate that the internal pacemakers in our body are organized according to the laws of hierarchy: there are the most important clocks and subordinate clocks. The main center of the circadian clock is the suprachiasmatic nucleus in the brain, a dense cluster of about 20 thousand neurons, and it is located just next to the center that regulates the production of hormones in the body. As for the subordinate clocks, as analysis of gene expression in the cells of internal organs has shown, genes responsible for circadian rhythms are expressed in every cell of the body, including even connective tissue. This led scientists to believe that each organ has its own internal clock. The internal clock system of the internal organs was called the peripheral clock, and the suprachiasmatic nucleus that controls them was called the central clock (Fig. 1). The liver, blood vessels, heart, and kidneys have their own chronometer. But for the body to function effectively, it is extremely important that all clock mechanisms are tuned to work harmoniously in the same rhythm - synchronized.
Figure 1. Hierarchy of the internal biological clock: the main center of the circadian clock is the suprachiasmatic nucleus in the brain, which sets the rhythm of all cells of the body through the autonomic nervous system, specialized hormones and various factors. Subordinate clocks in the cells of internal organs are called peripheral.
The phases of internal chronometers can shift under the influence of certain stimuli that can impose their own rhythm. Such stimuli are called zeitgebers (from German Zeit - “time” and geben - “give”) or pacemakers. Each watch is capable of responding to its own specific pacemakers. For example, light sets the rhythm of the central clock in the suprachiasmatic nucleus, while it does not directly affect the peripheral clock. Zeitgebers can be not only external influences, but also behavioral patterns: physical activity regimen, sleep-wake cycle, and even diet. For example, it has been clearly shown that the internal clock of the liver is more tuned to the rhythm of food intake than to the rhythms of the light and dark periods of the day [4].
The main physiological synchronizer of all peripheral clocks is the suprachiasmatic nucleus. Thanks to their connections with the light-sensitive cells of the retina, the neurons of the suprachiasmatic nucleus are able to receive information about the photoperiod from the outside and adjust the internal rhythms of the body to external conditions. Synchronization of peripheral clock systems is carried out through the autonomic nervous system by special hormones and, possibly, other, as yet poorly understood, pathways. Every year, scientists discover and describe in detail more and more new factors that influence the regulation of internal rhythms [5].
What is the circadian index
Various diagnostic techniques are used to assess cardiac activity. One of them, based on daily monitoring, is the identification of the circadian index (CI).
The human heart beats at a specific frequency, and in a graphical representation it resembles a sine wave. Normally, the resting heart rate is no less than 60 and no more than 90 per minute.
Not every patient understands what it is - the circadian index, for which it is necessary to know its meaning. This indicator allows you to determine the dynamics of cardiac activity over a long period of time (24 hours), obtain reliable information about hemodynamics and the course of certain somatic diseases.
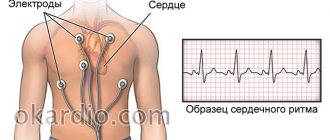
Holter monitoring
The circadian index value is calculated based on Holter monitoring data. In this case, the activity of the heart is recorded throughout the day.
For the first time, such a survey was proposed by the American biophysicist N. Holter in 1961, which is why it was subsequently named after him.
Monitoring is carried out using a portable device that records a daily electrocardiogram. The information received is deciphered only by a specialist, based on the suspected or established disease.
Calculation of the index and its norm
The indicator is calculated by the formula: the average daily heart rate (HR) for the period from 7.00 to 22.00 hours, divided by the average nighttime rhythm from 23.00 to 06.00 hours.
The optimal index value in adults and children ranges from 1.22 to 1.44, the norm as a percentage ranges from 122% to 144%, i.e. in the daytime the heart rate should be 22-44% higher than in night. The average value of the indicator is 1.32 (132%) with a permissible error of 0.08 in the direction of both decrease and increase.
In order to calculate the CI rate, specialists conducted a number of experiments. They showed that in healthy people, gender and age do not affect the indicator. In children under one year old, the normal CI is 115%, after 12 months - 120% and then equals the indicators for an adult.
What does deviation mean?
Due to the fact that many cardiac pathologies have a detrimental effect on the nerve fibers of the myocardium, as they progress, the value of CI changes. To assess the dynamics of the disease and adjust therapy, regular Holter monitoring is required.
A decrease in the index occurs in acute stroke and heart failure.
Deviations in values can be either up or down:
- Below 1.2 (or daytime heart rate is only 20% different from nighttime) – a rigid rhythm, which is a consequence of diseases affecting the intracardiac nervous system.
