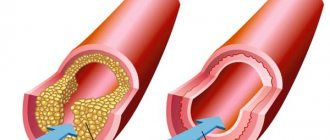
The disease belongs to the group of chronic obliterating diseases of the arteries of the legs. This is a whole group of diseases, the common symptom of which is a decrease in blood flow to the limb due to stenosis (narrowing) or occlusion (complete blockage) of the artery. The stage of arterial insufficiency and the degree of tissue ischemia (bleeding) depend on the degree of stenosis. The more pronounced the stenosis, not to mention the occlusion, the less blood volume enters the limb.
Changes in the vascular wall of the arteries, which lead to stenosis or occlusion of the vessel, occur in many diseases, but most often the cause is only four diseases:
Obliterating atherosclerosis - develops mainly in men over 40 years of age against the background of increased cholesterol levels (low and very low density lipoproteins). Mainly large and medium caliber arteries are affected, such as: aortic bifurcation; common iliac; femoral and popliteal arteries.
Obliterating endarteritis (thromboangiitis obliterans, Buerger's disease) is an inflammatory disease of the vascular wall of autoimmune origin, usually occurring at a young age. The disease is characterized by the presence of autoantibodies and circulating immune complexes in the blood. In the initial stages of the disease, mainly small and medium caliber arteries are affected, in particular, the arteries of the leg and foot. At later stages, larger arteries are involved in the pathological process - popliteal, femoral and iliac.
Nonspecific aortoarteritis (Takayasu's disease) is an inflammatory disease of autoimmune origin affecting the aorta and its large branches.
Diabetic angiopathy. Occurs in patients suffering from diabetes. Diabetic angiopathy is characterized by damage to both small and large vessels. Changes in the vascular wall occur especially often in arteries of medium and small caliber (popliteal, tibial, arteries of the foot).
In addition to the above diseases, post-embolic occlusion, traumatic thrombosis, as well as congenital diseases (hypoplasia, aplasia and fibromuscular dysplasia) are much less common.
It is generally accepted among specialists to divide the vascular bed of the lower extremities, including according to the level of disease damage, into 3 levels (segments):
- aorto-iliac;
- femoral-popliteal;
- popliteal tibial (peripheral)
The incidence of obliterating atherosclerosis and other occlusive diseases of the arteries of the lower extremities is not reliably known, since about half of patients with diseases of the peripheral arteries of the lower extremities do not have any symptoms or signs of the disease. However, the incidence of peripheral artery disease of the lower extremities is known to increase with age and at least 25% of the US population suffers from these diseases.
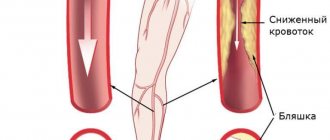
How OASNK is developing
The inner wall of healthy vessels is smooth and even. This allows blood to flow within the lumen of the vessel without any difficulty. With atherosclerosis, the inner wall of the artery becomes uneven and thickened due to cholesterol deposits (cholesterol plaques). This pathological process is called atherosclerosis. With further development of the disease, narrowing or complete blockage of the arteries occurs, which leads to a significant decrease in blood flow to the legs. The consequence of this is the appearance of pain in the calf muscles when walking (intermittent claudication), numbness, and chilliness in the feet. As the disease progresses, pain in the legs becomes constant. Ultimately, trophic ulcers and necrosis appear in the foot area. If no therapeutic measures are taken, the next stage of the disease may be gangrene (death) of the limb.
Narrowing of blood vessels in the legs: symptoms and consequences
Vasoconstriction of the lower extremities has several stages of development. And not all of them have clear symptoms. The first stage can be called asymptomatic. The patient does not notice any changes in his condition or does not attach much importance to them.
