Home / Phlebology / Congenital dysplasia or aplasia
A congenital venous defect is visible in a child immediately after birth. However, in some cases, the pathology manifests itself years later. Congenital dysplasia or aplasia can have a mixed form. Capillary disease is characterized by decreased blood flow. Arterial pathologies are characterized by increased blood flow.
Reasons for appearance
Typically, pathology begins to develop in the embryo during the period of 4-8 weeks of intrauterine development. It is during this period that the human circulatory system is formed.
The reasons for the development of vascular dysplasia have not been fully identified. The development of pathology is influenced by many genetic abnormalities. Taking harmful medications, maternal age, chromosomal abnormality, infection can have a direct effect on the development of fetal blood vessels.
Provoking factors also include:
- diabetes;
- fetal hypoxia;
- tuberculosis;
- exposure to carbon monoxide.
How to suspect venous disease?
Venous disease itself involves a lack of blood flow. Depending on the affected area (brain and legs), dysplasia may be accompanied by:
- discomfort/pain/distension in the development zone (this may be due to thickening of the walls of blood vessels or venous duplication);
- skin pigmentation is often observed with venous dysplasia;
- due to compression of the venous system by strands of fibrous tissue, it is possible to stretch one leg relative to the other;
- Dysplasia often accompanies varicose veins.
Venous dysplasia occurs in approximately 2-3 babies out of 100. The exact reasons for its occurrence remain unknown. The disease can occur without symptoms (approximately 30% of cases). The most difficult cases of venous disease are associated with the concentration of affected vessels deep in the muscles.
The main threat is not, in fact, dysplasia, which is de facto a defect of the venous system (localized or generalized), but possible complications, the treatment of which should be addressed. These consequences of venous insufficiency include:
- various forms of vascular malformations (pathology of connections between veins and arteries, which can lead to insufficient blood supply to parts of the body);
- cavernous hemangiomas (vascular formations visible on the skin);
- thrombosis;
- thrombophlebia;
- thrombotic ulcers;
- aneurysms.
Treatment of venous dysplasia
Treatment methods for venous dysplasia resemble complex therapy for varicose veins in deep stages. — Drug therapy improves blood flow and prevents the formation of blood clots (thrombi). — Surgical treatment restores the patency of deep veins and eliminates superficial veins, in the place of which healthy veins are formed. — Compression therapy improves the functioning of the venous system, prevents the appearance of edema and trophic ulcers.
The Russian company produces compression underwear (tights and stockings) of 2 compression classes, which are suitable for young people with venous dysplasia of the superficial veins (before the appearance of trophic ulcers).
Recognizing venous dysplasia
There are frequent cases of venous dysplasia developing into phleboangiotic dysplasia. In this case, disability cannot be avoided. In the case of sepsis or rupture of an aneurysm due to venous disease, death is also possible.
For this reason, diagnosis of dysplasia should be carried out as early as possible - at the first suspicion of venous insufficiency. In modern phlebology practice, various tactics for recognizing deep vein dysplasia are used. Since the external signs of the disease make it possible to accurately determine its location, the following is carried out in the problem area:
- CT/MRI/ultrasound;
- angiography and other phlebological manipulations.
Brain imaging (MRI) is often done to confirm.
Literature
- Mulliken JB Hemangioma sandvascular malformations in infants and children: A classification based on endothelial characteristics / JB Mulliken, J. Glowacki // Plast Reconst Surg. – 1982 Mar. – Vol. 69, N 3. – P. 412–420.
- Venous malformations (angiodysplasia) - the possibilities of modern methods of diagnosis and treatment / V. N. Dan [et al.] // Phlebology. – 2010. – T. 4, No. 2. – P. 42–48.
- Ethanol Sclerotherapy for the Management of Craniofacial Venous Malformations: the Interim Results / Ho Lee // Korean J Radiol. – 2009 May-Jun. – Vol. 10, N 3. – P. 269–76.
- Venous malformations of skeletal muscle / KD Hein // Plast Reconstr Surg. – 2002 Dec. – Vol. 110, N 7. – P. 1625–35.