- Above 1.5 (or more than 50% excess of daytime heart rate over nighttime) is an indication that the heart rate is sensitive to sympathetic stimulation.
With a reduced rhythm, there is a risk of developing arrhythmia, ischemia, and cardiomyopathy. If therapy is not started in time, sudden death syndrome is possible.
An increase in heart rate is often observed in people with the development of nocturnal bradycardia and extrasystole. Increased heart rate occurs in trained athletes experiencing high physical activity.
Indications for monitoring
One of the research methods for heartbeat disorders is Holter monitoring. Indications for its implementation are:
- rapid heartbeat, dizziness, fainting;
- suspicion of arrhythmia (the person is examined to correct the heart rate);
- the need to assess the proper blood supply to the heart muscle.
In addition, 24-hour monitoring is prescribed after a heart attack to determine adequate treatment, as well as to evaluate therapy for various arrhythmias and heart failure.
The value is calculated annually in the presence of diabetes mellitus, and more often if the glucose level is constantly significantly elevated.
Symptoms of deviation
Every person should be alert and consult a doctor for examination if the following signs appear:
- constant feeling of fatigue, dizziness with loss of consciousness in the absence of traumatic brain injury;
- fast or slow heartbeats;
- pain occurs during physical activity on the left side of the chest, radiating to the arm;
- strange cough in the absence of a cold, difficulty breathing.
You should be attentive to such symptoms if they appear when you start taking medications to correct your heart rate.
Factors influencing CI
In some cases, only the circadian index allows us to determine the presence of changes in the activity of the cardiovascular system.
- With an arrhythmia, such as ventricular tachycardia, a person may not experience unpleasant symptoms of its manifestation. Only with the help of the CI method is it possible to determine its presence in order to further prescribe the necessary examination and adequate therapy. With this pathology, the value of CI is reduced.
- A low level of the circadian index is observed when the blood supply to the heart is impaired, after a myocardial infarction.
- Taking d-blockers can increase the CI index, which indicates the sensitivity of the heart muscle to sympathoadrenaline effects.
Often, increased intracranial pressure is detected only when measuring the circadian index, since the person has not experienced any symptoms, such as dizziness, nausea, or headache.
A special risk factor is the presence of type 2 diabetes, aggravated by hypertension. With such a combination, macro- and microvascular complications arise, blood pressure rises, myocardial hypertrophy occurs, coronary heart disease and heart failure develop.
It is for this reason that patients with diabetes need to control CI.
Is treatment necessary?
A high or low indicator indicates the presence of pathology. To normalize it, it is necessary to identify the cause that caused the failure. Only after this the doctor chooses a therapeutic tactic, draws up an individual treatment regimen, and prescribes the necessary medications.
But there are also general principles of therapy:
- timely diagnosis of cardiovascular diseases and identification of other causes leading to the development of heart failure;
- immediate treatment of stroke and heart attack;
- treatment of pulmonary hypertension.
In addition, constant monitoring of patients with type 2 diabetes and hypertension is mandatory.
Loss of synchronization and disease progression
As experiments show, synchronization of all internal rhythms is an extremely important condition for maintaining health and life expectancy. When scientists study the relationship between a malfunctioning biological clock and heart disease, the obvious question that arises is what comes first: a breakdown in the internal clock causes heart disease, or is it the heart pathology itself that causes the malfunction of our built-in chronometers? In an attempt to answer this question, at least two opposing hypotheses have been put forward.
In support of the hypothesis that the loss of synchronization of internal rhythms is primary in the onset of the disease, a number of interesting experiments were conducted. Researcher Tami Martino analyzed the lifespan of golden hamsters with a specific mutation in the tau gene, which reduces the period of the circadian rhythm in the peripheral clock to 22 hours (Figure 2). In other words, the internal clock of this line of cheeky rodents is very fast. It turned out that the overall life expectancy of hamsters with the mutation is reduced by 20%, and they die at an early age from serious myocardial diseases - fibrosis and cardiomyopathies [6].
Figure 2. Golden hamster with a mutation in the tau gene: the hamster's internal clock is fast by two hours a day. The lack of synchronization of internal and external rhythms led to the fact that the rodent developed serious health problems - myocardial hypertrophy.
However, when artificial conditions were created for such hamsters so that the period of alternating light and darkness was 22 hours, the cardiac pathology was replaced by normal functioning of the heart. Moreover, removal of the suprachiasmatic nucleus, the main clock of the body, also had a preventive effect: myocardial hypertrophy did not develop in golden hamsters after the operation. What is the reason for such a miraculous healing?
