The heart valve system ensures the directed release of blood from one chamber to another, into the main vessels. The correct distribution of flow and the strength of myocardial contractions depend on the synchronous opening and closing of the valves. Through the aorta, blood enriched with oxygen and nutrients enters the general circulation.
Failure of the aortic valve leads to heart failure and is accompanied by impaired organ function.
Congenital bicuspid aortic valve (synonym - bicuspid aortic valve), according to its clinical manifestations, is not a harmless condition, but poses a risk of complications.
Inflammatory and atherosclerotic changes in the valves cause narrowing (stenosis) of the opening and varying degrees of insufficiency. The development of echocardiography has made it possible to identify pathology in childhood and determine early indications for aortic valve replacement.
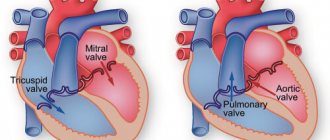
Anatomical structure
The valve is located at the border of the aorta and left ventricle. Its main function is to prevent the return of blood flow to the ventricle, which during systole has already passed into the aorta.
The valve structure consists of:
- fibrous ring - a strong connective tissue formation that clearly separates the left ventricle and the initial part of the aorta;
- three semilunar valves - represent a continuation of the endocardial layer of the heart, consist of connective tissue and muscle bundles of fibers, the distribution of collagen and elastin allows them to close tightly, block the lumen of the aorta and redistribute the load on the vessel walls;
- sinuses of Valsalva - located behind the aortic sinuses, immediately behind the semilunar valves, from which the bed of the right and left coronary arteries begins.
The parts of the valve are connected to each other by adhesions (commissures)
Violation of the structure leads to a picture of a congenital defect (CHD) or acquired nature. Congenital heart disease is detected in a child during the neonatal period based on symptoms and auscultation.
How does the aortic valve work?
The tricuspid structure of the aortic valve is distinguished from the bicuspid mitral valve by the absence of papillary muscles and tendon chords. Therefore, it opens and closes only under the influence of the difference in pressure in the cavity of the left ventricle and the aorta.
During opening, elastin fibers from the ventricle press the valves against the walls of the aorta, opening the hole for blood flow. At the same time, the aortic root (the initial part) contracts and pulls them towards itself. If the pressure in the ventricular cavity exceeds the pressure in the aorta, then blood flows into the vessel.
The valves close with swirling currents in the area of the sinuses. They move the valve away from the walls of the aorta towards the center. Elastic flaps close tightly. The closing sound is heard with a stethoscope.
Congenital changes in the aortic valve
The exact causes of congenital disorders are still unknown. More often it occurs simultaneously with another congenital heart disease - the mitral valve.
The most common developmental defects:
- formation of two leaflets rather than three (bicuspid aortic valve);
- one of the sashes is larger than the others, stretches and sags;
- one valve is smaller than the others, underdeveloped;
- holes inside the doors.
Aortic valve insufficiency ranks second in frequency after mitral valve defects. Usually combined with stenosis of the aortic lumen. More often found in boys.
Diagnosis of aortic valve diseases
Both types of diseases are diagnosed in similar ways. During the consultation, the doctor collects personal and family history. This is followed by an echocardiogram, a test that uses sound waves to create an image of the heart and aortic valve. Chest X-rays are also widely used to diagnose aortic valve disease.
If the diagnostic tests performed do not provide a definitive diagnosis, the doctor may suggest cardiac catheterization. During the procedure, a dye is used to allow the specialist to see any leaks from the heart valve. The dye is injected through a vein in the groin or arm, and then a monitor tracks the movement of the dye through the blood through the heart.
Acquired vices
The causes of acquired defects are severe chronic diseases, so they often develop in adulthood. The greatest connection has been established with:
- rheumatism;
- septic conditions (endocarditis);
- previous pneumonia;
- syphilis;
- atherosclerosis.
The nature of pathological changes is different:
- With rheumatic lesions, the valves are soldered at the base and wrinkled.
- Endocarditis deforms the valves, starting from the free edge. Here, warty growths are formed due to the proliferation of colonies of streptococci, staphylococci, and chlamydia. Fibrin is deposited on them and the leaflets fuse together, losing the ability to completely close.
- With atherosclerosis, the lesion passes from the aortic wall, the valves thicken, fibrosis develops, and calcium salts are deposited.
- Syphilitic changes also spread to the valves of the aorta, but are accompanied by the death of elastic fibers and expansion of the fibrous ring. The valves become dense and inactive.
The causes of the inflammatory process can be autoimmune diseases (lupus erythematosus), chest injuries.
In older people, atherosclerosis of the aortic arch leads to expansion of the root, stretching and sclerosis of the valves.
Pathological changes in damage to the aortic valves
The result of congenital and acquired changes is the formation of insufficient closure of the valves, this is expressed in the return of part of the blood to the cavity of the left ventricle when it relaxes. The cavity expands and lengthens in size.
Forced intensification of contractions causes, over time, a breakdown of compensatory mechanisms and hypertrophy of the muscular layer of the left ventricle. This is followed by dilation of the left venous opening connecting the ventricle to the atrium. Overload from the left sections is transmitted through the pulmonary vessels to the right heart.
The impaired ability of the valve leaflets to close tightly leads to the formation of insufficiency and prolapse under the influence of reverse blood flow. Usually, aortic stenosis occurs simultaneously. In the clinical picture we can talk about the predominance of one type of defect. Both increase the load on the left ventricle of the heart. Features of the course must be taken into account when choosing a treatment method.
Introduction
Many researchers of sclerodegenerative aortic disease, according to their ideas about its pathophysiology, give different definitions to the disease: “cyanocyanic aortic stenosis”, “Mönckeberg disease”, “calcified aortic valve stenosis of sclerodegenerative origin”, “degenerative defect”, “age-related involution-calcium degeneration of the aortic valve”. valve." These names do not contradict each other, but rather are complementary, however, according to the latest literature data [9, 11, 13, 16, 18, 22], we will call this nosological form of aortic heart disease sclerodegenerative.
As a special form of aortic heart disease in elderly patients, it occurs quite often and by the age of 70 it is the main one [4, 8, 9, 13, 16].
In recent years, the structure of heart valve diseases has changed significantly and sclerodegenerative lesions of the aortic valve apparatus have taken first place in prevalence. The changes in the structure of valvular heart lesions are based on an increase in the life expectancy of the population and a decrease in the incidence of rheumatism [2, 13, 18].