- Ethanol sclerotherapy of venous malformations: evaluation of systemic ethanol contamination / FD Hammer // J Vase Interv Radiol. – 2001 May. – Vol. 12, N 5. – P. 595–600.
- Advanced management of venous malformation with ethanol sclerotherapy: mid-term results / BB Lee // J Vasc Surg. – 2003 Mar. – Vol. 37, N 3. – P. 533–38.
- Diagnosis and treatment of venous malformations. Consensus Document of the International Union of Phlebology / BB Lee [et al.] // Int Ang. – 2009 Dec. – Vol. 28, N 6. – P. 434–51.
- Sonographically guided percutaneous sclerosis using 1% polidocanol in the treatment of vascular malformations / R. Jain // J Clin Ultrasound. – 2002 Sep. – Vol. 30, N 7. – P. 416–23.
- Treatment of venous malformations with sclerosant in microfoam form / J Cabrera // Arch Dermatol. – 2003 Nov. – Vol. 139, N 11. – P. 1409–16.
- Percutaneous sclerotherapy of peripheral venous malformations in pediatric patients / F. Gulsen // Pediatr Surg Int. – 2011 Dec. – Vol. 27, N 12. – P. 1283–37.
What can be done?
With dysplasia, it is important to direct maximum efforts to eliminate complications and prevent related vascular pathologies. Only this approach will allow you to completely get rid of dysplasia (possibly in more than 40% of cases).
The range of activities may include:
- laser therapy (coagulation) is one of the modern methods of activating blood supply channels, which gives a positive effect even in complex cases associated with cerebral or intramuscular damage;
- physical therapy is required (including contrast showers, electrical stimulation, whirlpool baths);
- Constant compression is also recommended for venous dysplasia, but only a phlebologist can select it.
Depending on the time of detection, both a course of medication and urgent surgical intervention may be effective. There is little room for independent actions with venous dysplasia. Therapeutic exercise, constant massage (kneading), control of regular load on the legs if the veins are affected in them - this is what a parent can do for the child himself. Without professional intervention, these measures will be absolutely insufficient.
Clinical case
The clinical case is demonstrated with the informed consent of the patient and written consent is submitted to the editor.
The patient, born in 1987, applied to the vascular surgery department of the Road Clinical Hospital, St. Petersburg, on May 17, 2010, with complaints of the presence of two formations on the right half of the face, deforming its shape.
Suffering from birth, notes slow growth of formations over the last 4 years (Fig. 1).
Rice. 1. Photo of the patient before treatment
One of the medical institutions in St. Petersburg performed a CT scan of the head, the results of which confirmed the presence of an area of angiomatosis in the area of the zygomatic arch and a solid hypervascular structure in the projection of the fat pad of the right cheek.
Medical care was refused with the recommendation of dynamic medical observation. Two years later, due to the further growth of the formations, the patient turned to the Department of Maxillofacial Surgery of the North-Western State University named after I.I. Mechnikov, St. Petersburg. Considering the progressive growth of education and a significant deterioration in the patient’s quality of life, an inpatient examination with staged surgical treatment was recommended at the angiosurgery department of the Road Clinical Hospital.
Upon admission, the condition was satisfactory. A comprehensive examination did not reveal any abnormalities in the internal organs and systems.
Local status. In the projection of the right zygomatic arch in the thickness of the subcutaneous tissue there is a formation of 4x4 cm, round in shape, soft-elastic consistency, with smooth contours, painless, the skin above it is of normal structure and color; in the depths of the subcutaneous tissue of the right cheek there is a similar formation of 5x5 cm, the skin of the cheek is of normal structure and color.
Ultrasound examination (Logiq Book XP device, color Doppler mapping mode, sensor with an operating frequency of 6.8 MHz) of the tissues of the zygomatic arch revealed areas of angiomatosis with different-sized vascular cavities with low- and medium-speed blood flow in the latter (Fig. 2).
Rice. 2. Ultrasound scan of angiomatous tissues
According to the results of a puncture biopsy of the cheek lesion, no evidence for the presence of a malignant process was revealed.