The results obtained indicate that it is not so much damage to the peripheral clock as loss of synchronization between the central and peripheral pacemakers that leads to the occurrence of cardiovascular pathology. In mutant hamsters, there was a mismatch between the 22-hour period of the peripheral clock and the 24-hour period of the central clock. When a rhythm of 22 o'clock was imposed on the central chronometer through changes in external conditions (light/dark), it was synchronized with the peripheral clock, and cardiac pathology did not develop. And when the suprachiasmatic nucleus was removed, then again nothing prevented the peripheral clock from freely implementing its own rhythm, and the hamster’s heart was again saved.
On the other hand, the disease itself can disrupt the coherence of internal biorhythms. For example, during acute myocardial infarction, damaged cells undergo a phase shift in the circadian clock relative to healthy tissues. This loss of synchronization is very dangerous and can cause life-threatening arrhythmia attacks.
Restoring the coherence of heart cell rhythms with the natural cycles of other organs and tissues and with cyclical changes in environmental conditions may be a promising strategy in the fight against cardiovascular diseases. But to implement this direction, very deep knowledge about the patterns of functioning of biorhythms is required. Interestingly, even in healthy people, the circadian rhythm of the cells in the inner lining of the veins varies depending on their anatomical location. Further research is needed to identify all the zeitgebers in the body as accurately as possible, and to use this knowledge to repair our built-in chronometers if they fail.
Material and methods.
The circadian profile of the heart rhythm was assessed based on the calculation of CI as the ratio of the average heart rate during the waking period (from 07 to 22 hours) to the average heart rate during night sleep (from 23 to 06 hours) /2.4-7/. The CI indicator was calculated based on the results of 22 published works, where the average daytime and nighttime values of heart rate or RR intervals were presented separately in healthy subjects and patients aged 2 to 99 years, both according to the results of classical HM and blood pressure monitoring /10, 27/ (Tables I and II).
In works reflecting the results of a study of the circadian rhythm of the heart in healthy individuals, the calculation of the difference between the average night and day values of RR intervals was also carried out: Night/day difference (Ndd), a parameter for the time analysis of heart rate variability, also used to analyze the circadian rhythm of heart rate / 12.13/. Statistical processing of the results was carried out using the Excel software package.
Daily variability of cardiovascular parameters
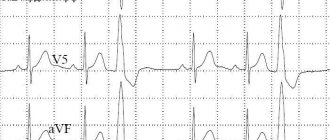
Another very important point is that during the day the heart’s sensitivity to stress, emotional and physical stress varies. The indicators of cardiovascular function themselves also change over time: blood pressure, blood flow speed, heart rate and others. Continuous recording of an electrocardiogram for 24 hours in people at rest shows that a person's heart rate is constantly varying: it reaches a minimum in the fifth or sixth hour of sleep and at this time is 48–50 beats per minute. It reaches its maximum in the evening, at about 6 p.m., and then gradually begins to decrease again.
All these phenomena are possible due to the complex molecular mechanisms of the cardiovascular system's own peripheral clock. About 10% of genes expressed in cardiac cells have a daily rhythm of expression. Currently, an active search is being carried out for factors affecting the functioning of the heart and having circadian rhythm. Molecular clocks have already been found in the muscle cells of the heart, in the cells of the inner lining of blood vessels (in the endothelium) and in the muscle cells of blood vessels.
Circadian index: what is it, norms and reasons for decreased and increased indicators
Disturbances in the normal activity of cardiac structures are represented by the diagnosis category in ICD-10. Each has a group of symptoms, its own clinical picture and, with careful assessment, can be distinguished from the other.
The problem is that external signs do not always correlate with the real state of affairs; not in every case they accurately indicate a disease. Objective research methods allow us to understand the issue. Including ECG.
The circadian index is the ratio between the heart rate during the daytime and the same indicator at night. It is calculated during daily Holter monitoring using a programmable device.
The calculation is carried out automatically, human participation is not required, and studying the indicator manually is extremely problematic.
Hospital stay is not required for calculations. On the contrary, it is desirable that the patient remain in natural conditions. This way the assessment will be more accurate. The detected level is recorded and used to determine the likely severity of the functional impairment.
Norms and calculation formula
The formula for obtaining the circadian index in adults is calculated simply: you need to take the average heart rate in the period from 6 to 22 hours and divide it by the heart rate level in the period from 22 to 6.00. The resulting number will be the desired one.
The circadian index norm is determined in the form of a decimal coefficient. An adequate value is in the range from 1.2 to 1.4, plus or minus 0.3.
