Determine your total cardiovascular risk
April 30, 2015
There are no clear causes for the development of cardiovascular diseases, but predisposing factors have been identified. They are usually called risk factors. Risk factors are interrelated and enhance each other’s effects, so doctors determine the total cardiovascular risk. This can be done using the SCORE scale, which is used in all European countries, including Russia.
There are no clear causes for the development of cardiovascular diseases, but predisposing factors have been identified. They are usually called risk factors. Risk factors are interrelated and reinforce each other, so doctors determine the total cardiovascular risk. This can be done using the SCORE scale, which is used in all European countries, including Russia. The SCORE (Systematic COronary Risk Evaluation) scale allows you to estimate a person’s risk of dying from cardiovascular diseases over the next 10 years. It is recommended to use the SCORE scale in people aged 40 years and older. To determine cardiovascular risk using the SCORE scale, you need to know a person's age and gender, total cholesterol levels and systolic (upper) blood pressure levels, and whether the person smokes or not.
How to use the score scale
1. First, decide which side of the Scale applies to you. The left one measures risk in women, the right one measures risk in men. 2. Select the horizontal columns that correspond to your age (40 years, 50 years, 55 years, 60 years and 65 years). 3. Each age corresponds to two columns, the left column refers to non-smokers, the right column refers to smokers. Choose the one that applies to you. 4. Each column has four horizontal lines corresponding to the level of systolic (upper) blood pressure (120 mmHg, 140 mmHg, 160 mmHg, 180 mmHg, ) and five vertical columns corresponding to the level of total cholesterol (4 mmol/L, 5 mmol/L, 6 mmol/L, 7 mmol/L, 8 mmol/L). 5. In the column of your choice, find the cell that corresponds to your systolic (upper) blood pressure and total cholesterol levels. 6. The number in this cell indicates your total cardiovascular risk. A risk of less than 1% is considered LOW, ranging from ≥ 1 to 5% - MODERATE ≥ 5 to 10% - HIGH ≥10% - VERY HIGH For people under 40 years of age, it is recommended to use the Relative Risk Scale. The scale is used regardless of a person’s gender and age and takes into account three factors: systolic (upper) blood pressure, total cholesterol level and smoking. The technology for its use is similar to that for the main SCORE scale. Using this scale you can determine how much your cardiovascular risk is above the minimum. Non-smokers with a blood pressure level of 120/80 mmHg have minimal cardiovascular risk. and total cholesterol – 4 mmol/l. The SCORE scale is not used if you have: - cardiovascular disease, which is based on vascular atherosclerosis - diabetes mellitus type I and II - very high levels of blood pressure and/or total cholesterol - chronic kidney disease If these conditions are present, the risk is considered HIGH and VERY HIGH. In people with moderate and especially high and very high cardiovascular risk, active measures are needed to reduce the levels of all risk factors.
Tags:
- GCC
- year of fight against CVD
To leave a comment you must be an authorized user
What is the Score scale and what is it used for?
The Score scale began to measure absolute cardiovascular risk in 2003. The decision to use this technique was made after 12 basic studies were carried out in Western European countries aimed at creating a unified system for predicting potential consequences for the heart and blood vessels.
The scientific project involved 205,178 patients of different ages, gender, and also having different indicators of blood tests and the functional state of internal organs.
Using research data, doctors were able to create a universal scale that is used to make a high-quality and objective forecast for the development of the risk of possible diseases of the cardiovascular system, as well as the occurrence of death in adult men and women.
Automatic calculation
It's easier to work with a calculator. Data on gender, age, blood pressure and cholesterol levels, and smoking status are entered into the appropriate cells. After entering the data, the “Calculate” button is activated. The resulting number will be the risk percentage.
Evaluation of results
| Received number, % | Risk level |
| 1 | Weak |
| 1―5 | Average |
| 5—10 | High |
| From 10 | Critical |
If the obtained indicator lies above the limit of 10%, but there are no symptoms of a disturbance in the functioning of the cardiovascular system, then the person is nevertheless at risk of a stroke or heart attack with a fatal outcome.
What measures should be taken in case of absolute risk?
Men and women diagnosed with an absolute risk of developing cardiovascular disease should take the following responses:
- undergo a comprehensive examination by a cardiologist and phlebologist;
- give up alcohol, tobacco products and taking drugs;
- start leading an active lifestyle;
- perform moderate cardiac exercises;
- follow dietary standards aimed at reducing blood cholesterol levels;
- get rid of excess body weight;
- undergo a course of medication and physiotherapeutic treatment of concomitant diseases, the progression of which increases the risk of cardiovascular pathologies.