In June 2010, the following were performed: 1 session of foam-form sclerotherapy with 2% and 1 session with a 3% fiber-vein solution at an interval of 10 days. Both sessions without any clinical effect. From July 2010 to September 2010, four sessions of puncture endovasal laser coagulation (EVLC) of angiomatosis of the zygomatic region and two sessions of EVLC of hypervascular tissue of the cheek on the right were performed with a time interval of 10-14 days. In September 2010, laser ablation of a vascular neoplasm in the zygomatic region was supplemented with two procedures of foam-form sclerotherapy with a 3% fibrovein solution. All procedures with good immediate clinical and ultrasound effect (Fig. 3).
Rice. 3. Photograph of the patient after sclerotherapy and EVLT of angiomatous tissues
This formation significantly decreased in size; according to duplex angioscanning, blood flow in it was not recorded.
However, in the area of Bichat bodies, the formation retained its volume. In order to correct the shape of the face with radical removal of the solid structure of the cheek, together with plastic surgeons of the Department of Maxillofacial Surgery of the North-Western State University named after I.I. Mechnikov, a decision was made to perform an open combined intervention.
On 03/09/11, in the department of angiosurgery of the Road Clinical Hospital, an operation was performed: unilateral face-lifting with SMAS plication of the middle and lower zone of the face; removal of the cheek fat pad; EVLT of the residual area of hypervascular tissue (Fig. 4).
Rice. 4. Stages of the operation. Arrows indicate areas of hypervascular tissue
The main areas of hypervascularization, sclerosed and coagulated with a laser in the first stages, significantly simplified the intervention technique and made it possible to perform it almost bloodlessly.
The postoperative period was uneventful. The patient was discharged on March 23, 2011 with a good clinical result and cosmetic effect (Fig. 5).
Rice. 5. Photo of the patient after surgery
Histological conclusion: in the first tissue fragment there are fragments of fatty tissue with inclusions of fibrous and bone tissue. In the second tissue fragment there are many dilated capillaries and vascular cavities of various shapes and sizes. The walls of the cavities are lined with endothelium and separated by connective tissue septa.
Using this clinical observation as an example, we wanted to show the capabilities and effectiveness of various methods of vascular obliteration - laser, chemical and surgical - in the staged treatment of angiodysplasia. The presence in the surgeon’s arsenal of several complementary treatment methods allows one to achieve sufficient radicalism and a good cosmetic effect.
Causes
The specific causes, mechanism of occurrence and course of the disease have not been fully studied. Most researchers believe that this systemic vascular pathology is a consequence of congenital changes in the structure of elastic tissue. A deficiency of elastic fibers leads to a compensatory increase and proliferation of muscle and fibrous tissue.
Some doctors focus on the specific role of mechanical stress. An example is the development of characteristic degeneration of the renal artery due to tension in the vascular pedicle of the kidney due to its excessive pathological mobility - ptosis. But this conclusion remains quite controversial.
Introduction
Mitral valve dysplasia (used synonyms: prolapse, myxomatous transformation, degenerative mitral insufficiency) belongs to the group of hereditary connective tissue dysplasias, heterogeneous in their phenotypic manifestations. These systemic connective tissue diseases most often have an autosomal dominant type of inheritance of mutations that disrupt the synthesis and structuring of the fibrous proteins collagen and elastin and are referred to as Ehlers-Danlos syndrome. In cardiac surgery, these are primarily patients with aneurysms of large vessels, non-rheumatic mitral and aortic insufficiency, and non-coronary cardiomyopathies.
Dysplasia, which is based on genetically determined disorganization of the fibrous base of the mitral valve leaflets, meanwhile inevitably progresses with age. Most often, clinical manifestations of such mitral regurgitation with signs of central hemodynamic disturbances develop after the third and fourth decades of life [1].
The modern approach to the treatment of hereditary mitral valve dysplasia focuses on early surgical correction of the defect, before dilated remodeling of the left chambers of the heart and the development of secondary cardiomyopathy [2]. At the same time, the desire to preserve the patient’s own valve and avoid prosthetics is natural. The range of reconstructive surgical techniques from the period of the first developments in the 70-80s, made by A. Carpentier, and in our country B.A. Konstantinov, is expanding every year [1, 3, 4].