According to the definition of researchers of this problem [8, 10, 12, 13, 16, 20], aortic heart disease of sclerodegenerative etiology can be diagnosed in patients aged 65 years and older who did not suffer from rheumatism, congenital aortic heart disease, or primary infective endocarditis.
Sclerodegenerative aortic valve disease is a fairly common disease. In industrialized countries, aortic valve damage ranks third, second only to coronary heart disease and arterial hypertension [9].
Patients in the older age group often suffer from atherosclerotic coronary disease, requiring myocardial revascularization. At the same time, the aging of the population increases the risk of developing aortic heart disease of sclerodegenerative origin in combination with atherosclerotic lesions of the coronary bed. The combination of aortic heart disease with coronary lesions in this category of patients has long ceased to be exclusive.
It is known that myocardial revascularization in the older age group when correcting aortic valve disease may be required in 45% of patients or even more [3, 6, 7]. The frequency of stenotic lesions of the coronary bed in the group of patients with sclerodegenerative lesions of the aortic valve varies from 35 to 65% [3, 6, 7, 12, 13, 24].
Hospital mortality after intervention on the aortic valve and coronary bed remains quite high and ranges from 5 to 11% [1, 3, 6, 7, 17].
Taking into account the above, we present our own experience of surgical treatment of patients with aortic disease of sclerodegenerative origin and coronary heart disease, and the identified features of the postoperative period.
Material and methods
The study included patients aged 65 years and older who, according to the anamnesis (and intraoperative findings), did not suffer from congenital heart disease, rheumatism, primary infective endocarditis, or who had atherosclerotic lesions of the coronary bed, dictating the need for myocardial revascularization.
At the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky, from 1994 to 2009, 54 patients aged 65 to 88 years (average age 68.4±5.9 years) were operated on for aortic heart disease of sclerodegenerative origin in combination with coronary heart disease.
In total, during this period, 89 patients were operated on for aortic heart disease of sclerodegenerative origin, of which 34 (38.2%) did not require coronary artery bypass grafting, since atherosclerotic lesions of the coronary bed were not diagnosed or there were hemodynamically insignificant stenoses (less than 60% of the vessel diameter ).
The condition of the majority of patients (88.9%) belonged to NYHA functional class (FC) IV. Men predominated - 47 (87%). 2 (3.7%) patients had previously suffered acute myocardial infarction. The mean left ventricular ejection fraction was 51.8±9.3%. The mean systolic gradient between the left ventricle and the aorta was 56.3 ± 27.8 mm Hg.
Clinical manifestations of IHD were observed in 45 (83.3%) patients. Extreme degree of calcification of the aortic valve (III degree according to the classification of the Scientific Center for Cardiovascular Surgery named after A.N. Bakulev, IV degree - according to B.A. Konstantinov) was noted in 48 (88.9%) cases.
Concomitant diseases are presented in the table.
Most often, patients suffered from arterial hypertension, chronic obstructive pulmonary diseases, multifocal atherosclerosis and varicose veins of the lower extremities.
According to the preoperative examination, calcification of the ascending aorta was diagnosed in 18 (33.3%) patients.
Atrial fibrillation upon admission was recorded in 5 (9.3%) patients, one of them had previously been implanted with a permanent pacemaker.
All surgical interventions were performed from a longitudinal median sternotomy in moderate hypothermia (from 28 to 32 °C). Cardioplegic solutions of St. Thomas, Consol, and Custodiol were used.
Aortic valve replacement in combination with coronary bypass surgery was performed in 50 patients. Due to an organic defect of the mitral valve (myxomatous degeneration of the leaflets), as well as widespread calcification with organic damage to the mitral valve, replacement of the mitral and aortic valves was performed in 3 patients. Replacement of the ascending aorta using the Bentall-De Bono technique with coronary bypass grafting was performed in one patient. In one observation, due to hemodynamically severe stenosis of the carotid artery, aortic valve replacement with coronary artery bypass grafting was supplemented with carotid endarterectomy from the left common carotid artery. Plastic surgery of the aortic root with a patch of xenopericardium using the Nix method was performed in 1 patient and in 3 cases it was performed for the purpose of suturing the aortotomy incision after decalcification of the surrounding tissues due to their rigidity.
In total, in 54 observations, 106 distal anastomoses with the coronary bed were formed, thus, the myocardial revascularization index was 1.9. In 19 (35.2%) cases, one coronary artery was bypassed, in 22 (40.7%) - two, in 9 (16.7%) - three, in 4 (7.4%) cases - four. The left internal mammary artery was used in 72.2% of cases. The reasons for refusing to use it were significant stenotic lesions of the left subclavian artery, as well as unsatisfactory blood flow through the artery after its isolation. Proximal anastomoses (n=36) on the clamped aorta were performed in 25 (69.4%) cases, and with lateral compression of the aorta - in 11 (30.6%) cases.
Mechanical prostheses were implanted in the position of the aortic valve in 37 (68.5%) cases, and biological ones in 17 (31.5%) cases.
The average duration of artificial circulation was 104.3±33.1 minutes (56-224 minutes), myocardial anoxia - 80.4±22.1 minutes (49-173 minutes), artificial ventilation - 12.4±7.3 hours (from 7.5 to 46 hours).
Results and discussion
Non-lethal complications (heart failure) were noted in 11 (20.3%) cases. Rhythm and conduction disturbances were recorded in 10 (18.5%) patients: paroxysms of atrial fibrillation - atrial flutter - in 6, transient atrioventricular block requiring temporary cardiac pacing - in 4. In 4 cases, the rhythm was restored with medication, in 2 cases cardioversion was performed. Subsequently, one patient was implanted with a permanent pacemaker system due to the development of sick sinus syndrome.
Respiratory failure requiring prolonged artificial ventilation and/or sessions of the recruiting maneuver “opening the lungs” followed by sessions of non-invasive mask ventilation was observed in 10 (18.5%) cases. Renal failure occurred in 4 (7.4%) patients. In one observation, 3 sessions of ultrahemodiafiltration were performed with complete restoration of renal function.
As for complications from the central nervous system, neurological dysfunction was noted in 5 (9.2%) cases: in 1 - dynamic cerebrovascular accident with complete regression of neurological symptoms even at the hospital stage and the absence of pathological changes according to computed tomography of the brain, in 4 (7.4%) there were signs of encephalopathy (short-term psychomotor agitation or retardation), which required a course of appropriate complex therapy.