- The growth of the conditional level is considered not such a dangerous indicator. Occurs in athletes and people of physical labor. Less often for pathogenic reasons.
- A decrease in numbers is the result of pathology of the cardiovascular system. The rate of fall directly correlates with the likelihood of death. It is considered an important prognostic point.
It is possible to carry out repeated daily monitoring and, accordingly, calculate the circadian index. The frequency of changes depends on the likely pathological process.
The classic scheme is a study before the start of treatment, during, approximately a week after the start of therapy, and after the course. This will allow you to see the picture in dynamics and evaluate the effectiveness of the measures.
The norm as a percentage is rarely calculated, because the level is difficult to perceive and is not widely used in medical practice. Standard values are from 120 to 140%, perhaps a little higher, but not lower.
Symptoms of QI deviation
The circadian index is not a diagnosis or even a manifestation of a pathological process. We are talking about an instrumental result, a specially calculated indicator. Therefore, it is incorrect to talk about the clinical picture.
It is necessary to consider the pathological process that is behind this diagnostic finding, and there are many of them.
Standard symptoms that cause the circadian index to be below normal:
Heart rhythm disturbances
Usually a type of bradycardia of varying severity. From a slight drop in heart rate, which the patient does not even feel, to a critical level leading to Morgagni-Adams-Stokes attacks.
Usually we are talking about heart failure, a previous heart attack, cardiomyopathy and other abnormalities, including defects.
Dyspnea
Against a background of peace. After physical activity it increases several times. Lying down can result in asphyxia and death of the patient.
Typically, such a severe manifestation is observed in the decompensated phase of heart failure.
Chest pain syndrome
Slight or medium in strength. Appears after intense physical activity. Similar to that of angina pectoris.
The pain is pressing or burning, spreading in nature. They appear after activity and go away in a matter of minutes.
Cough
For no apparent reason. Pulmonary etiology cannot be excluded by eye. It is necessary to carry out at least an x-ray, only then there is a chance to delimit the pathological processes.
The symptom intensifies after physical activity and is not relieved by bronchodilators. Combined with shortness of breath and asphyxia. Continues almost constantly, does not leave the patient for a minute.
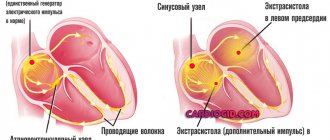
Extrasystole
Changing the intervals between each subsequent heartbeat. The essence of this condition is the appearance of extraordinary contractions at the moment of relaxation of cardiac structures (diastole).
Singles are not dangerous. But against the background of a decrease in the circadian index, group, paired extrasystoles (bigeminy) come to the fore. They pose a great threat to the patient's life. Urgent relief of the condition is necessary.
Dizziness
Develops as a result of a decrease in myocardial contractility. This phenomenon is indirectly confirmed by a decrease in the circadian index: a disruption in the normal nutrition of the brain affects it.
This is an unfavorable prognostic sign. The risk of stroke—an acute weakening of blood circulation in cerebral structures—is growing. Manifests itself as the impossibility of normal orientation in space. The world literally floats before your eyes, the earth disappears from under your feet.
Headache
Cephalgia. Localized in the area of the back of the head, crown. Baling in nature. Follows the beat of the heart. It intensifies after a change in body position and is accompanied by severe heaviness in the chest.
Nausea, vomiting
Reflexive in nature. Such manifestations are associated with a malnutrition of the brain, as in previous cases. Restoration of the normal state occurs independently.
Fainting
Syncope or disturbances of consciousness. They appear suddenly. As a rule, in the early stages they are short-term and appear rarely. The patient can be easily returned to normal. Then the process gets worse.
Rigidity of the circadian rhythm (instability, drop in level) affects a group of cardiac, respiratory and neurogenic manifestations.
How severe it is depends on the underlying disease. At the same time, it is possible to control the dynamics and course of the pathology, including using the specified value.
If the circadian index is elevated, there are most often no manifestations. This is not always good. There are several reasons: disruption of the nervous system, professional training, extrasystole and others.
The clinical picture in this case may be completely absent.
Reasons for decreased qi
The factor is always cardiac.
- Heart failure. The main pathological process that ends with a decrease in myocardial contractility, a small volume of blood ejection into the systemic circle and disruption of the functioning of all organs and systems. Poses the greatest danger. Develops as a result of a long course of arterial hypertension or a heart attack.
Read more about the symptoms of acute heart failure in this article.