Vasoconstriction makes itself felt gradually. As the disease progresses, the nutrition of tissue cells deteriorates due to insufficient blood supply. Some patients begin to notice that their legs feel cold and sensitivity is impaired. And only then do they wonder what is happening to them? This means that the symptom complex of the pathology is increasing. In its manifestations, this is called obliterating atherosclerosis and is characterized by the following unpleasant sensations in the lower extremities:
- a feeling of tingling and burning in the feet;
- pain in the ankle and toes;
- intermittent claudication syndrome;
- increased sweating;
- swelling;
- cyanosis;
- hypertension, etc.
Due to the fact that the disease is detected in late stages, the symptoms are already its consequences. Therefore, along with the above symptoms, patients are faced with:
- necrosis and rotting of soft tissues;
- muscular atrophy of the lower extremities;
- dysfunction of the pelvic organs;
- trophic ulcers.
The above consequences mean that the disease is already severe, and may lead the patient to subsequent disability.
Expert opinion
Not only the localization of pathology in the veins of the lower extremities, but also in the arteries can lead to dangerous consequences for the health and even the life of the patient. In particular, stenosis of cerebral vessels deserves special attention. A gradual decrease in the lumen of the veins and arteries that supply the brain leads to a decrease in the volume of nutrients necessary for the normal functioning of the brain. This leads to the development of neurological problems, the most dangerous of which is stroke.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
Statistics on the development of deep vein thrombosis by disease
Risk factors for OASNK
Atherosclerosis of the vessels of the lower extremities is characterized by the same risk factors as other arterial diseases, for example: coronary heart disease and cerebrovascular insufficiency.
- High blood pressure (hypertension),
- High blood cholesterol levels,
- Smoking,
- Sedentary lifestyle,
- Obesity,
- Burdened heredity.
A few words about smoking. Complete abstinence from any form of tobacco is necessary. Smoking even 1 cigarette per day of the lightest type is an unfavorable risk factor that causes the progression of obliterating atherosclerosis of the lower extremities and the development of its severe complications. The nicotine contained in tobacco causes the arteries to spasm, thereby preventing blood from moving through the vessels and increasing the risk of blood clots in them.
Why does lower limb stenosis occur?
Among the factors that provoke the development of this disease are:
- history of atherosclerosis;
- active and passive smoking;
- alcohol abuse;
- lower limb injuries;
- diabetes;
- high blood pressure;
- obesity;
- consequences and complications of past infectious diseases.
Hereditary factors play a major role in the etiology of lower extremity stenosis. If close relatives are diagnosed with this pathology of the cardiovascular system, the patient is at risk.
Symptoms of OASNK
- Pain in the leg at rest, depriving the patient of sleep;
- Pain or a feeling of fatigue in the leg muscles when walking (usually in the calf muscles) - this symptom is one of the early signs of atherosclerosis of the leg vessels;
- Unusual feeling of chilliness and numbness in the foot, aggravated by physical activity (walking, climbing stairs;
- The presence of a non-healing wound or trophic ulcer, usually located in the foot or lower third of the leg;
- Darkening of the skin, often in the form of dark brown or black necrosis of the toes (gangrene);
- Difference in skin temperature between extremities (the affected leg is cooler than the healthy leg).
Stages of development of atherosclerosis of the lower extremities
The manifestation of one or another symptom depends on the stage of atherosclerosis of the arteries of the lower extremities. In this connection, the following stages are distinguished (in our country, classification according to A.V. Pokrovsky, 1976):
- Stage I – pain in the lower extremities manifests itself during heavy physical activity, walking over a distance of more than 1 km.
- Stage II A – pain in the limb occurs when walking at a normal pace for more than 200 m.
- Stage II B - pain in the limb occurs when walking at a normal pace of less than 100-200 m,
- Stage III – pain in the limb occurs at rest or when walking less than 25 m.
- Stage IV – the pain is constant, there are ulcerative-necrotic changes in the tissue.
Most often, the level of damage is accompanied by complaints of characteristic localization.
With atherosclerosis of the aorta and iliac arteries, the so-called Leriche syndrome, in which pain is localized in the gluteal muscles, thigh muscles, there is no pulsation in the femoral arteries, or it is sharply weakened. Men also experience impotence.
