Home — For the public
- Map of medical organizations
- Vaccination
- Clinical examination
- Fluorography
- Addresses and opening hours of clinics
- Emergency rooms
- Oncology
- Where to take an HIV test
- Healthy child's office
- Services
- Prevention of CVD
- Disease Prevention
- World Patient Safety Day
- Newspaper "Medical News"
- specialist
- School of Health
— Disease prevention
- HIV infection
- All about vaccination
- All about proper nutrition
- Hepatitis
- Flu
- Dementia
- Schoolchildren's health
- STD
- Tick-borne encephalitis
- Whooping cough
- Measles
- Legionellosis
- Meningococcal infection
- Oncology
- Acute intestinal infection
- Pediculosis
- First aid
- Pneumococcal infection
- Pneumonia
- Prevention of rabies
- Dependency Prevention
- Rotavirus infection
- Diabetes
- Cardiovascular diseases
- Injuries
- Tuberculosis
- Tularemia
- Physical activity
- Obstructive pulmonary disease
- Exotic infections
- Ecology
- Why is swimming in ponds dangerous?
— Cardiovascular diseases — How stress and negative emotions affect the development of vascular diseases
They say: “all diseases are from nerves,” they warn: “don’t take it to heart,” or “it can break your heart.” The pathophysiological model describing how stress affects health was created by Hans Selye more than 60 years ago. How does the heart react to overstrain, unexpressed emotions, fears and doubts? And is it possible to somehow “tune it in a new way”?
Hans Selye's theory of adaptation to stress
What is stress? This is a set of normal reactions of the body that occur in response to the action of unfavorable factors. War, famine, epidemic, car accident, marriage, birth of a child - all this can become stressful.
The regulation of metabolism, physiological reactions, and behavior is carried out by a chain of hypothalamus, pituitary gland and adrenal glands. Corticotropic hormone of the hypothalamus stimulates the production of adrenocorticotropic hormone of the pituitary gland, which in turn triggers the secretion of cortisol.
Cortisol is a steroid hormone. It is synthesized in the adrenal cortex. Cortisol inhibits the breakdown of glycogen in muscles, activates it in the liver, and takes part in the development of the body's response to stress. How does he work? This hormone stimulates the sympathetic nervous system, giving impetus to any activity.
The concentration of cortisol in the blood changes throughout the day: it is maximum in the morning, when you need to get up and start doing something, and gradually falls during the day. In the evening, the level of the hormone in the blood is low, a person can relax and fall asleep. If he is busy with something important and interesting, then the adrenal glands secrete more cortisol than during routine activities.
What happens under stress? Cortisol levels increase. The hormone tells the body: “fight or flight.” The pulse quickens, blood pressure rises, muscles tense - the person is preparing for immediate decisive action.
This mechanism of adaptation to stress was discovered back in 1936. The author of the theory, biochemist Hans Selye described in detail how the body reacts to any strong stimulus, and introduced the concepts of eustress and distress. In the first case, the body is mobilized to complete the task, the person feels cheerful, active, and productive. And when the situation returns to normal, cortisol levels decrease. A person can “exhale and relax.”
Distress is chronic stress in which cortisol concentrations remain high. A person does not have time to recover and spends all the body’s resources on maintaining combat readiness. Everyday problems do not require “putting out fires and stopping horses in a gallop,” but they constantly keep you at a “low start,” preventing you from relaxing or reacting with your body to relieve tension. Cortisol levels are still high, and the circadian rhythms of its secretion are disrupted. So a person begins to sleep worse at night, body weight increases, blood pressure rises, and the ratio of cholesterol fractions changes.
Selye's triad, which describes this condition, includes 3 groups of symptoms:
- stomach ulcer;
- hypertrophy of the adrenal cortex
- atrophy of the thymus gland (thymus).
“If stress is excessive, it can lead to hypertension, asthma, irritable bowel syndrome,” says Ernesto Shiffrin, a professor in the Faculty of Medicine at McGill University, Montreal.
Causes of inflammation of the trigeminal nerve
Doctors believe that the main cause of inflammation of the trigeminal nerve is compression of it either inside the skull or outside it. Inside the skull, the trigeminal nerve can be compressed as a result of the formation of tumors, in most cases resulting from some kind of head injury.
Also a fairly common cause of inflammation of the trigeminal nerve is internal venous or arterial displacement.
Other causes of trigeminal neuralgia include:
- the presence of a chronic inflammatory process, viral or bacterial infection in the body;
- herpes infection (herpes);
- a brain tumor;
- scarring in the brain stem;
- failure of anesthesia during treatment or tooth extraction.
Most often, inflammation of the trigeminal nerve affects women at pre-retirement and retirement age (usually from fifty to seventy years). If trigeminal neuralgia is diagnosed in a young man or girl, then most likely its cause is a change in the arteries of a sclerotic nature or a strong dilatation of blood vessels.
Who handles stress worse?