Reliability and durability of the reconstruction should be the main criteria when choosing a surgical technique: unreliable plastic surgery is worse than the modern prosthetic technique that remodels the subvalvular structures [7]. The purpose of this retrospective analysis is to develop an algorithm for choosing a surgical technique for operations in adult patients with mitral valve dysplasia.
Material and methods
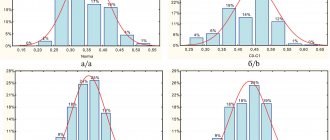
The group of patients selected for analysis of surgical tactics in the treatment of mitral valve dysplasia, complicated by hemodynamically significant mitral regurgitation, included 203 people operated on between July 1998 and July 2012. 92 operations were performed in the Department of Cardiovascular Surgery of the Russian Cardiological Scientific Center. - production complex (RKNPK) of the Ministry of Health of the Russian Federation and 111 operations - in the department of surgery of myocardial dysfunction and heart failure of the Russian Scientific Center for Surgery. The principles of treatment, tactics and surgical techniques were identical thanks to the work of one team of specialists.
Among those operated on there were 139 men and 64 women, with a predominance of young and middle-aged patients (from 20 to 75 years; on average 52.4 years). According to clinical symptoms, all patients were assigned to NYHA functional class III-IV.
Patients are divided into 2 groups. The main criterion for division is the nature of the surgical intervention on the mitral valve: valve-sparing repair (73 patients, or 36%) or universal chord-sparing replacement.
Fundamentally important during the operation were an accurate analysis and description of the anatomy of the mitral valve apparatus, as well as identification of the main causes of mitral regurgitation (Tables 1 and 2).
Just by comparing the causes of mitral regurgitation in the given tables, a significant difference is visible, which determined the choice of surgical tactics by the operating surgeon, striving for a reliable final result.
The type and volume of related operations are presented by group in Table. 3 and 4.
In the plastic reconstruction group, the AnnuloFlow semi-rigid support ring was always used (73 operations). The original technique of its implantation, used by the authors, consists of applying interrupted sutures without gathering in the area of the anterior leaflet and a continuous suture that reduces the size of the fibrous ring in the area of the posterior leaflet. Universal chord-sparing prosthetics is also an original technique that involves preserving four supporting chords along the anterior and posterior semicircle of the mitral valve fibrous annulus. The technique of these operations is described in detail in our earlier publications [1, 6].
For mitral replacement, only mechanical prostheses were used, which was primarily due to the relatively young age of the patients (Table 5).
All operations were performed under conditions of artificial circulation (28 °C) and cold cardioplegia with extracellular colloidal solution “Consol”.
Results and discussion
Overall hospital mortality was 2.46% (5 of 203 patients died). Accordingly, in the 1st and 2nd analyzed groups, failures were distributed as follows: in the group of plastic reconstructions on the mitral valve - 2.74% (2 out of 73 patients died), in the prosthetics group - 2.3% (3 out of 130 patients died). ). The causes of hospital mortality were different in both groups. In the 1st group, a 59-year-old patient, who, due to the separation of the chords of the posterior leaflet, underwent resection of the latter in the P2 zone, plastic surgery and implantation of the AnnuloFlow-32 support ring, on the 5th day after the operation, against the background of stable hemodynamics, a clinical picture of severe pseudomembranous colitis. Subsequently, severe hemolysis and acute renal failure occurred. Despite intensive plasma replacement and volumetric therapy, hemodialysis sessions, the patient died on the 9th day after surgery. Another patient in this group, 71 years old, also underwent resection and plastic surgery of the posterior leaflet due to chordal avulsion and implantation of the AnnuloFlow-34 support ring. For linear plastic surgery of the valve, Teflon gaskets were used. Due to progressive postoperative hemolysis, on the 5th day, a universal chord-sparing prosthetic operation (MIKS-29 disc prosthesis) was performed. The patient died on the 12th day due to symptoms of cardiopulmonary and renal failure.