- Cardiomyopathy. Growth, thickening of the walls of the muscular organ, expansion of the chambers always causes the circadian rhythm to decrease. Recovery as such is impossible. This is an anatomical phenomenon, it exists constantly. On the other hand, there is a chance of compensation through medication, then the circadian index will return to normal.
- Inflammation of the heart muscle (myocarditis, pericarditis). Autoimmune or infectious origin, when the pathology goes far in its development. It manifests itself as bradycardia, which is not typical for this diagnosis. This is a terrible sign. Urgent treatment is required. Although it needs to start even earlier, as soon as the process has begun.
A drop in CI may be the result of taking antiarrhythmic drugs. Then you need to wait a while and do the research again.
Reasons for increasing QI
They are relatively rarely pathological. More often, a deviation in the circadian index indicates that the body is highly trained.
The violation (relatively speaking) is inherent in professional athletes and representatives of physical labor. In this case, recovery is not required, but the patient must be monitored.
You never know how your heart will behave next. Fatal consequences as a result of decompensation of the condition are quite possible.
Also, the cause of increased CI is an increase in pressure in the pulmonary artery and the accompanying dysfunction of the organ, anatomical defects, the so-called cor pulmonale.
Diagnostics
It is carried out on an outpatient basis. Hospitalization is required only in critical cases. Specialist - cardiologist.
Approximate list of events:
- Oral questioning of the patient regarding complaints. Objectification of symptoms allows you to build a clear clinical picture and put forward approximate hypotheses regarding the possible disruption of the heart.
- Anamnesis collection. Previous illnesses, habits and lifestyle, family history, other points.
- Measuring blood pressure using routine methods. Using a regular tonometer. Used for immediate assessment of vital signs.
- The basis of diagnosis is daily Holter monitoring. Only it can provide accurate information on the circadian rhythm. The measurement is carried out every half hour or hour and is entered into the memory of an automatic programmable device. Then the device independently calculates the indicator and remembers it.
- Then doctors have more opportunities for diagnosis, the vector becomes clear. Because the numbers usually depend on the probable pathological process.
- The following shows electrocardiography. It is necessary to detect rhythm disturbances. For example, extrasystoles and other similar deviations.
- Echocardiography. Ultrasound research technique. It is used for early detection of anatomical defects or determining the stage of the disorder.
- MRI if necessary.
- Load tests. If there is no reason to suspect anatomical defects, heart failure or other dangerous conditions. It is carried out under the supervision of doctors in order to provide first aid if necessary.
Other specialists may be involved. They are not able to eliminate the cause of the disorders, but identifying abnormalities in the nervous system and respiratory activity is their prerogative.
Treatment
Treatment of the underlying pathological process is carried out. The circadian index should not be specifically normalized. Yes, and there is no such possibility. Contractility needs to be increased.
https://www.youtube.com/watch?v=Ri_fhBhj_UE
Treatment is mainly conservative, with the use of medications to relieve symptoms and combat the etiological factor. Both problems are solved at once.
What drugs are prescribed:
- Antiarrhythmic. Amiodarone or Quinidine. To restore normal heart rate and intervals between contractions. Used in short courses, it is not used on an ongoing basis due to the significant danger and mass of side effects.
- Antihypertensive. As needed. ACE inhibitors, calcium antagonists, centrally acting agents, diuretics with a mild, potassium-sparing effect. The names are selected by the doctor. With illiterate therapy, rapid development of heart failure and death of the patient in the short term is possible.
- Beta blockers. They help lower blood pressure and stop tachycardia. Increased frequency also occurs, but less frequently. If the normal functioning of the heart is disrupted, such as bradycardia, they are never prescribed.
- Cardiac glycosides. If there are no symptoms of coronary insufficiency, ischemia of cardiac structures.
If necessary, statins are also indicated to dissolve cholesterol plaques and eliminate excess low-density lipids. Antiplatelet agents, special agents for normalizing the rheological properties of blood and preventing the formation of blood clots.
The operation is prescribed in extreme cases, strictly according to indications. These are considered to be heart defects. Congenital and acquired. Aortic, mitral, tricuspid valves, the vessels themselves, during the formation of aneurysms and other conditions.
Up to the destruction of chambers, for prosthetics or mechanical expansion of arteries (stenting, ballooning), creating bypass paths of blood flow (bypass surgery).
Radiofrequency ablation is possible for blockades of the conduction system (cauterization of an excessively active area).
The choice of the optimal direction of therapy is decided at the discretion of the doctor. The patient is instructed to limit himself for the rest of his life. But these are reasonable limits that will not cause much discomfort.