Will everyone who is under acute or chronic stress “take it to heart” and develop chronic diseases? Psychologists and psychiatrists have been studying the causes of psychosomatic disorders for more than 50 years. Thus, American cardiologists Friedman and Rosenman in 1960 first described the traits of a person predisposed to coronary artery disease and called it “type A.” Scientists analyzed the incidence of the disease in people of both sexes in different countries. The study showed that in countries where heart attacks are more common in men than women, the behavior and lifestyle of patients had characteristic features:
- ambition and lack of flexibility. These qualities were combined with a high level of efficiency, a need for recognition, and a desire to compete with others even in situations where this was not so important;
- desire to control combined with impulsiveness. This led to attempts to work in several directions simultaneously;
- Difficulties in interpersonal relationships due to inflexibility and self-centeredness. Such people are easily offended, break ties if they cannot achieve what they want, and those around them do not want to “lose” to them;
- the desire to interrupt others and independently finish phrases in dialogue, the lack of “adjustment” to the interlocutor. Dramatic speech, high speed of associations;
- expressive facial expressions and gestures that often indicate muscle tension: gnashing of teeth, “chewing” movements of the lower jaw, clenched fists;
- sharp breathing with frequent sighs, demonstrative exhalations in conversation, designed to place emphasis;
- high speed of work and life, such people perform several tasks simultaneously, without counting their resources.
High sympathetic nervous system tone makes Type A people very sensitive to stress. Representatives of type B are not like that: they are in no hurry, lack the spirit of competition, can give in and not complete some things.
In general, cardiac risk is higher in older people, patients with concomitant diseases: myocardial infarction, coronary heart disease, transient ischemic attack (or stroke), diabetes mellitus, history of arterial damage. The situation is aggravated by hypercholesterolemia, excess weight, and bad habits. To predict the probability of disease, cardiologists use different scales.
Types of trigeminal neuralgia
Trigeminal neuralgia is divided into two types. The first, the so-called true trigeminal neuralgia, is a holistic disease caused in most cases by compression of the nerve or disruption of the blood supply. The second type - secondary trigeminal neuralgia - is a symptom of a general disease of the body. It could be a tumor or a serious infection.
In most cases, doctors diagnose inflammation of one of the processes of the trigeminal nerve, but in some situations inflammation of two or three processes occurs at once. Inflammation can affect either one side of the face or both, and in different combinations.
Stressors: Holmes and Ray model
“What will happen to him! Look how he holds up!” - this can be said about any unfamiliar person, and then you are surprised to find out that he is trying his best and has already suffered 2 heart attacks. Based on the time of action, psychogenic factors of CVD are divided into mental trauma and psychotraumatic situations. Injuries occur suddenly, a person is at the mercy of emotions and often does not have time to adapt (acute stress). Psychotraumatic situations exist for a long time, sometimes for years. At some stage, a person can adapt to them, but over time, compensatory mechanisms are exhausted. The disease develops.
How can you assess the strength of the negative influence and the body’s resource? According to the importance of the operating factor, life situations are assigned different numbers of points. In 1970, American psychiatrists T. Holmes and R. Ray analyzed people's reactions to significant events, ranked them and compiled a scale of stressors. The list includes not only obvious disasters, but also a large number of “ordinary” events and situations. The ten most important situations are listed below in descending order:
- death of a spouse or other closest person;
- divorce of spouses;
- separation of spouses (in marriage);
- imprisonment;
- death of one close family member;
- illness (injury);
- marriage;
- dismissal;
- reconciliation of spouses;
- termination of work upon retirement.
Fewer points are “given” for changing jobs, vacations, pregnancy, fines for minor offenses, and changing habits. In the Holmes and Ray scale there are only 43 event points that can pull the rug out from under your feet.
To assess the resource and likelihood of developing a nervous or psychosomatic disorder, the authors of the theory recommended noting the events that a person experienced during the year and summing up the points. A high score on the Holmes and Ray scale indicates that the subject has exhausted his resources and needs immediate help.
How to treat heart pain
The next night the same thing happened again, but it was all removed with tincture of valerian, motherwort and Corvalol. I took all this and glycine for 1-2 weeks. Feeling of suffocation pah-pah no. Then they came, 3 nights and my heart ached, it hurt in the heart area, as if there was a burning sensation and just a frantic heartbeat. There are still fears, which I all relieve with pills. I take Capoten in the morning for blood pressure, then for nerves 20 drops of Corvalol, 20 motherwort, 20 valerian and glycine, and all this 3 times a day. But sometimes I still had body aches, terrible fatigue, drowsiness during the day, periodically I felt pain in my heart or pain in my chest and the feeling that I would definitely fall on the street. Of course, I myself am a heart patient, but all this is strange. My cardiologist says it's not his and referred me to a neurologist. Of course, I don’t want to offend medicine, I know that all doctors are different, and there are those who save lives, but my clinic is more like sitting through the torment of queues, and receiving, excuse me, delirium that you are not coming to me. I don’t want to torture myself, not understanding who to go to, a therapist or a neurologist, and I’m afraid that I’ll be looking for a toilet at the clinic faster than looking for a doctor.”
