General information
Hypovolemic shock is a pathological condition that develops under the influence of a decrease in the volume of circulating blood in the bloodstream or fluid deficiency (dehydration) in the body. As a result, stroke volume and the degree of filling of the ventricles of the heart decrease, which leads to the development of hypoxia , tissue perfusion and metabolic . Hypovolemic shock includes:
- Hemorrhagic shock, the development of which is based on acute pathological loss of blood (whole blood/plasma) in a volume exceeding 15-20% of the total bcc (circulating blood volume).
- Non-hemorrhagic shock, developing due to severe dehydration of the body caused by uncontrollable vomiting, diarrhea , and extensive burns.
Hypovolemic shock develops mainly with large losses of fluid from the body (with pathological loose stools, loss of fluid through sweat, uncontrollable vomiting, overheating of the body, in the form of clearly imperceptible losses). According to the mechanism of development, it is close to hemorrhagic shock, except that fluid in the body is lost not only from the vascular bloodstream, but also from the extravascular space (from the extracellular/intracellular space).
The most common occurrence in medical practice is hemorrhagic shock (HS), which is a specific response of the body to blood loss, expressed by a complex of changes with the development of hypotension , tissue hypoperfusion , small output syndrome , hemocoagulation , impaired permeability of the vascular wall and microcirculation, multisystem/multiple organ failure.
The triggering factor for HS is pathological acute blood loss, which develops when large blood vessels are damaged as a result of open/closed trauma, damage to internal organs, gastrointestinal bleeding, pathologies during pregnancy and childbirth.
Lethal outcome from bleeding occurs more often as a result of the development of acute cardiovascular failure and much less often due to the loss of blood of its functional properties (impaired oxygen-carbon dioxide metabolism, transfer of nutrients and metabolic products).
Two main factors play a role in the outcome of bleeding: the volume and rate of blood loss. It is generally accepted that an acute simultaneous loss of circulating blood in a short period of time in a volume of about 40% is incompatible with life. However, there are situations when patients lose a significant amount of blood due to chronic/recurrent bleeding, but the patient does not die. This is due to the fact that with minor one-time or chronic blood loss, the compensatory mechanisms existing in the human body quickly restore blood volume/circulation speed and vascular tone. That is, it is the speed of implementation of adaptive reactions that determines the possibility of preserving/maintaining vital functions.
There are several degrees of acute blood loss:
- I degree (BCC deficiency up to 15%). Clinical symptoms are practically absent, in rare cases - orthostatic tachycardia , hemoglobin more than 100 g/l, hematocrit 40% or higher.
- II degree (BCC deficiency 15-25%). Orthostatic hypotension, blood pressure decreased by 15 mm Hg. or more, orthostatic tachycardia, heart rate increased by more than 20/minute, hemoglobin level 80-100 g/l, hematocrit level 30-40%.
- III degree (BCC deficiency 25-35%). There are signs of peripheral dyscirculation (pronounced pallor of the skin, cold extremities to the touch), hypotension (systolic blood pressure 80-100 mm Hg), heart rate exceeds 100/minute, respiratory rate more than 25/minute), orthostatic collapse , decreased diuresis (less 20 ml/h), hemoglobin within 60-80 g/l, hematocrit - 20-25%.
- IV degree (BCC deficit more than 35%). There is impaired consciousness, hypotension (systolic blood pressure less than 80 mm Hg), tachycardia (heart rate 120/minute or more), respiratory rate more than 30/minute, anuria; hemoglobin is less than 60 g/l, hematocrit is less than 20%.
The degree of blood loss can be determined based on various direct and relative indicators. Direct methods include:
- Calometric method (weighing of spilled blood by colorimetry).
- Gravimetric method (radioisotope method, polyglucinol test, determination using dyes).
To indirect methods:
- Algover shock index (determined using a special table based on the ratio of pulse rate and systolic pressure).
Based on laboratory or clinical indicators, the most accessible of which are:
- Based on blood specific gravity, hemoglobin content and hematocrit.
- By changes in hemodynamic parameters (BP and heart rate).
The amount of blood loss during injuries can be determined approximately and by the location of the damage. It is generally accepted that the volume of blood loss from rib fractures is 100-150 ml; for a fracture of the humerus - at the level of 200-500 ml; tibia - from 350 to 600 ml; hips - from 800 to 1500 ml; pelvic bones within 1600-2000 ml.
