Electrocardiography (ECG) is the main and most common instrumental method for diagnosing coronary heart disease (CHD). Depression or elevation of the ST segment on the ECG, inversion and other alterations of the T wave, especially associated with physical or psycho-emotional stress, reliably indicate pathology of the coronary vessels.
Savely Barger
practicing cardiologist, candidate of medical sciences, Moscow. In the 1980s, he was one of the first scientists in the USSR to develop a technique for diagnostic transesophageal cardiac pacing. Author of manuals on cardiology and electrocardiography. He is the author of several popular books devoted to various problems of modern medicine.
The variety of clinical manifestations of coronary artery disease, the prevalence and localization of coronary artery lesions, combined with the low specificity of changes in the ST segment and T wave, cause difficulties in diagnosing coronary pathology. The connection of an anginal attack in coronary artery disease with physical stress allows the use of stress tests: characteristic ECG changes during physical activity are almost unambiguously associated with the pathology of the coronary arteries.
When taking a test with physical activity, squats, walking or running in place, bending or push-ups are performed, performed with different intensities and at different tempos, which does not allow unification and standardization of diagnostic physical activities.
Bicycle ergometry (VEM) and treadmill test (treadmill test) used today make it possible to dose physical activity in kilogram meters (kg*m), joules (J) or in MET units (metabolic equivalent, 1 MET corresponds to the level of basal metabolic rate: 3. 5 ml of oxygen per 1 kg of body weight per minute). The level of oxygen consumption reflects the functional state of the body, primarily the state of the cardiovascular system. High oxygen consumption during physical activity is typical for trained people; a decrease in this indicator indicates depleted reserves of the heart muscle.
Clinicians (cardiologists and therapists) must know the diagnostic capabilities of the method, indications and contraindications for it, some limitations of its use imposed by the sensitivity and specificity of the technique. Load tests are prescribed:
- for diagnostic purposes in patients whose diagnosis of coronary artery disease has not been established
- to clarify the origin of pain in the heart area
- for diagnosing cardiac arrhythmias
- to identify individuals with a hypertensive response to exercise
- to determine the exercise tolerance of patients with an established diagnosis of coronary artery disease, including those who have suffered a myocardial infarction or cardiac surgery in order to evaluate the effectiveness of treatment and or rehabilitation measures
- to clarify the prognosis in coronary patients and in patients with other heart diseases, including after surgical treatment for examination of work capacity
- for assessing the physical condition of healthy people, including in sports, military, and space medicine
The Master's step test, performed at a pace set by the beat of a metronome, was the first attempt to standardize the ECG test with physical activity; it made it possible, with a certain degree of reliability, to compare the results of different laboratories and evaluate the dynamics of disease progression or success in the patient's rehabilitation.
Diagnostic stress test
In patients with cardialgia, to verify the diagnosis of coronary artery disease, an exercise test is performed on a bicycle ergometer or on a treadmill. The choice of research technique depends on the technical capabilities of the laboratory, on preferences and, to a lesser extent, on the physical condition of the patient.
Some patients find it easier to perform the exercise on a bicycle ergometer, while others find it more convenient to use a treadmill. People with excess body weight (more than 100–110 kg) are offered a treadmill, as are patients with concomitant pathology of the lower extremities (joint diseases, vascular pathology), who find it difficult to perform exercises on a bicycle ergometer.
It is preferable for women to be prescribed a treadmill; all other things being equal, they perform a higher power load on the treadmill, and accordingly, a higher heart rate is achieved. When performing a test on a bicycle ergometer, women and older patients stop the load before reaching a submaximal heart rate for noncardiac reasons (fatigue, pain in the legs, etc.), accordingly, the test is incomplete and diagnostically insignificant.
A diagnostic exercise test is prescribed to patients with an initially unchanged ECG, on which the ST segment is located on the isoline. This is primarily due to the fact that a positive stress test in the classic case presupposes ST segment depression of more than 1 mm (0.1 mV) or its elevation of more than 2 mm (0.2 mV).
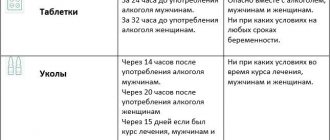
Beta blockers and coronary lytics, as well as vasodilating drugs, are discontinued 1–2 days before the study. If for clinical reasons it is impossible to stop taking these drugs (retrosternal pain due to drug withdrawal), interpretation of the study results will be extremely difficult, and the test itself will be devoid of diagnostic meaning.