A cardiologist, whose examination is mandatory, may prescribe additional preventive measures that strengthen the heart muscle, as well as improve blood flow in the great vessels.
If necessary, the heart can instantly change its operating mode
Normally, the heart is a strong muscular pump capable of pumping blood throughout the body to provide oxygen and nutrients to all organs and tissues of the body, and remove waste products. But in order to move blood through spasmodic vessels, the heart requires more effort than normal. This leads to its size becoming larger, especially the left ventricle. Because of this, weakness of the heart muscle develops. When the heart stops adequately supplying tissues and organs with oxygen and nutrients, doctors diagnose heart failure. It can be caused by irregular heartbeats (cardiac arrhythmias). It is dangerous and can lead to heart failure when the heart beats more than 140 beats per minute, since the processes of filling and ejecting blood by the heart are disrupted.
You can live with heart failure for many years without a diagnosis. This is not an independent disease, but the outcome of various heart diseases. It signals itself in the form of increased fatigue, swelling of the legs, shortness of breath, asthma attacks, and causeless weight loss. These symptoms, if noticed individually, appear in a wide variety of diseases. Therefore, the correct diagnosis is rarely made and usually in later stages. Significant weight loss, which is typical of severe heart failure, is often mistaken for a sign of cancer. And harmless swelling of the legs caused by stagnation of lymph is diagnosed as “heart failure.” With some primary symptoms (for example, pulmonary edema), there is an immediate risk of death. Within 3-5 years, 50% of patients die from heart failure, and after 9 years, only 2 people out of 1000 patients remain alive - of course, provided that appropriate treatment is not carried out. There is a radical way to help - a new heart transplant. But restrictions - an age limit, an expensive operation, few donor hearts - make it unrealistic for most.
In recent years, medical science, pharmacology and medical experience have helped to achieve amazing success in treating even severe forms of heart failure. Patients can not only save their lives, but also restore their quality. Moreover, treatment can take place on an outpatient basis, without a hospital stay.
Treatment of people with cardiovascular diseases requires effort, time and great pedantry. The speed and accuracy of diagnosis of the underlying disease that caused heart failure plays a huge role. In 50% of cases, this is coronary heart disease, which can be identified and treated with coronary angiography and angioplasty. The earliest, they are called preclinical (that is, before the onset of complaints), forms of heart failure can be treated only by using instrumental research methods: echocardiography, Holter monitoring, stress tests.
The problem of the century is atherosclerosis
Atherosclerosis is deposits of cholesterol in the wall of a vessel in the form of plaques, which can partially or completely close the lumen of the vessel. This process happens with age for everyone, but in different ways. Its development is influenced by heredity (heart attacks or strokes in close relatives at an early age), the level of cholesterol and its fractions in the blood, lifestyle (smoking, lack of physical activity, poor nutrition) and the presence of concomitant diseases (arterial hypertension, diabetes mellitus, kidney disease ). All these diseases and conditions contribute to faster and more intense growth of atherosclerotic plaques.
The most “popular” atherosclerosis is obliterating - when atherosclerotic plaques are deposited on the walls of blood vessels and therefore block them. It usually affects large arteries of the elastic and muscular-elastic type - for example, the terminal aorta, iliac or femoral arteries. Often these are the lower extremities. People die from this type of atherosclerosis all over the world because it ends in a stroke or heart attack. Less is known about vasodilatory atherosclerosis - when the nutrition of the vascular wall is disrupted, causing it to expand, forming a pouch. At the final stage of type 2 atherosclerosis, it is called an aortic aneurysm. An aneurysm occurs in the thoracic or abdominal aorta. Statistics show that abdominal aneurysm occurs more often. But all aneurysms are equally dangerous. At one unexpected moment, the bag bursts and the person dies. Vasodilating atherosclerosis is talked about less, but people die from it just as often as from obliterating atherosclerosis. The percentage of people dying from vasodilating atherosclerosis is quite high - up to 75%.