Quit smoking, alcohol, no drugs, no anti-inflammatory drugs without a doctor’s prescription, less fatty and fried foods in the diet. Get adequate sleep and at least minimal physical activity.
This is quite enough. Not a high price to pay for health, and possibly life.
Forecast
Mostly favorable. Changes in the circadian index are not an independent disease. This is not a diagnosis at all. Therefore, you need to look at the primary pathological process.
What is it and how aggressively is it progressing, at what stage was it detected, is there a positive reaction to the therapy.
The patient’s age, gender, lifestyle and habits, family history, and other points that should be taken into account in combination also play a role.
It is impossible to say even on average what a patient can expect. There are so many diseases, so many prognoses. Within the same diagnosis, the probabilities differ significantly.
It is better to address the question to your attending physician. He will be able to give a clear answer, but not immediately. An assessment of the patient's condition, diagnosis and primary treatment is needed.
Factors that worsen the outcome:
- Presence of concomitant diseases. Especially neurological or endocrine (diabetes mellitus as the leader).
- Age over 50.
- Unfavorable family history.
- Lack of positive dynamics with the use of drugs.
- The need for surgery when it is impossible to perform it due to the general serious condition of the patient.
- A drop below 1.2 indicates a critical process. The probability of death is high.
If the circadian index is reduced, it means that there is a decrease in myocardial contractility. This is a generalized functional process.
For what reasons it arises, it is necessary to clarify using diagnostic methods. Usually heart failure, previous heart attack, developmental defects.
The indicator is restored after cure or at least compensation of the condition. The probability of a positive outcome is quite high even against the background of advanced diseases.
Source: https://CardioGid.com/tsirkadnyj-indeks/
Molecular clock in cardiac muscle cells
Recently, scientists published a report in the journal Nature that the protein Klf 15 (kruppel-like factor), which controls the processes of tissue formation, fat metabolism and inflammation in the body, can also influence the circadian rhythms of the heart. The concentration of this protein varies depending on the stage of the sleep-wake cycle. The researchers bred lines of mice with two variant mutations in the gene encoding Klf 15, which led to the fact that the level of the factor in the blood plasma was either excessively elevated or the protein was absent altogether. In both cases, the mice suffered from life-threatening cardiac arrhythmias [7].
Upon deeper study, it turned out that Klf 15 is only the first step in a complex molecular cascade, because it controls another protein, KChIP 2 (Kv channel-interacting protein), a factor that interacts with potassium channels in cardiac muscle cells. Changes in the concentration of KChIP 2 lead to electrical instability of heart tissue and, as a consequence, to cardiac arrhythmias; Moreover, the gene for this factor has a daily rhythm of expression.
The potassium channel genes of cardiac muscle cells Kv1.5 and Kv4.2 also have a daily rhythm of expression. Interestingly, the expression of Kv1.5 increases during the dark period, while messenger RNA of the Kv4.2 protein is found in higher concentrations during the light period. Rhythm disturbances in any link of this complex system can be associated with the daily time of occurrence of arrhythmia attacks.
Results and discussion.
The results of the CI calculation are presented in Tables I and II. There is a high stability of CI in all groups of healthy subjects (Table I), regardless of gender, age and type of equipment used (CM, non-invasive/27/ or invasive blood pressure monitoring/10/). The CI value, based on our calculation based on the results of 20 studies combining the results of daily monitoring in 7870 healthy subjects aged 10 to 79 years (Table I), practically does not differ from the normative parameters we previously determined (1.32 + 0.06) /4-7/ and on average is 1.33 + 0.05. A study by J. Freitas et al. /17/ showed high reproducibility of the daily structure of heart rate, even when changing periods of sleep and wakefulness in shift workers.
We also compared the CI with the difference between the night and day values of the average RR interval in the indicated works (Table 1) and correlated these parameters with heart rate values. A significant correlation of the Night/day difference was noted with the night-time heart rate level (r = -0.61), while no significant interdependencies were identified between the heart rate and CI parameters. As can be seen from our calculations, the close dependence of this indicator on the initial heart rate level, high variability with age-related and physiological fluctuations in the average heart rate value (sinus bradycardia or tachycardia), even in healthy subjects, lead to the lack of stable normative standards in the assessment, which did not allow it has yet to find wide application in practice. The maximum Ndd value in our analyzed group of healthy people (N 19, Table 1) is almost 2 times (42%) higher than the minimum (N 2, Table 1), while CI in the same group does not differ significantly ( differences by 12%), NN 1 and 20 in Table 1.