Signs of hypovolemic shock
Obvious symptoms of this condition develop with a loss of 10-20% of the blood volume. Early signs of hypovolemic shock include:
- thirst;
- anxiety, irritability;
- pale skin covered with sticky sweat;
- decreased blood pressure, rapid breathing;
- dizziness;
- confusion (not always).
In the absence of adequate medical care, the patient's condition worsens and late symptoms develop: a sharp decrease in blood pressure, severe tachycardia, decreased temperature, dizziness, loss of consciousness.
Treatment of hypovolemic shock is usually carried out by a resuscitator in collaboration with specialized specialists. Therapy is aimed at eliminating respiratory and circulatory hypoxia and ensuring sufficient blood supply to organs, as well as restoring circulating blood volume.
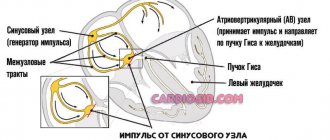
Pathogenesis
The main factors in the development of hemorrhagic shock include:
- Severe deficit of blood volume with the development of hypovolemia , which leads to a decrease in cardiac output.
- Decreased oxygen capacity of the blood (oxygen delivery to cells and reverse transport of carbon dioxide decreases. The process of delivery of nutrients and removal of metabolic products also suffers).
- Hemocoagulation disorders that cause disorders in the microvasculature - a sharp deterioration in the rheological properties of blood - increased viscosity (thickening), activation of the blood coagulation system, agglutination of blood cells, etc.
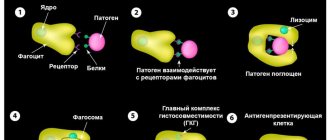
hypoxia occurs , often of a mixed type, capillarotrophic insufficiency, causing dysfunction of organs/tissues and disruption of the body's vital functions. Against the background of disruption of systemic hemodynamics and a decrease in the intensity of biological oxidation in cells, adaptation mechanisms are turned on (activated) aimed at maintaining the vital functions of the body.
Adaptation mechanisms primarily include vasoconstriction (vasoconstriction), which occurs due to activation of the sympathetic part of neuroregulation (release of adrenaline , norepinephrine ) and the action of humoral hormonal factors (glucocorticoids, antidiuretic hormone, ACTT, etc.).
Vasospasm helps to reduce the capacity of the vascular bloodstream and centralize the circulatory process, which is manifested by a decrease in the volumetric velocity of blood flow in the liver, kidneys, intestines and vessels of the lower/upper extremities and creates preconditions for further disruption of the function of these systems and organs. At the same time, the blood supply to the brain, heart, lungs and muscles involved in the act of breathing continues to remain at a sufficient level and is the last thing to be disrupted.
This mechanism, without pronounced activation of other compensation mechanisms in a healthy person, is capable of independently neutralizing the loss of about 10–15% of the bcc.
The development of severe ischemia of a large tissue mass contributes to the accumulation of under-oxidized products in the body, disturbances in the energy supply system and the development of anaerobic metabolism. adaptive response to progressive metabolic acidosis , since they contribute to more complete utilization of oxygen by various tissues.
Relatively slowly developing adaptive reactions include fluid redistribution (its movement into the vascular sectors from the interstitial space). However, this mechanism is realized only in cases of slowly occurring minor bleeding. Less effective adaptive responses include increased heart rate (HR) and tachypnea .
Developing cardiac/respiratory failure is leading in the pathogenesis of acute blood loss. Volumetric bleeding leads to decentralization of the systemic circulation, an extreme decrease in the oxygen capacity of the blood and cardiac output, irreversible metabolic disorders, “shock” organ damage with the development of multiple organ failure and death.
In the pathogenesis of hypovolemic shock, it is necessary to take into account the role of the developing imbalance of electrolytes, in particular, the concentration of sodium ions in the vascular bed and extracellular space. In accordance with their concentration in the blood plasma, isotonic type of dehydration (at normal concentration), hypertonic (increased concentration) and hypotonic (decreased concentration) type of dehydration are distinguished. Moreover, each of these types of dehydration is accompanied by specific shifts in plasma osmolarity, as well as extracellular fluid, which has a significant impact on the nature of hemocirculation, the state of vascular tone and cell functioning. And this is important to consider when choosing treatment regimens.