In the 2nd group, a 54-year-old patient with distinct Ehlers-Danlos symptoms underwent mitral-aortic replacement (MIX-31 and MICS-25). In the post-perfusion period, uncontrolled bleeding developed from the aortic root along the suture line fixing the aortic prosthesis. A 70-year-old patient, who initially had mitral valve dysplasia with chordal avulsion and coronary heart disease, developed severe respiratory failure after the operation of universal chordal-sparing prosthetics with the ATS-28 prosthesis and 2-CABG. A 55-year-old patient diagnosed with secondary dilated cardiomyopathy (DCM) and avulsion of the anterior leaflet chords died on the 7th day after surgery for reverse cardiac remodeling due to medically uncontrolled arrhythmia and cardiovascular failure.
During the first year after surgery in group 1, one 64-year-old patient died, who had undergone plastic surgery 2.5 months earlier due to avulsion of the posterior leaflet chordae due to infective endocarditis. She died with symptoms of acutely developed mitral regurgitation; an autopsy revealed multiple avulsions of the chordae of the anterior leaflet. During a 14-year follow-up of patients in this group, there were no reoperations associated with recurrence of mitral regurgitation. One patient, 2 years after plastic surgery on the mitral valve, underwent tricuspid valve plastic surgery due to the progression of isolated (without pulmonary hypertension) tricuspid insufficiency. In group 2, the patient died after 3 years as a result of acutely developed (in sinus rhythm and adequate anticoagulant therapy) thrombosis of the Roscardix prosthesis.
Functional results were monitored for up to 10 years after surgery in 89 patients operated on in the Department of Cardiovascular Surgery of the Russian Republican Scientific and Pedagogical Research Center of the Ministry of Health of the Russian Federation (examination completeness 94.4%). The majority of patients (83.3%) corresponded to NYHA functional class I-II with an average follow-up of 6.9±2.4 years.
Thus, these results suggest the high effectiveness of surgical treatment of genetically determined mitral valve dysplasia. A prerequisite for such effectiveness, in our opinion, is a comprehensive surgical approach with correction of all accompanying changes and complications of mitral disease.
The choice of surgical tactics is largely determined by the accuracy of not only the anatomical, but also the etiological diagnosis of the defect. The main criteria for diagnosing mitral connective tissue dysplasia in our observations were clinical
(early diagnosed or suddenly appeared systolic murmur, supraventricular tachyarrhythmia, shortness of breath on exertion),
echocardiographic
(leaf prolapse, moderate fibrosis, malformed leaflets and subvalvular apparatus, chordal separation, enlargement of the left ventricle and atrium, regurgitation jet),
medical-genetic
(stigmata systemic connective tissue dysplasia: spinal scoliosis, excessive joint mobility, inguinal and umbilical hernias, visual impairment, heart rhythm disturbances, autonomic disorders, history of syncope and presyncope) and
histological
(fragmentation and disintegration of collagen and elastic fibers and their partial lysis, myxomatous transformation and decrease in the density of fibrous structures, fragmentation of the subendothelial elastic membrane, with long-term existence of the defect - the appearance of large areas of marginal fibrosis)
criteria.
Currently in the laboratory of medical genetics of the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky has created a Data Bank of biological samples from patients with connective tissue dysplasia syndrome and is searching for DNA mutations in the genes most often involved in the pathogenesis of the disease (M.D. E.V. Zaklyazminskaya, V.A. Rumyantseva).
Assessing the clinical condition of the patients we observed, who, as a rule, have signs of systemic circulatory decompensation, it should be noted that Russian cardiologists are late in referring patients with mitral valve dysplasia for surgical treatment. Compared to similar statistics from foreign clinics, in which operations in the case of mitral valve dysplasia are considered indicated already in functional class II according to the NYHA, our observations are dominated by patients with functional class III-IV. In 26 of the operated patients, the degree of decompensation and disturbances of intracardiac hemodynamics corresponded to the syndrome of secondary dilated cardiomyopathy with a decrease in the left ventricular ejection fraction to 20-25%, which forced us to solve a difficult problem: to offer patients reconstructive organ-preserving intervention or orthotopic heart transplantation. According to the initial severity of the patients' condition, the volume of surgical intervention significantly exceeded only surgery on the mitral valve.
Our experience allows us to say that all lesions of the tricuspid valve in the diagnosis of connective tissue dysplasia are of an independent organic nature and are not a consequence of mitral valve dysfunction: the degree of tricuspid insufficiency, as a rule, does not directly depend on the pressure in the pulmonary artery and on dilatation and insufficiency of the pumping function of the right ventricle. Therefore, all these patients who underwent mitral-tricuspid intervention have real two-valve heart defects. For patients in this group, suture annuloplasty according to De Vega should be performed with a rigid Etibond-2.0 thread.