It should be noted that out of 25 cases in which distal anastomoses were formed on the clamped aorta, neurological dysfunction occurred in 2 (8%), in a group of 11 patients after lateral compression of the aorta - in 3 (27.3%).
Suppuration of soft tissues was observed in 3 (5.6%) patients, bleeding requiring resternotomy was observed in 1 patient.
Hospital mortality was 3.7% (2 patients). In one observation, after replacement of the aortic and mitral valves and bypass of two arteries, complex conduction and rhythm disturbances developed in the immediate postoperative period, which led to the development of fibrillation and ineffective hemodynamics, which was the cause of death. In another observation, after aortic valve replacement and bypass surgery of two arteries, the cause of death was increasing cardiovascular failure.
Acquired valvular heart defects are the main cause of disability and premature death of patients worldwide [2, 9, 13, 16]. The relevance of the problem of sclerodegenerative aortic stenosis is due to the aging population, the high prevalence of this disease in the elderly, deteriorating quality of life, poor prognosis and high mortality of patients if surgical intervention is not performed [18]. The prevalence of aortic stenosis is 3-7%; among patients 80 years of age and older, its frequency increases to 15-20% [8, 9, 12, 16, 22]. Currently, in developed countries, sclerodegenerative aortic heart disease is the most common heart valve disease and ranks third among all cardiovascular diseases after arterial hypertension and coronary heart disease [11, 14, 16]. Sclerodegenerative aortic stenosis, regardless of severity, leads to an increased risk of myocardial infarction, cerebrovascular accident, heart failure and sudden death [4, 8, 9].
The history of studying sclerodegenerative lesions of the aortic valve dates back to 1904, when J. Monckeberg [19] described 2 observations of stenosis of the aortic mouth with significant calcification of the valves. It has long been believed that calcified aortic stenosis in the elderly is the result of a nonspecific, age-related degenerative process that develops as a result of “age-related wear” of the valve leaflets with passive deposition of calcium on them. This hypothesis has undergone significant changes in the last decade. Currently, epidemiological and experimental data have been obtained that the development of sclerodegenerative aortic stenosis is the result of an active cellular biological process in which lipoproteins accumulate in the valve leaflets, signs of an active inflammatory process, neurohormonal activation and endothelial dysfunction are determined. The active process of calcification leads to the subsequent formation of mature bone tissue in the valve leaflets [8, 9, 18, 20, 21].
Sclerodegenerative aortic stenosis is the result of a genetically determined immune-mediated inflammatory process in the leaflets of the aortic valve, usually leading after 60 years to pathological fibrosis and/or ectopic ossification of the leaflets, in which compaction and calcium weighting of the leaflets cause obstruction of the outflow tract without the primary formation of commissural adhesions [8, 9, 20, 21].
We should not forget that with aortic stenosis, significant hypertrophy of the left ventricular myocardium develops. In this context, work in recent years has forced a new assessment of the role of dysmetabolic processes in the heart muscle [8, 9]. Oxygen in the cardiomyocyte is sequentially used in two processes - β-oxidation of fatty acids and two-stage glycolysis. Under conditions of hypertrophy, oxygen is not enough to carry out the final stages of glycolysis: the oxidative decarboxylation of pyruvic acid is inhibited, which halves the synthesis of ATP and provokes an increased formation of membrane-damaging protons. After the addition of myocardial ischemia, which is an indispensable companion to the disease in question, a reorientation of energy metabolism in cardiomyocytes from glycolysis to β-lipid oxidation is observed, inevitably leading to the development of intracellular lactic acidosis. This process turns out to be key in the development of heart failure in hemodynamically significant aortic stenosis, especially in combination with coronary lesions [8, 9, 12, 13, 15]. That is why the condition of the majority of patients we observed belonged to NYHA FC IV.
The predominance of NYHA FC IV in our observations is explained by the elderly age of the patients, as well as concomitant diseases, among which the dominant role is played by arterial hypertension, chronic obstructive pulmonary diseases, and atherosclerotic lesions of various vascular systems.
There are similarities between vascular atherosclerosis and sclerodegenerative aortic stenosis: common clinical risk factors (age, arterial hypertension, smoking, hyperlipidemia, etc.) [8, 9, 16, 20-22], as well as morphological features (infiltration by macrophages and lymphocytes, deposition lipoproteins, foci of calcification). It is still not uncommon for a diagnosis to be formulated as “atherosclerotic stenosis of the aortic mouth,” but the question of whether the development of sclerodegenerative aortic stenosis in elderly patients is a sign of an atherosclerotic process remains controversial.
It should be noted that, unlike atherosclerosis, there is currently no convincing evidence of a cause-and-effect relationship between clinical factors and calcific aortic valve disease. The relationship between aortic sclerosis and age has been shown to be non-linear, with a clear increase in disease prevalence in men aged around 65 years and in women aged around 75 years [8, 20–22]. In addition, sclerodegenerative aortic stenosis does not develop in all elderly people, while half of the population over 80 years of age does not have characteristic changes in the aortic valve [8, 18, 20].
The association of risk factors for cardiovascular diseases with aortic stenosis is partly explained by the presence of concomitant coronary heart disease in patients with aortic stenosis [1, 3, 6, 7, 12, 13, 15, 20]. Convincing evidence that atherosclerosis and sclerodegenerative aortic stenosis are different diseases is the discrepancy between the severity of damage to the aortic valve and changes in the coronary arteries - only about 40% of patients with aortic stenosis have severe coronary heart disease, and vice versa, most patients with severe coronary artery disease never aortic stenosis does not develop [13].
According to some researchers, the prevalence of coronary heart disease in patients with aortic stenosis and typical angina ranges from 40 to 50%, in the presence of atypical chest pain - 25%, in the absence of chest pain - 20% [3, 6, 7, 18]. Even in patients under 40 years of age with aortic stenosis, without chest pain and without risk factors for coronary heart disease, coronary atherosclerosis is detected in 3-5% of cases, not to mention patients over 65 years of age with sclerodegenerative aortic valve disease [14].