With obliterating atherosclerosis of the femoral and popliteal arteries, pain is localized in the muscles of the legs and feet.
Obliterating diseases of the aorta and arteries of the lower extremities
X
Chronic obliterating diseases of the aorta and arteries of the lower extremities (caused in most cases by atherosclerosis) account for more than 20% of all types of cardiovascular pathology, which corresponds to 2–3% of the total population [1]. Thus, in the Edinburgh study (1990) [2], patients with intermittent claudication accounted for 4.5% in the age group from 55 to 74 years, and asymptomatic lesions were noted in 8% of cases. It is significant that the attending physicians only 30–50% of patients knew about the presence of intermittent claudication in the latter [3].
The main feature of this pathology is its steadily progressive course.
, characterized by an increase in the severity of intermittent claudication and its transition to a constant pain syndrome or gangrene, which occurs in 15–20% of patients [4]. Perioperative mortality for amputations below the knee is 5–10%, above the knee – 15–20%. Mortality during the first two years after amputation ranges from 25–30%, and after 5 years – 50–75%. Moreover, after amputation of the lower leg, only 69.4% of patients walk on a prosthesis after 2 years, and only 30.3% of the hips.
Mortality after reconstructive surgery, which previously amounted to 2–13% [5], currently does not exceed 1.2% in leading Russian clinics [6]. When estimating the required number of operations for patients with obliterating diseases of the aorta and arteries of the lower extremities, we can cite the United States as an example, where in 1995 there were 400,000 hospitalizations for diseases of the peripheral arteries. 50,000 balloon angioplasties, 110,000 bypass operations, and 69,000 amputations were performed. Moreover, the costs of primary amputation in developed countries, such as the UK, were twice as high as the costs of successful revascularization [7].
According to L.A. Bokeria et al. [8], as of 1998, the need for reconstructive operations on the arterial system in Russia is 930 per 1 million population, no more than 22% of the required number is performed annually.
Pathomorphology and pathogenesis
The term “atherosclerosis” comes from the Greek words “athtre” - wheat gruel and “sclerosis” - hard. Despite the fact that the pathomorphology of atherosclerosis has been studied for more than 140 years, starting with the first works of R. Virchow (1856), the nature and features of the processes occurring in the vascular wall during this disease remain not completely clear. Even cellular and extracellular changes observed during microscopic examination in the vessel wall in the area of atherosclerotic plaque formation are interpreted differently. During the formation of atherosclerosis, the main changes occur in the endothelium and smooth muscle cells of the subendothelial layer of the intima.
There are 4 types of atherosclerotic changes in blood vessels:
1. Fatty spots or stripes, which are pale yellow areas containing lipids that do not rise above the surface of the intima. These are the earliest manifestations of atherosclerosis.
2. Fibrous plaques
- oval or round formations containing lipids, rising above the surface of the intima, often merging into continuous tuberous fields.
3. Fibrous plaques with various kinds of complications:
ulceration, hemorrhage, imposition of thrombotic masses.
4. Calcinosis
– deposition of calcium salts in fibrous plaques.
The most significant atherosclerotic changes are most often localized in places of greatest hemodynamic or mechanical impact on the vessel wall: bifurcation zones, places where the main arteries depart from the aorta and in tortuous sections of the artery.
According to JSA Fuchs [9], the leading risk factors for the development of atherosclerosis include arterial hypertension, hypercholesterolemia and smoking. To a lesser extent, obesity, diabetes mellitus, hypertriglyceridemia, sedentary lifestyle, stress and heredity influence.