The aorta delivers blood from the heart to all organs and tissues, passing through the chest and abdominal cavity. The normal diameter of the abdominal aorta is about 2 cm. When the diameter increases by 1.5-2 times, an aneurysm is formed. To prevent aneurysm rupture, endoprosthetics is performed. Aortic aneurysm is one of the most unpredictable diseases. Very often it appears and gradually increases in size unnoticed by the patient - therefore, sometimes the first clinical symptom of an aneurysm is its rupture. The incidence of aneurysms increases with age.
A ruptured aneurysm is usually fatal, regardless of treatment. The survival rate of patients after a standard aortic replacement procedure, even in a planned manner, is low; every fifth patient dies.
“Smart” gadgets are an assistant in heart control
I really like modern devices that allow you to assess how much work a person did during the day, how many steps and kilometers he walked, and what his heart rate was. This is useful, since the load level is often calculated based on the pulse. I also like devices that allow you to evaluate the duration and quality of sleep (by sleep phases). This is a very useful feature for people living in the modern world, when both pleasure and work are prolonged due to sleep. Meanwhile, only in sleep the body is restored, healed and absorbs daytime information. “Smart” gadgets are my favorite gift to everyone who is dear to me.
How often do you need to be tested when an absolute cardiovascular risk is determined by the Score?
Adult men and women over 40 years of age who have completed the Score examination and are found to be at absolute cardiovascular risk undergo a preventive examination as directed by a cardiologist.
The frequency of visits to a specialist in this profile is influenced by the patient’s general health, his age, and the type of concomitant diseases. In the absence of pronounced symptoms associated with decreased function of the heart and blood vessels, the optimal frequency of preventive examinations by a cardiologist is once every 4-6 months.
Odds
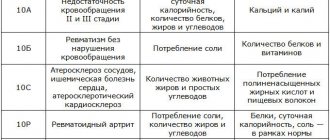
The tables present the coefficients that are used to assess the potential risk of death from cardiovascular diseases, taking into account the Score methodology.
Table 1:
| Main risk factors for death | Coronary heart diseases | Non-coronary diseases of the cardiovascular system |
| Use of tobacco products | 0,71 | 0,63 |
| Cholesterol (unit mmol/l) | 0,24 | 0,02 |
| Systolic blood pressure indicator | 0,018 | 0,022 |
Table 2:
| Coronary heart diseases | Non-coronary diseases of the cardiovascular system | ||||
| A | R | A | R | ||
| Low level | Male | -22,1 | 4,71 | -26,7 | 5,64 |
| Female | -29,8 | 6,36 | -31,0 | 6,62 | |
| High level | Male | -29,8 | 4,62 | -25,7 | 5,47 |
| Female | -29,8 | 6,23 | -30,0 | 6,42 | |
Based on these coefficients, a formula is drawn up with further complex and step-by-step calculations, allowing one to obtain the final result in the form of the potential probability that over the next 10 years a particular person will die from heart or blood vessel diseases.
In this case, the onset of death can occur suddenly, or occur due to prolonged coronary heart disease.
Evidence-based medicine and myths of cardiology
Until the 90s, Russian cardiologists treated based on the opinions or views of different medical schools, which often did not agree with each other on scientific research. When the massive advent of computers helped to introduce the principles of evidence-based medicine everywhere, uniform requirements for conducting scientific research were formulated. When evaluating drugs, double-blind randomized studies have begun to be used, which are highly accurate and impartial. We created a unified knowledge base and assessment of all research conducted in the world that corresponds to a high scientific and technical level. As a result, the efficiency and safety of diagnosing and treating patients has dramatically increased.
A myth that all doctors face, but which is especially dangerous in cardiology, can be expressed in one common phrase: “Don’t take medicine, you’ll destroy your liver.” Medicines are metabolized in the liver and eliminated through the liver or kidneys, but they do not destroy them. Canceling the selected therapy can lead to a sharp increase in blood pressure, cholesterol levels and other indicators. This aggravates diseases from heart attack and stroke to diabetic coma. Surprisingly, patients are not afraid to take dietary supplements (dietary supplements) or alcohol in any quantity.
The second common myth in the practice of a cardiologist is the erroneous opinion about the dangers of cholesterol-lowering drugs - statins. A large number of studies based on the principles of evidence-based medicine confirm the high effectiveness of this group of drugs in preventing the development of atherosclerosis and its consequences (heart attack, stroke, damage to the arteries of the legs, intestines); these drugs are included in all generally accepted recommendations. Statins require constant, simple laboratory monitoring in order to avoid fairly rare side effects. Individual intolerance occurs when using any medicine or even food product. When using statins too, but rarely.