When implanting artificial chordae in the position of the anterior leaflet, we obtained good functional results in 6 cases. However, for now we are cautious about the idea of expanding the indications for this type of chordal prosthetics in patients with signs of severe circulatory decompensation and concomitant cardiac diseases [5].
Thus, when assessing the results of surgical treatment of mitral valve dysplasia in adults in the Russian population, it should be noted that surgical treatment must be performed, as a rule, in patients with hemodynamically advanced defects and clinical symptoms of left ventricular failure. In such a situation, the choice of surgical technique and surgical intervention technique plays a decisive role in achieving an effective and reliable result. In each observation, we aimed to perform a reconstructive valve-sparing intervention, while keeping the reliability of the operation as the main priority [7].
By retrospectively analyzing the nature and extent of damage to the mitral valve apparatus and the type of surgery performed (plasty or prosthetics), we determined those factors that limit the possibilities of reliable reconstruction. With such structural and clinical features as avulsion of chords of the anterior cusp of the mitral valve, multiple avulsion of chords, excessive excess of cusps of the Burlow valve, two-valve mitral-aortic disease, progressive cardiomyopathy and dilatation of the heart cavities, secondary infective endocarditis, often more reliable, hemodynamically sound and effective is the operation of universal chord-preserving prosthetics. Like valve-sparing correction, due to the full functioning of the preserved native chordae, this operation provides close to natural mechanics of left ventricular contractions.
Absolutely reliable and durable in the long term, plastic reconstruction of the mitral valve with dilatation of the fibrous ring, moderate prolapse of the leaflets, partial separation of the chords of the posterior leaflet. To perform plastic surgery in risky situations, there must be compelling, primarily medical, reasons.
Information about authors
Sonkin I.N., Candidate of Medical Sciences, Head of the Department of Vascular Surgery of the National Healthcare Institution "Road Clinical Hospital" of JSC "Russian Railways", St. Petersburg.
Shaydakov E.V., Doctor of Medical Sciences, Professor, Deputy Director for Scientific and Clinical Work of the Federal State Budgetary Institution "Research Institute of Experimental Medicine" of the North-Western Branch of the Russian Academy of Medical Sciences, St. Petersburg. Mikhailov V.V., Candidate of Medical Sciences, Associate Professor of the Department of Maxillofacial Surgery, North-Western State University named after I.I. Mechnikov. Remizov A.S., Candidate of Medical Sciences, Deputy Chief Physician for Surgery of the National Healthcare Institution "Road Clinical Hospital" of JSC "Russian Railways", St. Petersburg. Krylov D.V., surgeon, department of vascular surgery, National Health Institution "Road Clinical Hospital" of JSC "Russian Railways", St. Petersburg. Chernykh K.P., surgeon, department of vascular surgery, National Health Institution "Road Clinical Hospital" of JSC "Russian Railways", St. Petersburg. The article was received on May 24, 2013.
Diagnosis of the disease
Mucosal dysplasia does not hurt, does not interfere with life - it has no symptoms.
The simplest way to detect pathology of the cervical mucosa was invented by Papanicolaou in the 1940s and consisted of taking scrapings of surface cells . Today, modified instruments are used to collect more material. Examination of cells under a microscope - cytology allows us to determine the next diagnostic stage - colposcopy.
Extended colposcopy - examination of tissues under high magnification from five to 30 times, with additional enhancement of the “picture” with special solutions, which helps in choosing the optimal place for taking a piece of tissue - a biopsy of the area of dysplasia. Pieces of mucous membrane measuring at least 3 millimeters are sent for microscopy - histology. A biopsy is excluded in case of inflammation and infections, but only temporarily.
Further, with morphological confirmation of dysplasia the mucous membrane of the cervical canal is scraped to identify its changes; in a woman, dysplasia can be localized in the glandular crypts - the pits of the mucosa and the epithelial transition zone can move higher. Curettage visualizes the pathological substrate hidden from the eye.