Therapy for hypovolemic shock
Hypovolemia requires immediate treatment. The patient is usually hospitalized in the intensive care unit, where complex therapy will be carried out aimed at restoring circulating blood volume, normalizing blood circulation in vital organs (brain, heart, lungs, kidneys) and restoring the acid-base balance. For this purpose, infusion therapy, blood replacement drugs, glucocorticosteroids, and sedatives are prescribed. In parallel, oxygen inhalations are carried out, and if necessary, the patient is transferred to mechanical ventilation.
Emergency care for hypovolemic shock before the ambulance arrives:
- In an unconscious state, a person must be placed on his back and his head turned to the side (in the absence of damage to the cervical spine);
- raise your legs 30 cm;
- cover with a blanket (to avoid hypothermia).
Clinical recommendations for providing first aid for hypovolemic shock in children are identical to those described above.
Classification of hemorrhagic shock
The classification of hemorrhagic shock is based on the stage of development of the pathological process, according to which there are 4 degrees of hemorrhagic shock:
- First degree shock (compensated reversible shock). It is caused by a small amount of blood loss, which is quickly compensated by functional changes in the work of cardiovascular activity.
- Shock of the second degree (subcompensated). Developing pathological changes are not fully compensated.
- Third degree shock (decompensated reversible shock). Disturbances are expressed in various organs and systems.
- Fourth degree shock (irreversible shock). It is characterized by extreme depression of vital functions and the development of irreversible multiple organ failure.
The importance of fluid in human physiology
Water is part of the entire complex of fluids that wash organs and tissues. It is the main component of blood, lymph, cerebrospinal and interstitial fluid, secretions of the salivary glands, gastric and other juices produced by internal organs, tears, and urine.
Liquid creates a universal internal environment for the existence of cells. Through it the following is carried out:
- nutrition and removal of toxins;
- “orders” are delivered from the nervous and endocrine centers;
- the necessary brain structures are excited.
The role of liquid in ensuring metabolic processes is great. All biochemical reactions take place only in dissolved form. By changing the amount of water in the body in accordance with physiological needs, the required concentration of salts, electrolytes, acids and alkalis, biological substances, everything that ensures the internal environment or homeostasis is maintained.
The preservation of homeostasis indicators is guaranteed by natural tissue barriers (skin, mucous membranes of organs and blood vessels). Equilibrium can change under the influence of regulatory systems, but within very narrow limits.
Therefore, any disturbances in the composition of liquid media can be used to judge the pathology that has arisen. A decrease in fluid causes significant changes in homeostasis: some substances are lost along with water, others sharply increase in concentration. Pathophysiological disorders may concern:
- cellular composition of blood;
- alkaline balance;
- concentration of dissolved substances.
The functional capacity of systems depends on the norms of water distribution in the body.
Changed conditions cause many diseases.
In humans, it is convenient to judge the volume of fluid by the indicator of circulating blood. It is calculated in the laboratory. A decrease of 25% in healthy people is well compensated and does not cause any significant changes in homeostasis. 90% of the blood is in the vascular bed, the rest is deposited in the spleen and bones. If necessary, it is thrown out of storage and replenishes losses.
Large losses lead to varying degrees of hypovolemia, and in the absence of compensation and assistance - to a hypovolemic shock state.
Causes
The most common causes of hemorrhagic shock are:
- Injuries - damage (fractures) to large bones, injuries to internal organs/soft tissues with damage to large vessels, blunt trauma with rupture of parenchymal organs (liver or spleen), rupture of an aneurysm of large vessels.
- Diseases that can cause blood loss are acute gastric/duodenal ulcers , cirrhosis of the liver with esophageal varices, infarction/ lung gangrene , Mallory-Weiss syndrome, malignant tumors of the chest and gastrointestinal tract, hemorrhagic pancreatitis and other diseases with a high risk of rupture of blood vessels vessels.
- Obstetric bleeding that occurs when a tube ruptures/ectopic pregnancy, abruption/ placenta previa , multiple pregnancy, cesarean section, complications during childbirth.
First aid to the victim
Since the disease in question is a rather insidious pathology that can have fatal consequences, it is imperative to understand the algorithm for providing emergency care:
- The patient is placed on any hard surface.