It is known that angina pectoris may not always be an indicator of coronary damage in the presence of aortic stenosis. Only about half of these patients with the classic clinical picture of angina have significant damage to the coronary arteries. In most patients, myocardial ischemia is caused by overload of the left ventricle, which is explained by increased tension of its wall, hypertrophy and changes in microcirculation in the subendothelial layers of the left ventricular myocardium. At the same time, 14% of patients with aortic stenosis have lesions of the left main coronary artery or three-vessel lesions without angina [15]. In our study, lesions of the left main coronary artery or three-vessel lesions without angina pectoris were rare - in 5.6% of cases.
The natural course of aortic stenosis in elderly patients is characterized by a rather long latent period. The clinical picture of the disease manifests itself at the stage of severe damage to the aortic valve. With aortic stenosis, blood flow from the left ventricle to the aorta is hampered, as a result of which the systolic pressure gradient between the left ventricle and the aorta increases significantly. It usually does not exceed 30 mmHg, but can reach 100 mmHg. and more [4, 7, 12, 13, 18, 20]. Due to the increase in afterload of the left ventricle, its hypertrophy develops, which depends on the degree of narrowing of the aortic opening. So, if normally the area of the aortic opening is about 3 cm, then its reduction by half causes a pronounced hemodynamic disturbance. Particularly severe violations occur when the hole area decreases to 0.5 cm2. End-diastolic pressure may remain normal or increase due to impaired relaxation of the left ventricle, which is associated with its severe hypertrophy. Due to the great compensatory capabilities of the hypertrophied left ventricle, cardiac output remains normal for a long time, although during exercise it increases to a lesser extent than in healthy individuals [3, 4, 7, 13].
Clinical manifestations of the disease, in addition to angina, are signs of heart failure and/or often syncope. This signals that the course of the defect is entering a critical period, since after the manifestation of these symptoms, the average life expectancy is 2-3 years. Approximately one third of asymptomatic patients experience sudden death [4, 7, 8, 13, 16].
The incidence of stenotic lesions of the coronary arteries in patients with sclerodegenerative aortic valve disease varies depending on age. Significant damage to the coronary arteries (60% or more of the vessel diameter) is observed in 30-50% of patients, whose average age is 60-70 years. Such a lesion is registered in more than 50% of patients under the age of 75 years and in 41-65% of patients over 75 years of age [3, 7, 15]. According to our data, significant damage to the coronary bed in aortic disease of sclerodegenerative origin was noted in 60.7% of cases.
Statistics indicate that aortic valve insufficiency is less likely to be combined with coronary heart disease, especially compared to aortic stenosis. Among patients who underwent aortic valve replacement, the percentage of patients with aortic insufficiency is relatively small (does not exceed 10-25% of the total number of patients with aortic valve defects and coronary heart disease) [3, 7].
The main feature of aortic valve insufficiency, which essentially determines the entire pathophysiology of this disease, is an increase in the volume load on the left ventricle with its subsequent dilatation. Enlargement of the left ventricular cavity, as a rule, does not occur suddenly. The exception is patients with acute aortic regurgitation, who have severe symptoms associated with a sudden increase in left ventricular end-diastolic pressure and a decrease in effective cardiac output to the peripheral vasculature. At the same time, we must not forget that ischemic dysfunction of the left ventricle can also lead to an increase in its size [3, 4, 11].
The disease in patients with aortic heart disease, including sclerodegenerative origin, and coronary heart disease can occur in one of the following three scenarios [3]:
- aortic valve disease may be asymptomatic and discovered by chance during an examination for symptomatic coronary heart disease;
- without any symptoms, while the presence of a murmur over the aorta, detected during a routine medical examination, prompts additional examination and diagnosis of coronary heart disease;
- the disease may be detected relatively late, when the natural history of aortic valve disease leads to heart failure due to left ventricular overload (pressure or volume) and/or ischemic damage.
The presence of a long latent period, as mentioned above, during which the severity of hemodynamic obstruction of the left ventricular outflow tract gradually increases, makes it difficult to diagnose this disease in the early stages. Thus, at the outpatient stage, only every third patient with stenosis is diagnosed with calcified aortic valve stenosis of degenerative origin. The difficulty of diagnosis is also due to the low specificity of symptoms and their blurred nature in older people. In addition, the presence of other associated conditions, such as coronary heart disease, chronic heart failure, arterial hypertension, and their prevalence in elderly people make it difficult to correctly interpret echocardiographic data [9].
Overall hospital mortality during surgical treatment of combined lesions of the aortic valve and coronary bed ranges from 4.3-5.7% [14, 23] to 11-10.6% [6, 7]. Even balloon coronary angioplasty with stenting followed by aortic valve replacement does not allow achieving a hospital mortality rate below 8.3-7.8% [3, 7]. In our study, the mortality rate was 3.7%.
Since the group of patients we observed falls under the World Health Organization definition of “elderly and senile” age (65 years and older), there are features that must be taken into account during treatment [5]: the presence of concomitant diseases of organs and systems, decreased strength characteristics and elasticity tissues, extreme degree of calcification of the valve apparatus/annulus fibrosus, long-term restoration of muscle tone in the early postoperative period, long recovery period after surgery, delayed tissue repair.
This explains the fact that the average duration of mechanical ventilation in the early postoperative period was 12.4 hours. Often, due to the spread of calcifications to the aortic wall, mitral valve, or the formation of an aneurysm of the ascending aorta, it was necessary to expand the scope of surgical treatment: decalcification of surrounding tissues and the mitral valve, plastic surgery aortic root with xenopericardium or synthetic patch, replacement of the ascending aorta, which increases the duration of artificial circulation and myocardial anoxia.
Thus, in Russia, little attention has been paid to the study of aortic defect of sclerodegenerative origin in combination with coronary heart disease, which means that the practicing physician is not focused on the appropriate diagnostic search. At the same time, the rather rare diagnosis of atherosclerotic stenosis of the aortic mouth due to a lack of understanding of the true nature of the defect leads to the fact that the patient is more often prescribed a diet and cholesterol-lowering drugs than referred for a consultation with a cardiac surgeon. Such “pathogenetic treatment” only leads to the progression of petrified stenosis, which increases the risk of sudden death. Conservative symptomatic tactics in patients with aortic stenosis are generally ineffective, and even more so in patients with calcified aortic stenosis, not to mention the presence of hemodynamically significant lesions of the coronary bed.