Modern diagnostic methods
Modern methods for diagnosing peripheral arterial circulatory disorders are distinguished by their wide range - some are used to clarify the clinical diagnosis, the nature and extent of vascular damage, others are used to assess the effectiveness of treatment or dynamic monitoring of the patient. In order to study hemodynamics in the lower extremities and topical diagnosis of lesions of the arterial bed, the following instrumental research methods are used:
Doppler ultrasound sphygmomanometry, treadmill test, ultrasound angioscanning, including duplex, and radiopaque aortoarteriography. In addition, it is necessary to determine indicators of lipid metabolism, coagulation system and rheological properties of blood.
As the first stage, all patients with suspected occlusive-stenotic lesions of the aorta or arteries of the lower extremities undergo Doppler ultrasound with measurement of the ankle-brachial index
.
This index is the ratio of the maximum pressure on one of the tibial arteries to the pressure on the brachial artery. A decrease in this indicator to less than 0.9 requires closer attention to the patient. of Doppler ultrasound and standard treadmill test seems to be one of the most promising at present.
[10].
Non-invasive research methods also include ultrasound angioscanning
, thanks to which the degree of stenotic lesion can be determined with a high degree of certainty.
Recently, duplex ultrasound angioscanning
has taken one of the leading places in the diagnostic program algorithm due to its non-invasiveness and safety, as well as high sensitivity and specificity.
According to duplex scanning data, not only the structure of the atherosclerotic plaque is determined, but also the hemodynamic degree of stenosis is assessed, which is of fundamental importance. X-ray contrast angiographic examination
currently remains the main method for diagnosing obliterating diseases of the vascular bed. Using this method, it is possible to accurately determine the location, extent, degree and nature of stenosis, the multiplicity of occlusive lesions of the main arteries of the lower extremities, assess the condition of the collateral bed, predict the nature and volume of reconstructive surgery, and also monitor the effectiveness of treatment and surgery. In the arsenal of angiologists and vascular surgeons there are also such diagnostic methods as laser Doppler flowmetry, transcutaneous O2 monitoring, photoplethysmography, radioisotope study, computed tomography and nuclear magnetic resonance.
Terminology and clinical classification
“Leriche syndrome” is often used to refer to diseases of the abdominal aorta that lead to its narrowing or occlusion.
, which summarizes the picture of damage to the bifurcation of the abdominal aorta and iliac arteries.
The main features of the clinical course of this lesion are high intermittent claudication (pain in the limb when walking), bilateral absence of pulses in the arteries and impotence.
In approximately 30% of patients with chronic arterial insufficiency of the lower extremities, the atherosclerotic occlusive process is localized in the abdominal aorta, in 70% of patients - in the arteries of the femoral-popliteal segment.
Tactical issues in choosing one or another treatment method for atherosclerotic lesions of the aorta and arteries of the limb are based on the severity of chronic ischemic syndrome, which is classified into 4 stages of the disease. The predominant assessment system is the classification of R. Fontaine and A.V. Pokrovsky.
At stage 1 of the disease
pain in the lower extremities appears only with heavy physical activity; it is not related to the distance the patient walks.
For stage 2
Characteristic is the appearance of limiting pain when walking (limiting intermittent claudication). From a tactical point of view, this stage is divided into 2A (a distance walked without pain of more than 200 m) and 2B (the appearance of pain when walking at a distance of less than 200 m).
Pain in the limb at rest characterizes the 3rd stage
, the appearance of ulcerative-necrotic changes -
stage 4 of the disease.
Surgical tactics and determination of the degree of surgical risk
The fundamental generally accepted position in choosing a treatment method in accordance with this classification is the need to restore the main blood flow using reconstructive operations, starting from stage 2B.
When deciding on surgical treatment, it is necessary to take into account the multifocal nature of the atherosclerotic lesion and the presence of concomitant pathology that aggravates the condition of the patients. According to our data, about 70% of patients suffer from coronary heart disease, every 4th is diagnosed with post-infarction cardiosclerosis and chronic cerebral circulatory failure, half of the patients have hypertension in combination with chronic lung diseases. 35% have gastrointestinal tract diseases and every 7th person has diabetes mellitus.