- Place a pillow under your feet so that they are higher than head level.
- The pulse is checked. If the person is unconscious, place him on his side with his head thrown back.
- It is better to undress and cover with a blanket.
- If the spine is broken, it is best to keep the patient face up.
- If there is open bleeding, all measures should be taken to stop it. This is done by clamping the vessel over the injury and applying a splint or tourniquet.
- An antiseptic bandage is applied to the wound.
- If necessary, it is recommended to give the victim pain medication.
Only a specialist can take further action.
Symptoms
The clinical picture of hemorrhagic shock develops in accordance with its stages. Clinically, signs of blood loss come to the fore. At the stage of compensated hemorrhagic shock, consciousness, as a rule, does not suffer, the patient notes weakness, may be somewhat agitated or calm, the skin is pale, and the extremities are cold to the touch.
The most important symptom at this stage is the desolation of the subcutaneous venous vessels in the arms, which decrease in volume and become thread-like. The pulse is weak and rapid. Blood pressure is usually normal, sometimes elevated. Peripheral compensatory vasoconstriction is caused by overproduction of catecholamines and occurs almost immediately after blood loss. Against this background, at the same time the patient develops oliguria . At the same time, the amount of urine excreted may be reduced by half or even more. Central venous pressure decreases sharply, which is due to a decrease in venous return. In compensated shock, acidosis is often absent or local in nature and mildly expressed.
At the stage of reversible decompensated shock, the signs of circulatory disorders continue to deepen. In the clinical picture, which is characterized by signs of the compensated stage of shock (hypovolemia, pallor, profuse cold and sticky sweat, tachycardia, oliguria), the main cardinal symptom is hypotension , which indicates a disorder in the circulatory compensation mechanism. It is in the stage of decompensation that organ circulatory disorders (in the intestines, liver, kidneys, heart, brain) begin. Oliguria, which in the compensation stage develops as a result of compensatory functions, at this stage occurs on the basis of a decrease in hydrostatic blood pressure and renal blood flow disorders.
At this stage, the classic clinical picture of shock appears: acrocyanosis and coldness of the extremities, increased tachycardia and the appearance breath , dullness of heart sounds, which indicates a deterioration in myocardial contractility. In a number of cases, there is a loss of individual or a whole group of pulse impulses in the peripheral arteries and the disappearance of heart sounds during deep inspiration, which indicates an extremely low venous return.
The patient is inhibited or in a state of prostration. Shortness of breath and anuria develop . DIC syndrome is diagnosed. Against the background of the most pronounced vasoconstriction of peripheral vessels, direct discharge of arterial blood into the venous system occurs through opening arteriovenous shunts, which allows increasing oxygen saturation of the venous blood. At this stage, acidosis is pronounced, which is a consequence of increasing tissue hypoxia .
The stage of irreversible shock is not qualitatively different from decompensated shock, but is a stage of even more pronounced and profound disorders. The development of a state of irreversibility is manifested by a matter of time and is determined by the accumulation of toxic substances, the death of cellular structures, and the appearance of signs of multiple organ failure. As a rule, at this stage there is no consciousness, the pulse in the peripheral vessels is practically not determined, blood pressure (systolic) is at the level of 60 mm Hg. Art. and lower, difficult to determine, heart rate at 140/min., breathing is weakened, rhythm is disturbed, anuria. There is no effect from infusion-transfusion therapy. The duration of this stage is 12-15 hours and ends in death.
Tests and diagnostics
The diagnosis of hemorrhagic shock is established based on examination of the patient (presence of fractures, external bleeding) and clinical symptoms reflecting the adequacy of hemodynamics (color and temperature of the skin, changes in pulse and blood pressure, calculation of the shock index, determination of hourly diuresis) and laboratory test data, including: determination CVP, hematocrit , blood CBS (indicators of acid-base status).
Establishing the fact of blood loss due to external bleeding does not present any difficulties. But in its absence and suspicion of internal bleeding, it is necessary to take into account a number of indirect signs: in case of pulmonary hemorrhage - hemoptysis; for stomach and duodenal ulcers or intestinal pathology - vomiting “coffee grounds” and/or melena; in case of damage to parenchymal organs - tension of the abdominal wall and dullness of percussion sound in the sloping parts of the abdomen, etc. If necessary, instrumental studies are prescribed: ultrasound, radiography, MRI, laparoscopy, consultations with various specialists are prescribed.