In other words, refusal to interpret sclerodegenerative calcified stenosis of the aortic mouth as “atherosclerotic” will lead Russian cardiologists and therapists to form a completely definite view of the treatment prospects for such patients. Surgical treatment is recognized as the only effective treatment worldwide: aortic valve replacement (as a method with the best long-term survival rates) in combination with myocardial revascularization for ischemic disease or the use of balloon valvuloplasty.
In this report, we presented our small experience in the surgical treatment of aortic disease of sclerodegenerative origin in combination with coronary heart disease, however, we believe that the low hospital mortality rate, as well as the small number of complications, give reason to recommend a more aggressive approach when determining indications for surgical treatment of this severe group patients.
Of course, the question of the possibility of large-scale surgical intervention in elderly patients with aortic valve disease in combination with coronary heart disease is very relevant at the present time. The risk of peri- and postoperative complications increases with age, the severity of hemodynamic disorders, as well as the volume of surgical intervention, therefore the decision to perform surgical treatment in each specific observation must be made taking into account the individual risk, benefit and prospects for improving the quality of life in the future.
Place of the bicuspid valve among aortic defects
The incidence of bicuspid aortic valve detection among children reaches 20 cases per thousand newborns. In adults it is 2%. For most people, two valves are enough to ensure normal blood circulation throughout a person’s life and do not require treatment.
On the other hand, when examining children with congenital heart disease in the form of aortic stenosis, up to 85% of cases reveal a variant of the bicuspid aortic valve. In adults, similar changes are found in half of the cases.
The “throughput” area of the aortic opening depends on the options for valve fusion.
Usually one of the two valves is larger than the other, the opening has an asymmetrical appearance like a “fish mouth”
If the congenital pathology of heart disease is “layered” with causes of an infectious nature, atherosclerosis of the aorta, then the valves fail faster than usual and undergo fibrosis and calcification.
What causes aortic valve disease and who is affected by it?
Aortic stenosis
One of the common causes of aortic stenosis is congenital heart disease. The aortic valve consists of three triangular cusps called petals. During normal operation of the valve, the petals close tightly and prevent blood from flowing in the opposite direction. If there is a congenital defect, the aortic valve may have only one or two leaflets instead of three. This type of aortic stenosis can be completely asymptomatic until adulthood, after which signs of narrowing or blood leakage begin to appear.
Calcium accumulation on the valve leaflets can also cause aortic stenosis. Calcium deposits cause hardening of the lobes and narrowing of the aortic valve. This form of the disease usually appears in older people.
Rheumatism and scarlet fever can also be causes of aortic stenosis, since they often leave scars on the aortic valve, which lead to its narrowing. Scar tissue can also lead to calcium deposits on the surface of the valve leaflets.
Aortic valve insufficiency
Aortic valve insufficiency occurs for the same reasons as aortic stenosis, but can sometimes be due to simple tissue wear and tear. The aortic valve opens and closes thousands of times a day, so over time, natural wear and tear can cause abnormalities and backflow of blood into the left ventricle.
Endocarditis is an infection of the heart valves that can cause aortic valve regurgitation. Also, sexually transmitted diseases, such as syphilis, can (in rare cases) damage the heart valves. Even more rarely, valve damage is a side effect of a spinal disorder called ankylosing spondylitis.
How does valvular insufficiency manifest?
Symptoms of incomplete closure of the aortic valve begin to appear if the reverse flow of ejected blood reaches 15–30% of the volume of the ventricular cavity. Before this, people feel good, even play sports. Patients complain about:
- heartbeat;
- headaches with dizziness;
- moderate shortness of breath;
- feeling of pulsation of blood vessels in the body;
- angina pain in the heart area;
- tendency to faint.
With decompensation of the cardiac adaptation mechanisms, the following appears:
- dyspnea;
- swelling in the limbs;
- heaviness in the hypochondrium on the right (due to stagnation of blood in the liver).
During the examination, the doctor notes:
- pale skin (reflex spasm of peripheral small capillaries);
- pronounced pulsation of the cervical arteries and tongue;
- change in pupil diameter in accordance with the pulse;
- In children and adolescents, the chest protrudes due to strong heartbeats into the non-ossified sternum and ribs.
Intensified beats are felt by the doctor when palpating the heart area. Auscultation reveals a typical systolic murmur.
Blood pressure measurement shows an increase in the upper number and a decrease in the lower one, for example, 160/50 mmHg. Art.
The role of valves in the formation of aortic stenosis
With repeated rheumatic attacks, the aortic valves shrink, and the free edges become so welded together that they narrow the outlet. The fibrous ring becomes sclerotic, further increasing the stenosis.
Symptoms depend on the degree of narrowing of the opening. A critical stenosis is considered to be a diameter of 10 mm2 or less. Depending on the area of the free aortic opening, it is customary to distinguish between the following forms:
- light - more than 1.5 cm2;
- moderate - from 1 to 1.5 cm2;
- severe - less than 1 cm2.
Patients complain about:
- pain similar to angina attacks is caused by insufficient blood flow into the coronary arteries;
- dizziness and fainting due to brain hypoxia.
Signs of heart failure appear in the event of decompensation.
During the examination, the doctor notes:
- pale skin;
- palpation is determined by a shift to the left and down the apex impulse, “trembling” at the base of the heart on exhalation, like a “cat’s purr”;
- hypotension;
- tendency to bradycardia;
- typical sounds on auscultation.
Aortic valve disease: features of its course and treatment
According to statistics, disorders of the cardiovascular system have become increasingly observed in people over 30 years of age. There are many reasons that provoke pathologies. If some diseases are treatable and, by removing provoking factors, one can achieve normalization of health, then others accompany the patient throughout his life and can significantly shorten his life.
Aortic valve disease is a serious pathology. More often requires surgical intervention. It can be congenital or acquired. Appears as a result of narrowing of the aortic mouth or incomplete closure of its valve.
Causes and symptoms
There are no exact statistics on the prevalence of the disease by age group and gender, but cardiologists note that it is detected several times more often in women than in men. The peak number of patients is observed among people of older retirement age. The main reasons may be:
- leaflet calcification;
- progression of rheumatism;
- idiopathic dilatation of the aorta;
- arterial hypertension and endocarditis;
- aneurysm;
- congenital defect of the aortic valve.
Chest trauma, arthritis, syphilis and some pathologies that develop in a person over a long period of time can also give impetus to the appearance or progression of disruption of the normal functioning of the organ.