Based on all of the above, treatment of patients with atherosclerosis should be comprehensive
, aimed both at restoring blood circulation in the aorta and main arteries of the limb, and at correcting concomitant pathology. The main goal - restoration of blood circulation - should be achieved with minimal trauma to the patient.
Principles of conservative treatment
One of the main directions of conservative treatment is to improve the rheological properties of blood.
And this is not accidental, since patients have pronounced deviations in rheological characteristics: an increase in the level of fibrinogen in plasma, an increase in platelet aggregation time, blood and plasma viscosity, a decrease in the fibrinolytic activity of the blood and a change in thromboelastogram parameters towards hypercoagulation.
Among the drugs used for conservative therapy, several groups are distinguished.
1. Antispasmodics:
peripheral myolytics (papaverine, drotaverine, bencyclane), drugs blocking a-adrenergic receptors or preganglionic impulse transmission (caffeine, prazosin), central cholinomyolytics (tolperisone, baclofen), substances with versatile effects (abana).
2. Disaggregants:
pentoxifylline, acetylsalicylic acid, xanthinol nicotinate, ticlopidine, rheopolyglucin.
3. Antiatherosclerotic agents:
drugs that block the absorption of cholesterol from the intestine (cholestyramine), inhibiting the biosynthesis and transfer of cholesterol and triglycerides (fibric acid derivatives - clofibrate, ciprofibrate) and statins (lovastatin, simvastatin), other drugs (nicotinic acid).
4. Metabolic drugs:
solcoseryl, actovegin, etc.
5. Angioprotectors:
pyricarbate, etc.
I would especially like to emphasize that dosed walking
– health path, which promotes the development of collateral circulation.
Purely conservative treatment is indicated for patients with chronic arterial insufficiency of stage 1 and 2A; in patients with stage 2B and critical ischemia with the development of ulcerative-necrotic lesions, the question arises about the need to restore the main circulation. Thanks to the capabilities of modern technologies, in recent years a lot of work has appeared on the use of balloon angioplasty.
in patients with different localization of occlusive-stenotic lesions of the arteries of the pelvis and lower extremities.
However, it is not possible to use balloon repair in all cases due to aortic occlusion or common arterial occlusions. Attempts at recanalization in these cases are dangerous by the development of thrombosis of the main arteries (often with thrombosis of the peripheral bloodstream), which inevitably leads to amputation of the limb in 60% of cases, and often to death.
Types of reconstructive surgical interventions
In case of high occlusion of the aorta, bilateral damage to the arteries of the extremities, depending on the severity of the patient’s condition, operations are performed from aortofemoral bifurcation or linear bypass to axillary or subclavian-femoral bifurcation bypass. If critical ischemia is present only on one side, then if the iliac and femoral arteries are affected on the contralateral limb, a unilateral cross-iliac-femoral, axillary or subclavian-femoral bypass
.
At the present stage, reconstructive operations occupy a leading place in the treatment of these patients. The number of such operations is constantly increasing, their scope is expanding significantly, which makes it possible to save a limb even in severe forms of chronic arterial insufficiency. Contractubex is effective for resolving keloid scars that occur after surgery.
, which has fibrinolytic, antithrombotic and keratolytic effects.
Meanwhile, performing a full-fledged reconstruction often conflicts with the patient’s ability to undergo surgery. Operations in these cases should be minimal in terms of trauma and duration, since the vast majority of this group of patients have severe concomitant diseases that sharply limit the functional reserve capabilities of the body [11]. Using the combined operations method
, including balloon angioplasty in combination with open surgery under epidural or local anesthesia, can significantly reduce the volume of intervention and eliminate complex surgical reconstruction in several segments.
Clinical case
Patient Z., 68 years old, was admitted with complaints
for aching pain in the right leg and foot at rest, intermittent claudication after 30 m.
Doppler ultrasound:
a significant decrease in the main blood flow in the right common femoral artery, collateral blood flow in the popliteal and tibial arteries.