It should be borne in mind that the assessment of the volume of blood loss is approximate and subjective, and if it is assessed inadequately, you can miss the permissible waiting interval and find yourself faced with the fact that a picture of shock has already developed.
Diagnostic methods
In addition to a standard examination by a medical specialist, it is possible to prescribe additional examinations to diagnose the disease. These:
- Blood analysis.
- Echocardiography.
- Endoscopy.
- ULTRA-HEARING.
- CT scan.
- Catheterization of the heart and urinary tract.
Depending on the accompanying symptoms, the following may be used:
- daily blood pressure monitoring;
- stool analysis;
- X-ray of the pelvis;
- Chest X-ray.
During pregnancy
Hemorrhagic shock in obstetrics, which occurs during pregnancy, during labor, as well as in the early/late afterbirth period, is one of the significant causes in the structure of maternal mortality, accounting for about 20–25%. The rate of obstetric hemorrhage relative to the total number of births varies between 5-8%.
The specifics of bleeding in obstetrics are:
- The suddenness of their appearance and massiveness.
- High risk of fetal death, which necessitates urgent delivery until stable stabilization of hemodynamic parameters and completion of infusion-transfusion therapy in full.
- Combination with pronounced pain syndrome.
- Rapid depletion of compensatory and protective mechanisms. At the same time, the risk is especially high in pregnant women with late gestosis and in women with complicated labor.
The permissible blood loss during childbirth during its normal course should not exceed 250-300 ml (approximately 0.5% of a woman’s body weight). This amount of blood loss refers to the “physiological norm” and does not negatively affect the condition of the woman in labor. The main causes of acute pathological blood loss during pregnancy with the development of hemorrhagic shock are: ectopic pregnancy , placental abruption/previa, multiple pregnancy, complications during childbirth, cesarean section, uterine rupture.
Features of hemorrhagic shock in obstetric pathology include: its frequent development against the background of a severe form of gestosis in pregnant women, the rapid development of hypovolemia , disseminated intravascular coagulation syndrome, arterial hypotension , and hypochromic anemia .
In case of HS, which developed in the early postpartum period against the background of hypotonic bleeding, a short period of unstable compensation is characteristic, after which irreversible changes quickly develop (persistent hemodynamic disturbances, DIC syndrome with profuse bleeding, respiratory failure and impaired blood coagulation factors with activation of fibrinolysis).
Factors in the development of the condition
In medicine, there are 4 main common factors that contribute to the occurrence of hypovolemic shock:
- Accumulation of a large amount of blood in the capillaries. It can be observed in pathologies of an infectious nature, as well as in traumatic shock.
- As a result of injury or other serious pathologies, irreversible loss of plasma occurs. This may be due to extensive burns of the body, as well as the formation of fluid in the peritoneum and intestines.
- Bleeding in a severe form, in which it is impossible to restore blood loss.
- A significant amount of isotonic fluid is lost due to prolonged vomiting or diarrhea.
A special role is played by the accumulation of free blood in peripheral capillaries. This condition is common in certain types of infections. In such cases, the patient may experience several types of shock as a result of various factors.
List of sources
- Bratus V.D., Sherman D.M. Hemorrhagic shock, pathophysiology and clinical aspects. Kyiv: Nauk. Dumka. 1989.
- Gakaev D. A. Pathophysiological changes in the body during acute blood loss [Text] // Medicine and healthcare: materials of the IV International. scientific conf. (Kazan, May 2021). - Kazan: Buk, 2016. - pp. 37-40.
- Vorobyov A.I., Gorodetsky V.M., Shulutko E.M., Vasiliev S.A. Acute massive blood loss. M.: GEOTAR-MED, 2001.
- Bryusov P.G. Emergency infusion-transfusion therapy for massive blood loss / P.G. Bryusov // Hematology and transfusiology. –1991. – No. 2. – P. 8-13.
- Stukanov M.M. Comparative assessment of infusion therapy options in patients with hemorrhagic shock / M.M. Stukanov et al. //Anesthesiology and resuscitation. – 2011. – No. 2. – P. 27-30.