How to prepare for the procedure
You need to prepare for an ECG with stress in advance, otherwise the results will not be reliable. Preparation is especially important for patients with vascular and heart problems. A cardiologist may recommend that you stop taking certain medications that slow your heart rate several days before the test, which reduces the stress response and reduces the heart muscle's need for oxygen. This group of drugs includes beta blockers.
Patients are also advised to:
- do not eat 3-4 hours before diagnosis;
- stop smoking and drinking alcohol 24 hours before the procedure;
- exclude vigorous physical activity 12 hours before;
- On the eve of the test, exclude chocolate, coffee, energy drinks, and sweet carbonated drinks from your diet.
Three days before the ECG stress test, men should not take any drugs that enhance erection (Viagra, Cialis, Levitra, etc.).
A special case
Among the contraindications to stress tests, there is no depression of the ST segment and a negative T wave (meaning leads where the T wave is obligately positive). At the same time, the appointment of a stress test in such patients must be approached with caution, and specialists in functional diagnostics must take into account some features when conducting the study and assessing its results.
The diagnostic algorithm in patients with initial ST segment depression and a negative T wave should include pharmacological tests with obzidan and potassium chloride. A positive test result (ST segment tightening and T wave inversion from negative to positive) is regarded as a sign that rejects the diagnosis of coronary artery disease. It is also useful to conduct an active orthostatic test - recording an ECG in the supine and standing positions; in some cases, ST depression disappears, the segment is pulled closer to the isoline. Such ECG dynamics cast doubt on the diagnosis of coronary pathology. In case of hyperventilation (at least 20 deep and frequent respiratory movements), a positive test is to normalize the ECG parameters. A positive test with hyperventilation is caused by sympatho-adrenal mechanisms; the diagnosis of IHD can be excluded in this case.
Exercise testing in patients with initially altered ECG (ST depression and T wave inversion) is carried out with extreme caution. If, under minimal loads (25 and 50 W) with an increase in heart rate, the ST segment returns to the isoline, then such ECG dynamics should be regarded as a sign of a negative test that rejects damage to the coronary arteries in the patient.
ECG interpretation algorithm
There is a scheme for deciphering an ECG with a sequential study of the main aspects of heart function:
- sinus rhythm;
- Heart rate;
- rhythm regularity;
- conductivity;
- EOS;
- analysis of teeth and intervals.
Sinus rhythm is a uniform heartbeat rhythm caused by the appearance of an impulse in the AV node with gradual contraction of the myocardium. The presence of sinus rhythm is determined by deciphering the ECG using P wave indicators.
Also in the heart there are additional sources of excitation that regulate the heartbeat when the AV node is disturbed. Non-sinus rhythms appear on the ECG as follows:
- Atrial rhythm - P waves are below the baseline;
- AV rhythm – P is absent on the electrocardiogram or comes after the QRS complex;
- Ventricular rhythm - in the ECG there is no pattern between the P wave and the QRS complex, while the heart rate does not reach 40 beats per minute.
When the occurrence of an electrical impulse is regulated by non-sinus rhythms, the following pathologies are diagnosed:
- Extrasystole is premature contraction of the ventricles or atria. If an extraordinary P wave appears on the ECG, as well as when the polarity is deformed or changed, atrial extrasystole is diagnosed. With nodal extrasystole, P is directed downward, absent, or located between QRS and T.
- Paroxysmal tachycardia (140-250 beats per minute) on the ECG can be presented in the form of an overlay of the P wave on the T wave, standing behind the QRS complex in standard leads II and III, as well as in the form of an extended QRS.
- Flutter (200-400 beats per minute) of the ventricles is characterized by high waves with difficult to distinguish elements, and with atrial flutter, only the QRS complex is distinguished, and sawtooth waves are present in place of the P wave.
- Flicker (350-700 beats per minute) on the ECG is expressed in the form of inhomogeneous waves.
Heart rate
The interpretation of the ECG of the heart must contain heart rate indicators and is recorded on tape. To determine the indicator, you can use special formulas depending on the recording speed:
- at a speed of 50 millimeters per second: 600/ (number of large squares in the RR interval);
- at a speed of 25 mm per second: 300/ (number of large squares between RR),
Also, the numerical indicator of the heartbeat can be determined by the small cells of the RR interval, if the ECG tape was recorded at a speed of 50 mm/s:
- 3000/number of small cells.
The normal heart rate for an adult is between 60 and 80 beats per minute.
Regularity of rhythm
Normally, the RR intervals are the same, but an increase or decrease of no more than 10% from the average value is allowed. Changes in the regularity of the rhythm and increased/decreased heart rate can occur as a result of disturbances in automatism, excitability, conductivity, and contractility of the myocardium.