Ankle-brachial index
left 0.59, right 0.35.
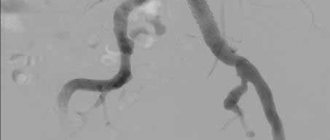
Aortoarteriography:
critical stenosis of the common iliac artery (CIA) on the right; stenosis of the deep femoral artery (DFA) on the right; occlusion of both superficial femoral arteries (SFA), segmental occlusion of the right popliteal artery for 5 cm (Fig. 1).
Rice.
1. Angiograms of patient Z.: a — stenosis of the abdominal cavity on the right; b — stenosis of the GBA on the right, occlusion of both SBAs; c — after balloon angioplasty (absence of an area of stenosis of the right PA). Atherosclerotic lesion of arteries (case history).
Concomitant diseases: coronary heart disease, atherosclerotic cardiosclerosis, angina pectoris, chronic bronchitis, pneumosclerosis, pulmonary emphysema.
coronary heart disease, atherosclerotic cardiosclerosis, angina pectoris, chronic bronchitis, pneumosclerosis, pulmonary emphysema.
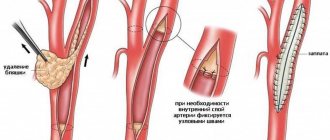
The first stage was balloon angioplasty of the right abdominal organ, and the second stage, under epidural anesthesia, was lateral plasty of the gastrointestinal tract on the right (Fig. 2).
Rice.
Fig. 2. Scheme of stages of surgical treatment of patient Z.: a - before surgery; b — balloon angioplasty of the right PCA; c — condition after plasty of the GBA and balloon angioplasty of the abdominal organ on the right. As a result,
positive dynamics were noted: the ankle-brachial index on the right increased to 0.71 (initially 0.35). The patient was discharged in satisfactory condition for outpatient treatment.
You can find a list of references on the website https://www.rmj.ru
References:
1. Pokrovsky A.V., Koshkin V.M., Kirichenko A.A. et al. Vasaprostan (prostaglandin E1) in the treatment of severe stages of arterial insufficiency of the lower extremities. A manual for doctors. M., 1999; 16.
2. Fowkes FG, Housley E, Cawood EH et al. Edinburgh artery study: prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidimiol 1991; 20: 384–92.
3. Burakovsky A.I., Bockeria L.A. Cardiovascular surgery. M., 1989; 750.
4. Dormandy J., Mahir M., Ascady G. et al. Fate of the patient with chronic leg ischemia. J Cardiovasc Surg 1989; 30:50–7.
5. Stoffers HEJH. Kaiser V. and Knottnerus JA Prevalence in the general practice. In: Fowkes FGR, ed. Epidemiology of peripheral vascular disease. London: Springer Verlag. 1992; 109–13.
6. Spiridonov A.A., Fitileva E.B., Arakelyan V.S. Ways to reduce mortality in surgical treatment of chronic ischemia of the lower extremities. J. Annals of Surgery. 1996; 1:62–6.
7. Bead J.D. Amputation or reconstruction for critical ischemia. J. Angitology and Vascular Surgery 1998; 1 (4): 72–82.
8. Bockeria L.A., Gudkova R.G. Surgery of the heart and blood vessels in the Russian Federation. M., 1998; 43.
9. Fuchs JSA. Atherogenesis and the medical management of Atherosclerosis. In: Rutherford RB, ed. Vascular surgery. Philadelphia: W. B. Saunders Company. 1996; 1:222–35.
10. Zatevakhin I.I., Tsitsiashvili M.Sh., Yudin R.Yu. Treadmill in the diagnosis and treatment of chronic arterial insufficiency. M., 1999; 87.
11. Siskin G., Darling RC III, Stainken B. et al. Combined use of Iliac artery angioplasty and infrainguinal revascularization for treatment of multilevel atherosclerotic disease. Annals of Vascular Surgery. St. Louis. 1999; 13 (1): 45.