We identified significant changes in the circadian profile of heart rhythm in patients with diseases of the cardiovascular system. Calculation of the CI index in the work of Molnar J. et al /21/ showed an increase in the rigidity of the circadian rhythm of the heart as the severity of the disease increased: CI 1.31, 1.24 and 1.1, respectively, in the control group of healthy people, in survivors and in patients who died suddenly with pathology of the cardiovascular system (dilated cardiomyopathies, heart attacks, idiopathic arrhythmias, arterial hypertension, etc.). In a study by G. Casolo et al. /12/, we noted a progressive smoothing of the circadian rhythm profile in patients with coronary heart disease and hypertrophic cardiomyopathy who died during observation, compared with survivors (CI 1.03 in dead and 1.09 in surviving patients ).
Determining the characteristics of the pathophysiological mechanisms underlying changes in circulatory system is possible by analyzing the circadian profile of the heart rhythm in groups of patients with verified disorders of the vegetative status. As an analysis of works studying the features of circadian rhythms in diabetic patients, a classic clinical model of autonomic imbalance, has shown, damage to both the parasympathetic and sympathetic parts of the nervous regulation of heart rhythm contributes to the formation of circadian rhythm rigidity. In all cases, the CI values we calculated were lower in patients with clinically pronounced total vegetopathy (NN 4,13,14,19. Table II), compared with diabetic patients without damage to the autonomic nervous system (NN 20, 24. Table. II). The importance of sympathetic denervation in the pathogenesis of decreased CI is confirmed by the analysis of the work of Hintze U. et al. /16/. When using the beta-blocker metropolol in patients over 70 years of age who have suffered a first myocardial infarction, there is an increase in the rigidity of the circadian rhythm (CI 1.16 at baseline and 1.13 after 6 months with constant use of metropolol), with the opposite dynamics of CI in the placebo group -control (1.13 at baseline and 1.2 after 6 months). The most demonstrative evidence of the influence of the autonomic nervous system on the formation of the circadian heart rate profile can be considered our analysis of the results of the classic study by D. Ewing et al. /15/. The authors assessed, based on the results of CM, heart rate variability in healthy people, in 3 groups of diabetic patients with varying degrees of severity of vegetopathy (without vegetopathy, with isolated parasympathetic denervation and total vegetopathy) and in patients with transplanted hearts, as a model of complete surgical denervation of the heart. Calculation of CI showed a progressive increase in the rigidity of the circadian heart rate profile as the degree of vegetopathy increases. The CI values were 1.41; 1.35; 1.25; 1.19 and 1.11, respectively, in the healthy control group, in diabetic patients without vegetopathy, with damage to parasympathetic innervation, total autonomic blockade and patients with transplanted hearts. Thus, the analysis allows us to assume that the basis for the persistent development of circadian rhythm rigidity (decrease in CI < 1.2) is the mechanism of total vegetopathy, with a violation of both the afferent and efferent links of the vagosympathetic regulation of heart rhythm, the development of the “denervated” phenomenon hearts. Smoothing of the circadian rhythm profile reflects the depletion of adaptive heart rhythm reserves and is clinically associated with a poor prognosis and a high risk of arrhythmogenic syncope and sudden death in patients at risk /12,15,19,21/. At the same time, in patients with severe neurological pathology, but without pronounced clinical signs of autonomic disorders (NN 22,23. Table II), the value of CI did not differ from the group of healthy people and patients with prognostically more favorable forms of arrhythmias (NN16,25,25 ,26,28.Table II).
The phenomenon of strengthening the circadian profile of the heart rhythm (increase in CI > 1.45) in our studies was noted in patients with idiopathic bidirectional ventricular tachycardia /7/. From the works of other authors, we noted an increase in CI in a study by Mathias C. et al./20/ in patients with chronic lesions of the nucleus tractus solitarius, a disease in which blockade of baroreceptor afferent impulses develops, but preservation of efferent symptomatic regulation, especially pronounced in response to physical , emotional stress /30/. Analysis of clinical work also confirms this assumption. Galassi A. et al./18/, assessing the circadian rhythm of the heart in patients with the so-called syndrome X (angina attacks in patients with normal coronary angiography), compared with patients with coronary heart disease and healthy volunteers, noted no differences in nighttime heart rate values in all groups, however, daily heart rate values were significantly higher in patients with syndrome X, which, when calculating CI, leads to an increase in this indicator. At the same time, the levels of adrenaline and norepinephrine in the blood plasma measured in this group of patients were not increased, which indicates the absence of a tonic increase in sympathetic activation and speaks more about increased sensitivity to catecholamines. In Pickering Th. et al./26/ CM was performed in 12 patients with extrasystole. Based on the values given in the work for daytime and nighttime heart rate levels for the group as a whole (75.5 + 9.5 and 61.2 + 12.7 beats/min, respectively), the calculation of the CI indicator was 1.26, i.e. did not go beyond the normative values we found. But when analyzing the individual dynamics of the heart rhythm in the examined patients, the maximum values of CI (1.68, 1.56 and 1.42) were noted in patients who were characterized by a decrease in the frequency of extrasystole at night by more than 90%. Only in patients with CI above 1.5, a pronounced increase in extrasystole was noted during bicycle ergometry.