8
24/7
Degrees
The risk to the patient's health and the need for surgery depends on the degree of aortic regurgitation.
| Stage | Amount of thrown blood, % | Prosthetics |
| First, full compensation | no more than 15 | Not required |
| Second, hidden CH | from 15 to 30 | Required under certain conditions |
| Third, relative coronary insufficiency | up to 50 | |
| Fourth, severe left ventricular failure | more than 50 | |
| The issue is resolved individually | Not required due to its uselessness. |
Depending on the degree, the valves are deformed and the quantitative volume of blood entering the heart through the aorta changes. The initial, first stage of the disease is virtually impossible to determine. The patient’s symptoms are completely absent or feel like side effects of other diseases. This occurs because the heart adjusts to the change in volume and compensates for it.
Symptoms
As the pathology develops, the organ ceases to cope with its functions, and symptoms characteristic of aortic valve disease appear:
- tinnitus and dizziness when moving or changing position;
- increased heartbeat, pronounced pulsation in the blood vessels;
- shortness of breath, fatigue, fainting and pre-fainting states, nausea;
- a pressing feeling of heaviness in the right hypochondrium, as well as swelling of the lower extremities;
- coughing attacks when lying down, standing, feeling of constant weakness.
Due to a lack of oxygen, a person’s complexion becomes pale gray, a bluish tint to the lips is observed, and typical circles appear under the eyes. Also, when examining a patient, the cardiologist examines the presence and severity of symptoms:
- the difference between the upper and lower blood pressure readings;
- pulsation on the carotid arteries, uvula and tonsils;
- reaction of the pupils to heart contractions, heart murmurs;
- changes in the size of the organ, protrusion in the chest area.
Diagnostics
Accurate diagnosis of the disease can only be made on the basis of objective data, a complete cardiac examination, biochemical blood test and a number of other tests.
Based on the presence of clinical symptoms, the severity of the defect, and the severity of aortic insufficiency, a decision about surgery is made. In elderly patients, due to the low contractility of the organ, the functional impairment is almost invisible. The severity of the pathology can be determined after studying the area of the hole in relation to the blood flow. Arterial insufficiency is determined by the indicator of reverse blood flow.
By listening, a cardiologist can determine the onset of development of bicuspid aortic valve disease:
- with stenosis, a systolic murmur is characteristic with a weakening of the 2nd tone in the aorta;
- Insufficiency is indicated by a murmur during diastole.
It is necessary to study the functioning of the heart by:
- ECG;
- X-ray examination;
- MRI to exclude coronary insufficiency and other pathologies.
However, the basis for choosing treatment is echocardiography.
When diagnosing, an accurate description of the patient’s feelings is of great importance, so before the appointment, you can write down all the complaints and let the doctor read them.
8
24/7
Treatment at different stages
Depending on the cause, extent, stage of aortic valve disease and other factors, different treatment methods may be used. The patient must be regularly observed by a specialist and undergo the examinations prescribed by him. In the absence of obvious symptoms:
- mild defect – once every 3 years;
- moderate form – once every 24 months;
- severe degree - annually, sometimes more often.
The following medications are prescribed:
- rheumatic nature of the disease - antibiotics;
- arterial hypertension - to normalize blood pressure.
Surgical intervention is not required, only constant monitoring by the attending physician is required.
If clinical complaints appear, to alleviate the patient’s condition in the preoperative period or if surgery is impossible, the following is prescribed:
- inhibitors, diuretics, nitrates;
- vasodilators and beta blockers;
- drugs that improve blood circulation.
A timely operation can help completely get rid of aortic valve disease. When blood reflux in an amount not exceeding 30% and slight deformation of the valves, intra-aortic balloon counterpulsation is recommended. In case of severe structural changes that allow more than 30% blood flow, implantation is required.
Surgery
In a person with heart disease, the bicuspid aortic valve requires replacement or replacement in several cases.
| Diagnosis | Cause |
| Severe stenosis | Complaints of severe pain and worsening condition. |
| Associated ischemia requiring coronary artery bypass grafting. | |
| Additional pathological changes in the organ requiring surgical intervention. | |
| The ejection fraction with cardiac contractility is below 50%. | |
| Severe valvular insufficiency | Clinical manifestations of the disease. |
| Surgery is required for other diseases of the organ. | |
| A decrease in ejection fraction in the absence of complaints from the patient. | |
| Too much enlargement of the ventricles. |
Surgical intervention is mainly performed after 30-35 years, but with the accelerated development of the disease it can take place at any time. The number of contraindications to prosthetics is minimal. They are:
- decompensated diabetes;
- oncological diseases;
- post-stroke condition;
- exhaustion and anemia.
For each patient, his condition is predicted at the time of the operation and during the rehabilitation period. Depending on this, a conclusion is given about the possibility of returning to normal life.
Forecast
The construction of treatment plans for the disease and the choice of methods occurs after diagnosis and identification of the severity of the aortic valve defect.
Mild hypertrophy with strong obstruction of blood flow leads to a decrease in the number of heart contractions and, accordingly, gradually reduces the therapeutic effect of surgery.
The process of hypertrophy allows, at a certain stage of the disease, to stabilize the functioning of the heart, but at the same time it can cause the development of angina pectoris and increase the likelihood of a heart attack.
If aortic heart valve disease developed asymptomatically, and then its rapid progression began, then the subsequent life expectancy of a person is no more than 3 years.
Risk factors and disease prevention
Aortic valve defects can be divided into 2 groups.
| View | Development time | Cause |
| Congenital | During intrauterine development of the fetus at 2-8 weeks of formation. | Genetic predisposition. Radiation exposure, rubella and other viral infections. Smoking, alcohol and drug addiction of the mother. |
| The defect becomes noticeable as the child grows. | The presence of a muscle cushion above the AC. The valve design is two- or single-leaf rather than three-leaf. Under the valve there is a membrane with a hole. | |
| Acquired | Any age | Infectious diseases that lead to microorganisms entering the organ. The subsequent appearance of a colony of connective tissue at the site of localization leads to deformation of the valves. |
| Autoimmune diseases become an impetus for the fusion of pouches and changes in the aortic mouth. | ||
| Age-related disorders, mainly calcification of the edges of the valves and the growth of fatty plaques, lead to closure of the lumen. |
There are no preventive measures that guarantee complete protection against the disease, but the following help reduce the risk:
- timely treatment of streptococcal infections;
- if you have rheumatism, constant monitoring by a specialist;
- taking certain groups of antibiotics and other drugs prescribed by a cardiologist;
- complete exclusion of alcohol, drugs and smoking;
- engaging in acceptable forms of exercise.