Diagnostic methods for OASNK
If atherosclerosis of the arteries of the lower extremities is suspected, further examination is necessary to confirm (or exclude) the diagnosis of OASNK, establish the stage of the disease and determine treatment tactics. For this purpose, the following series of diagnostic measures are carried out:
- Examination by a vascular surgeon to determine the pulsation of the main arteries of the extremities, neck and abdominal cavity, as well as listening to noises in the projection of large vessels;
- Ultrasound duplex scanning
- X-ray contrast angiography;
- Computed tomography in angio mode;
- Magnetic resonance imaging in angio mode.
Through the above studies, local damage or multifocal (multi-level, multi-story) atherosclerosis of the main arteries, atherosclerosis of the aorta and arteries of the lower extremities is revealed. Areas of complete closure of the lumen (occlusion) of the artery and thrombosis may be detected.
Narrowing of blood vessels in the legs: how is stenosis diagnosed?
What to do if symptoms of the disease are detected? In order to avoid an unfavorable prognosis due to narrowing of the blood vessels in the legs, you should plan a visit to the doctor as soon as possible. During it, the specialist will:
- a thorough survey to judge the development of a particular disease, its possible causes, and also to preliminarily assess the severity of the patient’s condition;
- examination of the legs to assess the condition of the skin;
- palpation of the extremities for pain, pastiness and compaction along the vessels.
After a physical examination, the doctor prescribes the necessary laboratory diagnostics of the patient’s condition. This may include:
- general clinical tests;
- extended hemostasiogram;
- lipid profile;
- immunogram;
- D-dimer test;
- analysis of blood composition for gases and acidity.
Diagnosis of narrowing of blood vessels in the legs
In turn, instrumental diagnosis of the disease is carried out in various ways: Dopplerography, duplex and triplex scanning, sonography, X-ray contrast angiography, electrocardiography, EchoCG, infrared thermography, rheoencephalography, etc. The most informative methods are considered to be contrast angiography and tomography with contrast. The selection of the optimal diagnostic method or their combination is made by the doctor individually in each specific case.
Treatment of atherosclerosis of the vessels of the lower extremities
A vascular surgeon treats atherosclerosis of the aorta and arteries of the lower extremities.
Treatment of obliterating atherosclerosis of the vessels of the lower extremities depends on the stage of the disease and its prevalence. In the initial stages, it may be sufficient to eliminate risk factors for the disease:
- Weight correction for overweight or obese patients;
- Monitoring and correction of blood sugar levels in patients with diabetes mellitus;
- Control of blood pressure and maintain it at the recommended level (no more than 140/90 mmHg);
- Quitting bad habits (primarily smoking);
- Regular physical activity (training walking, exercise on an exercise bike, visiting the pool, etc.). Therapeutic walking for atherosclerosis of the lower extremities is of great importance for the development of collaterals. A gradual daily increase in physical activity is necessary;
- Following a diet low in cholesterol and animal fats;
- Reducing blood cholesterol levels to doctor-recommended levels.
Drug treatment of obliterating atherosclerosis of the arteries of the lower extremities
Most often, to prevent the sticking of platelets (blood cells involved in the formation of a blood clot), the doctor prescribes drugs containing aspirin or drugs containing clopidogrel.
Medicines that improve collateral (roundabout) blood circulation - pentoxifylline containing drugs.
Statins are also used - these are drugs aimed at lowering blood cholesterol levels, thereby slowing down the growth of atherosclerotic plaque.
Medicines that improve peripheral circulation by dilating blood vessels - drugs based on prostanoids.
Surgical treatment of obliterating atherosclerosis
Surgical treatment for atherosclerosis of the arteries of the lower extremities is used in cases where conservative treatment is ineffective, there are signs of disease progression, as well as in advanced stages of the disease:
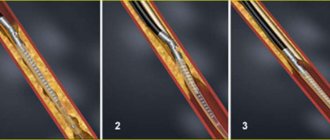
- Balloon angioplasty;
- Prosthetics;
- Stenting;
- Bypass;
- Endarterectomy.