Treatment of heart pain
The psychotherapist diagnosed the presence of astheno-depressive syndrome.
A comprehensive course of therapy was carried out for one month.
After treatment, the patient does not complain about heart pain, fears or other negative symptoms. It is recommended to consult a psychotherapist once every 3 months for a year. It is recommended to follow a daily routine and diet; if the condition worsens, contact a psychotherapist. No relapses have been observed for 3 years from the end of treatment.
Complaints of heart pain
2. Patient: Male; 43 years old, smokes – 1 pack a day, alcohol – moderate, on holidays, drugs – no. Married, two children, resident of a big city. He was observed for a long time by a cardiologist for heart pain and hypertension. I got an appointment with a psychotherapist by chance.
Description of the situation by the patient himself:
“About seven years ago, I began to experience rapid heartbeat: my pulse reached 120, it was pulling in my left shoulder and along my ribs, the pain was not severe, but aching. I periodically feel an increase or decrease in heart rate. I just bent over on the street, and after I straightened up I felt a painless movement in my chest, like a cramp, but somewhere inside. He immediately took the pulse on the carotid artery and did not feel it. Panic and dizziness immediately set in; after the panic attack, the heart rate, not urgently, slowly began to increase in frequency, although it was really scary. I was next to you and decided to come in and take your blood pressure. (BP - 152/100).
Self-medication of heart pain is unacceptable
Usually, in such situations, I take Valocordin and lie down. But the feeling of fatigue and heaviness in the body does not leave. A diagnosis of second-degree hypertension, ventricular extrasystole, and incomplete blockade of the left bundle branch of His was made. They prescribed sedatives, Concor and something else, a whole handful, I can’t remember exactly now, I have it written down. But the heart still sometimes begins to pound strongly in the chest, which causes pain. The pulse quickens and there is aching pain in the shoulder.” The patient's blood pressure was measured and an ECG was taken at the time of the attack. No cardiac pathology was detected. Complaints of severe heart pain and dizziness did not go away.
Reaction to stress
Stressful situations can unfold quickly (acute stress) or “undermine” a person’s health day after day (chronic stress). In the first case, the body's reaction may manifest itself in the form of takotsubo stress cardiomyopathy or the so-called “broken heart syndrome”. With this disease, the heart muscle temporarily loses its ability to contract, the apex of the left ventricle expands, and the thickness of the wall decreases. A person may die from a dangerous arrhythmia, wall rupture, or heart failure.
Chronic stress affects more than just your heart and blood pressure levels. It changes behavior, disrupts the functioning of the endocrine glands, which collectively leads to serious consequences. If acute stress either kills a person or makes it possible to survive the situation and try to move on, then chronic overstrain often seems to push one to drink alcohol and smoke. These addictions and other bad habits associated with them change lifestyle and further worsen the condition of patients.
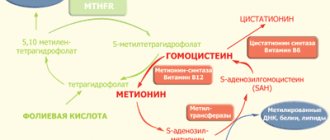
Prolonged nervous tension can trigger the following changes:
- To “calm down,” a person begins to consume sweets, baked goods, and other high-calorie foods.
- A high content of trans fats and animal fats disrupts the balance between the fractions of good and bad cholesterol, and atherosclerosis progresses.
- High-calorie foods with a high glycemic index can provoke insulin resistance and lead to type 2 diabetes, a complication of which is damage to small vessels.
- The persisting “combat” concentration of cortisol also negatively affects carbohydrate metabolism.
- Body weight increases and the load on the cardiovascular system increases. Hypertension occurs.
- The walls of blood vessels become denser and their lumen narrows. The likelihood of a stroke or heart attack increases.
How to recognize someone who will cope worse with stress and negative emotions? It is worth paying attention to the following destructive traits in his behavior:
- works too much;
- tries to “take on” and heroically solve too many problems;
- cannot get enough sleep regularly, sometimes forgets to sleep;
- has difficulty making important decisions, hesitates;
- often rushes, but cannot do the job well enough;
- eats food to relax and calm down;
- drinks and/or smokes;
- eats food very quickly;
- irritable, speaks quickly.
If you notice such personality traits in yourself or a loved one, you should take care of your health in advance: learn to “let go” of events, take your time, and not “eat and wash down” stress.
Don't worry?
Today, specialists understand that it will not be possible to ignore the psychological state of cardiac patients. And also that it is pointless to urge a person to calm down. According to statistics, Russians are among the most anxious people in Europe, and our country is also among the most depressed.
In cases where anxiety and depression are severe (often after cardiac accidents), the attending physician may prescribe the patient antidepressants or anti-anxiety medications. Before this or in parallel with taking medications, psychotherapy is used.
If anxiety and depression are not too severe, correction begins with non-drug methods. This can be done on your own, including for people who do not yet have heart problems. Learn relaxation techniques and stress relief. Active physical exercise helps suppress it - do it whenever possible.