In recent years, the calculation and interpretation of changes in CI based on the results of CM or 24-hour blood pressure monitoring have found widespread use in domestic clinical practice /35-45/. There are many studies in which we can talk about the demand for the use of CI, since the authors in a descriptive manner state a smoothing /46,47/ or strengthening of circadian rhythms of heart rate /48/, but without using a specific assessment parameter they cannot interpret the mechanism and clinical significance of these changes . This significantly complicates the clinical interpretation of the identified changes and does not provide the doctor with specific information to assess the patient’s condition and/or prognosis of the disease during treatment. The use of a standardized criterion for assessing the dynamics of the circadian rhythm of heart rate will help expand the diagnostic capabilities of CM, identify new pathogenetic links of cardiovascular diseases, and optimize the entire scheme of treatment and preventive measures in patients with cardiac pathology.
Conclusions:
1. The circadian index, calculated from the results of Holter or blood pressure monitoring as the ratio of the average heart rate during wakefulness to the average nighttime heart rate, reflects the basic structure of the circadian heart rate rhythm.
2. The CI value is within the range of 1.24 -1.44 USD. (M 1.32 + 0.06) is an indicator of the stable autonomic organization of the circadian rhythm of the heart.
2. A decrease in CI less than 1.2 is observed in diseases associated with autonomic “denervation” of the heart and is associated with a poor prognosis and a high risk of sudden death in patients at risk.
3. An increase in the circadian profile of the heart rate (increase in CI above 1.5) is associated with increased sensitivity of the heart rate to sympathetic stimulation.
For correspondence Dr.Med.Makarov L.M 127412 MNIIP and DH Ministry of Health of the Russian Federation, Moscow, Russia.
Tel. (095)483-2101. Email
Synchronization of the molecular clock of cardiac muscle cells with lipid metabolism
We have already talked about how important it is to synchronize heart rhythms with the cycles of other physiological systems of the body. It is equally important to note that some internal cycles are capable of imposing their rhythm on the heart clock. One of these master cycles is the daily rhythm of the circulation of fatty acids and lipid levels, which is tightly linked to the circadian one. Fatty acids are the primary “heart fuel”: 70% of them are utilized by the heart. With an excess of fatty acids, the contractile function of the heart is suppressed, and the heart responds to these changes in the internal environment by activating both oxidative (mitochondrial) and non-oxidative metabolism. In this way, the heart reduces cellular toxicity caused by fatty acid loading. And this process is also associated with the daily rhythms of gene expression.
American researcher Molly Bray studied circadian clock genes using DNA microarray technology. She was able to identify 548 genes that regulate the clock in atrial cardiomyocytes and 176 genes associated with the circadian rhythm of ventricular muscle cells. These included genes involved in lipogenesis and lipid binding proteins; all of them showed diurnal expression [8].
Peripheral clock in endothelial cells
Several groups of scientists have demonstrated the role of clock genes in the function of the endothelium, the tissue lining the inside of blood vessels and the heart. They found that in mice with a mutation in the Per 2 clock gene, blood vessels do not relax in response to the influence of the main relaxing neurotransmitter, acetylcholine. In addition to this very unpleasant dysfunction, a very high concentration of substances that stimulate vascular compression is detected in the blood of mice, which is fraught with the occurrence of arterial hypertension [9].
But the health problems for the unfortunate mice did not end there. Researcher Chao Wang showed that if endothelial cells have a mutation of the Per 2 gene, then blood vessels quickly age, are poorly restored after damage, and the life expectancy of rodents themselves is greatly reduced [10].
Peripheral clocks in vascular muscle cells
The smooth muscle cells of blood vessels - myocytes - also have their own peripheral clock. Takishige Kunieda studied the circadian system in aging vascular myocytes. He found that in these cells, the loss of circadian rhythmicity is associated with telomere shortening. The introduction of telomerase prevented problems with the expression of clock genes. These studies suggest that telomerase regulation may be one of the therapeutic options for age-related circadian rhythm disorders [11].