Aortic valve disease needs to be treated using scientific methods of therapy. Traditional methods do not have the desired effect and can lead to missed deadlines when the disease can be cured. Therefore, in case of any deviations, medical attention is needed.
8
24/7
Survey data
On an x-ray (including fluorography), the expansion of the aortic arch and enlarged left and right ventricles are clearly visible.
ECG - shows a shift to the left of the electrical axis, signs of myocardial hypertrophy, extrasystoles are possible.
Phonocardiographic signs allow you to objectively examine heart murmurs.
Ultrasound or echocardiography - indicates an enlargement of the left ventricle, most accurately characterizes the pathology of the valves (changes in structure, flutter of the valves, width of the residual opening).
Dopplerography is the most informative
The Doppler ultrasound method allows:
- see the return flow of blood;
- diagnose the degree of valve prolapse (internal deflection);
- establish the compensatory capabilities of the heart;
- determine indications for surgical treatment;
- assess the severity of stenosis by violation of the normal pressure gradient (from 3 to 8 mm Hg).
In the functional diagnosis of aortic stenosis using Dopplerography, it is customary to take into account the following gradient deviations (differences between pressure in the aorta and left ventricle):
- mild stenosis - less than 20 mm Hg. Art.;
- moderate - from 20 to 40;
- severe - over 40, usually 50 mmHg. Art.
The development of heart failure is accompanied by a decrease in the gradient to 20.
A type of echocardiography, the transesophageal version, is carried out by inserting a special sensor with an esophageal probe closer to the heart. It makes it possible to measure the area of the aortic annulus.
By catheterizing the chambers of the heart and blood vessels, the pressure in the cavities is measured (along the gradient) and the characteristics of the blood flow are studied. This method is used in specialized centers for diagnosis in people over 50 years of age, if it is impossible to decide otherwise on the method of surgical intervention.
Congenital defects are suggested to be operated on after 30 years of age, earlier - only with rapid decompensation
Aortic stenosis (narrowing of the aorta)
Aortic stenosis is a narrowing of the opening through which blood flows from the left ventricle of the heart into the aorta.
What is aortic stenosis?
Aortic stenosis can be congenital (due to disruption of the formation of the aortic valve during intrauterine development) and acquired (due to the effects of pathological processes, that is, diseases).
Aortic stenosis can be valvular or subvalvular. Valvular stenosis is the type of aortic stenosis in which the lumen of the aortic valve narrows. Subvalvular stenosis is called a stenosis caused by a narrowing of the outflow tract of the left ventricle under the aortic valve due to thickening of the muscular septum, or the presence of a membrane.
Why does it arise?
Normally, the aortic valve has 3 thin cusps, which, when opening, allow blood from the heart to the internal organs, and when closing, prevent blood from getting back into the heart and overloading it.
Quite often, as a result of a violation of intrauterine development, the aortic valve from birth may have only 2 leaflets, this leads to accelerated “aging” of the valve with the formation of a narrowing of its lumen.
Everyone knows such a disease as atherosclerosis; it affects the vessels of all organs, as well as some structures of the heart. The aortic valve is an intravascular formation as it is located in the lumen of the main artery of the body, the aorta. When atherosclerotic plaques develop on the aortic valve, thickening of the leaflets may occur. Thickened valves lose elasticity and become covered with calcium salts, which narrows the lumen.
Who can get sick
The disease is typical for patients of any age. Children are born with a bicuspid aortic valve, which makes them sick from birth. Subvalvular membrane is also a congenital defect. ( Any age )
Atherosclerosis progresses with age in all people, causing the gradual formation of aortic stenosis in a certain proportion of the population. ( Most typically from 45 to 70 years old )
A special group consists of elderly people in whom the function of the aortic valve arises as a result of its aging along with the entire body. ( Over 60 years old )
Subvalvular aortic stenosis often develops in women with a rare hereditary disease - hypertrophic cardiomyopathy. ( Ages 12 years and older, women are affected )
Anyone who has long-term high blood pressure and does not receive proper treatment can develop thickening of the heart muscle (myocardial hypertrophy), which can cause partial blockage of blood flow from the heart. ( Ages 35 and older )
What are the symptoms of the disease?
Aortic stenosis is an insidious disease. For a long time, no symptoms may appear at all; this is due to the compensatory capabilities of the body.
The following complaints are typical for this disease:
- Shortness of breath with little physical activity (people around you may notice that you get tired faster)
- Heartbeat
- Interruptions in heart function
- Pain in the heart area during exercise and at rest
- Dizziness when changing body position, or physical effort, stress.
- Late stages of the disease are characterized by sudden attacks of loss of consciousness
- Edema of the lower extremities
How is the diagnosis made?
Most often, when undergoing a professional examination, medical examination, or fluorography, doctors may notice significant deviations in the shape of the heart or changes in the electrocardiogram. An experienced cardiologist will always be able to hear a rough heart murmur characteristic of aortic stenosis and will prescribe a number of studies:
- Electrocardiograms
- X-ray of the chest organs
- 24-hour Holter ECG monitoring
- ECHO-cardiography (ultrasound of the heart)
- In difficult cases, multislice computed tomography with the introduction of a contrast agent is required.
This scope of research allows you to confirm or exclude the diagnosis, determine the stage of the disease and prognosis.
In the later stages of the development of the defect, patients are admitted to the cardiology department with symptoms of acute myocardial infarction; an incorrect diagnosis is often made and the effect is treated rather than the cause.
What are the stages of the disease?
Aortic valve stenosis occurs:
- Easy
- Moderate
- Expressed
- Heavy
- Critical
Who is treating?
Mild to moderate aortic stenosis is monitored by a cardiologist with periodic consultations with a cardiac surgeon.
Severe, severe and critical aortic stenosis is treated by a cardiac surgeon. The treatment method is surgical replacement of the aortic valve.
What are the approaches to surgical treatment?
Depending on the stage of the disease, the age of the patient and many other factors, there are open surgical techniques, minimally invasive techniques, and endovascular aortic valve replacement (TAVI).
Each method has its own advantages and disadvantages.