- Lumbar sympathectomy is an operation to destroy sympathetic nerve fibers and remove the lumbar sympathetic ganglia, which are capable of contracting the muscular wall of the arteries. The operation is performed to increase blood flow to the tissues and reduce pain. This operation is also performed to reduce excessive sweating of the feet.
Treatment
Based on the results of the examination, a treatment regimen adapted to the individual patient is prescribed.
In the early stages of stenosis, drug therapy is prescribed using drugs aimed at restoring and maintaining the elasticity of blood vessels; the patient also takes vasodilators. At the medical center. Rabin uses unique thrombus-dissolving drugs. With a properly designed treatment regimen, it is possible to achieve high treatment efficiency and avoid surgical intervention.
In the case of a critical stage of the disease, an operation is required, the purpose of which is to widen the affected vessel and install a special stent to prevent its re-narrowing.
Depending on the indications, angioplasty or stenting surgery is performed.
Balloon angylplasty
. The angioplasty procedure is an advanced endovascular technology that is performed without tissue incision and does not require intubation anesthesia. Using special miniature instruments with visual X-ray control, a special catheter with an inflatable balloon at the end is inserted into the artery. When a blockage in the vessel is reached, the balloon expands, expanding the lumen of the artery to its normal size. A self-absorbable stent is inserted into the lumen, which then serves as the frame of the vessel, with a special drug coating. When performing cryoplasty, liquid nitrous oxide is introduced into the balloon instead of air, and as a result of exposure to extremely low temperatures, the atherosclerotic plaque is destroyed.
The latest endoscopic equipment used in the medical center named after. Rabin, allows you to achieve the highest precision of all manipulations performed and restore the patency of blood vessels in the lower extremities.
Bypass surgery
. Open surgery is performed when balloon angioplasty is not possible for medical reasons. During surgery, a special shunt is created from a section of the saphenous vein of the leg to bypass the affected vessel. The operation is performed under general anesthesia.
In particularly difficult cases, endovascular (intravascular) balloon angioplasty with stenting and bypass surgery are performed simultaneously.
Video: What is vasoconstriction and how to deal with it
is not responsible for the accuracy of the information presented in this video clip. Source - Medservice Izhevsk
Sources:
- Karpenko A.A., Starodubtsev V.B., Ignatenko P.V., Zoloev D.G. Hybrid surgical interventions in patients with multilevel atherosclerotic lesions of the arteries of the lower extremities // Angiology and Vascular Surgery. 2014. T. 20, No. 2.
- Bondarenko M.A., Lebedeva E.A., Artyushin B.S. Biomechanical method for studying the influence of atherosclerotic lesions on hemodynamics in the arteries of the lower extremities // Proceedings of St. Petersburg Electrotechnical University "LETI". 2015. No. 9.
- Begun P.I., Krivokhizhina O.V., Sukhov V.K. Computer modeling and biomechanical analysis of critical condition and correction of structures of the vascular system (Part I) // Management in medicine and biology. 2005. No. 6.
- OBLITERATING ATHEROSCLEROSIS OF THE LOWER LIMB IN ELDERLY PEOPLE. Polyakov P.I., Gorelik S.G., Zheleznova E.A. // Bulletin of new medical technologies. – 2013. – No. 1. – P. 98-101.
- DIAGNOSTICS OF THROMBOTIC PROCESSES IN THE VEINS OF THE LOWER LIMB IN OUTPATIENT PRACTICE. Vlasova I.V., Tleubaeva N.V., Vlasov S.V., Pronskikh I.V. // Polytrauma. – 2011. –№3. – P. 65-75.
- https://iliveok.com/health/disease-peripheral-vessels-legs_112749i16070.html
- https://medlineplus.gov/ency/article/000170.htm
For an accurate diagnosis, contact a specialist.