Aortic valve replacement using an open technique under artificial circulation.
During open surgery, a longitudinal incision of the sternum and complete visualization of the heart are performed under artificial circulation. Then a heart-lung machine is connected, the heart stops, the altered heart valve is excised, and a prosthetic heart valve is securely sewn in its place.
Advantages of the method:
- Wide use
- This approach is considered excellent
- It is easy to influence complications that arise during surgery
Disadvantages of the method:
- Significant surgical trauma (scar length 20-25 cm).
- The need to sleep strictly on your back for 3 to 6 months.
Duration of the operation: from 3 to 6 hours.
In the intensive care unit: usually about 36 hours.
Total duration of hospitalization: 12-15 days.
Risk of intervention: about 1.5%
Aortic valve replacement from a mini-access under artificial circulation
This surgical correction option is characterized by a smaller incision, which is less traumatic for the patient. The course of the operation is similar to open surgery.
Advantages of the method:
- Less traumatic method
- Cut about 10 cm long
- Early rehabilitation
- There is no need to sleep on your back for long periods of time
Disadvantages of the method:
- Great technical complexity
- Limited ability to influence complications during surgery, or requires switching to a larger incision
Duration of the operation: from 2 to 8 hours.
In the intensive care unit: usually about 24 hours.
Total duration of hospitalization: 10-15 days.
Risk of intervention: more than 2%
Endovascular aortic valve replacement
Since 2007, intravascular aortic valve replacement has been used worldwide. With this approach, a large artery of the thigh is punctured, a folded prosthetic aortic valve is passed through the vessel into the heart, in the right place it is inflated on a special balloon and, breaking the narrowed aortic valve, it becomes in its place.
Advantages of the method:
- Minimal trauma, incision is 1 cm, often the intervention is performed under local anesthesia
Disadvantages of the method:
- It is extremely difficult to influence the complications that arise.
- High price
- Possibility of implantation of exclusively biological prosthetic heart valve
- There are many restrictions and contraindications for carrying out.
Duration of the operation: from 1 to 6 hours.
In the intensive care unit: usually about 24 hours.
Total duration of hospitalization: 5-10 days.
Risk of intervention: moderate
What's the prognosis?
If you seek medical help in a timely manner, most patients, after successful surgical treatment, fully return to normal life within 3-6 months. People who work physically can return to work after 4-6 months; if the work does not involve physical effort, 6-8 weeks is often enough for rehabilitation. It should be understood that in each specific case the pace of rehabilitation is individual and depends on the patient’s age, the degree of “neglect” of the case, the presence of concomitant diseases, and complications during treatment.
I need to get examined! What are the stages?
1. Consultation with a cardiac surgeon.
After an in-person examination and a standard physical examination, it is possible with a high degree of probability to confirm or refute aortic stenosis.
Research will be conducted:
- Electrocardiography
- ECHO-cardiography (ultrasound of the heart)
If the diagnosis is confirmed, further examination is indicated before hospitalization in a specialized hospital.
- Determination of blood group, Rh factor
- Diagnosis of HIV, hepatitis B, C, syphilis
- General urine analysis
- General blood analysis
- Standard biochemical blood test
- X-ray of the chest organs, or fluorography
- Consultation with a urologist for men, a gynecologist for women
- Fibrogastroscopy
The main purpose of the examination before planned hospitalization is to exclude possible contraindications.
2. Hospitalization to a specialized hospital for further examination
In a hospital setting the following will be performed:
- Coronary angiography (men over 40 years old, women in menopause)
- Control ECHO-cardiography
- Examination with the participation of the head of the department or a professor as part of a council in order to determine the indications for surgical treatment and the choice of treatment tactics.
3. Discharge from the hospital with the exact date of hospitalization for surgical treatment if consent and indications are available.
4. Registration of a quota of high-tech medical care for surgical intervention.
5. Hospitalization for surgical treatment
6. Postoperative observation.
If you find yourself with similar symptoms, or your cardiologist suggests this diagnosis, do not hesitate, seek qualified medical help, we will conduct an examination on an outpatient basis, accompany hospitalization in a specialized hospital for high-tech additional examination and surgical treatment, and ensure proper monitoring after the operation.
Without surgical treatment of severe forms, the long-term prognosis for life is unfavorable. Patients die from acute myocardial infarction, sudden arrhythmic death, rupture of aortic aneurysm, aortic dissection, and progressive congestive heart failure.
Remember: aortic valve stenosis cannot be treated with pills and IVs!!!
Make an appointment now
Treatment without surgery
Treatment of narrowing of the orifice and aortic valve insufficiency is required only if the onset of decompensation is suspected, arrhythmia is detected, or severe damage is detected. Correct and timely use of medications allows you to avoid surgery.
Groups of pharmacological drugs are used that enhance myocardial contractility, making it possible to prevent arrhythmias and the manifestation of failure. These include:
- calcium antagonists;
- diuretics;
- β-blockers;
- drugs that dilate coronary vessels.
Treatment of aortic valve diseases
Currently, unfortunately, there are no medications available to treat valve disease, so your doctor may prescribe medications that can reduce the effects of the disease.
Drug treatment
For aortic valve insufficiency, medications are prescribed to lower blood pressure and prevent fluid buildup. If you have aortic stenosis, your doctor may recommend the use of medications to control heart rhythm disorders. Beta blockers, as well as calcium deposit blockers, can cope with any angina pectoris (chest pain). Your doctor may also prescribe statins to lower your blood cholesterol levels.
Surgery
There are several surgical treatments for aortic valve disease, but the most common and effective treatment is valve replacement. During the procedure, the surgeon removes the damaged valve and replaces it with a new one made from tissue from a human donor or a large animal, such as a cow or pig.
The surgeon may also suggest transplantation of a mechanical valve made of metal. Such valves are highly wear-resistant, but increase the risk of developing blood clots in the heart. If a mechanical valve is installed, the patient will need to take anticoagulant medications (such as warfarin) for ongoing management of the person's condition.
Instead of replacing the valve, a treatment procedure called valvuloplasty may be performed. This treatment method does not require the long recovery required for valve replacement. During the procedure, the doctor inserts a thin tube with a balloon at the end into the patient's body, then guides it to the aortic valve and inflates the balloon. An inflated balloon opens and stretches the valve, improving blood flow. This operation is rarely performed on adult patients due to the risk of re-narrowing of the valve.