When the automatic function is impaired, the following interval indicators are observed in the heart muscle:
- tachycardia - heart rate is in the range of 85-140 beats per minute, a short period of relaxation (TP interval) and a short RR interval;
- bradycardia - heart rate decreases to 40-60 beats per minute, and the distances between RR and TP increase;
- arrhythmia – different distances are tracked between the main heartbeat intervals.
Conductivity
To quickly transmit an impulse from the source of excitation to all parts of the heart, there is a special conduction system (SA and AV nodes, as well as the His bundle), the violation of which is called blockade.
- Heart attack on ECG - signs and interpretation
There are three main types of blockades - sinus, intraatrial and atrioventricular.
With sinus block, the ECG shows a violation of impulse transmission to the atria in the form of periodic loss of PQRST cycles, while the distance between RRs increases significantly.
Intraatrial block is expressed as a long P wave (more than 0.11 s).
Atrioventricular block is divided into several degrees:
- I degree – prolongation of the PQ interval by more than 0.20 s;
- II degree – periodic loss of QRST with an uneven change in time between complexes;
- III degree - the ventricles and atria contract independently of each other, as a result of which there is no connection between P and QRST in the cardiogram.
Electric axis
EOS displays the sequence of impulse transmission through the myocardium and normally can be horizontal, vertical and intermediate. In ECG interpretation, the electrical axis of the heart is determined by the location of the QRS complex in two leads - aVL and aVF.
In some cases, axis deviation occurs, which in itself is not a disease and occurs due to an enlargement of the left ventricle, but, at the same time, may indicate the development of pathologies of the heart muscle. As a rule, the EOS deviates to the left due to:
- ischemic syndrome;
- pathology of the valve apparatus of the left ventricle;
- arterial hypertension.
A tilt of the axis to the right is observed with enlargement of the right ventricle with the development of the following diseases:
- pulmonary stenosis;
- bronchitis;
- asthma;
- pathology of the tricuspid valve;
- congenital defect.
Positive test
Criteria for a positive test: the appearance of a typical anginal attack, the development of rhythm or conduction disturbances during the test (atrial fibrillation, atrioventricular block, frequent extrasystoles, etc., ST segment depression of more than 2 mm during the test, inversion of the T wave into the negative phase). If the test is positive, the heart rate at which the indicated signs appeared, the double product, the maximum load power or the MET value should be noted when the criteria for stopping the test appear.
Based on the results of the test with physical activity, a conclusion is issued: a) positive test, b) negative test, c) doubtful or d) unreliable (incomplete, uninformative) test.
Research methodology
Special electrodes or branches are attached to the patient's chest and limbs, transmitting electrical vibrations that occur on the surface of the skin.
A total of six branches are used, three of them are installed on the anterior chest in the projection of the heart and three on the limbs. In some cases, additional branches are used. The electrocardiograph receives information from installed electrodes, which show different amplitudes of oscillations. The data from each electrode is recorded by an electrocardiograph and displayed on paper tape with a millimeter mark in a graphical image. The paper medium moves at a certain speed. Modern devices allow you to display the received data on a monitor and record the results on digital media. In the finished electrocardiogram
information from all electrode branches is summed up.
Cardiogram
The following electrical parameters of the heart muscle are reflected:
- the location of the electrical axis of our heart;
- heartbeat rhythm;
- physiological parameters of the heart;
- arrhythmias and other pathological disorders of the heart rhythm;
- various changes associated with disruption of the electrophysiological functions of cardiac tissue, insufficient conductivity, slow metabolism, etc.;
- myocardial damage in acute or chronic form.
ECG
allows for early diagnosis of atherosclerotic lesions of the heart vessels before the development of myocardial infarction, as well as other processes accompanied by changes in the coronary vessels (vasculitis).
Negative test
A conclusion about a negative test is formed in the absence of clinical and ECG signs of coronary circulatory disorders. In this case, attention should be paid to the patient achieving a submaximal heart rate (75–85% of the maximum heart rate for his age) and performing a load of at least 150 watts (12 MET). For example, achieving a heart rate of 150 min-1 at a load of 125 W does not allow us to conclude that the test is negative, since the submaximal heart rate was achieved at a load of less than 150 W. If, with a load of 150 W, a heart rate of 130 min-1 is achieved, which is less than 75% of the maximum heart rate, the test should still be regarded as negative. Our own experience and data from the medical literature suggest that patients with coronary artery disease are not able to perform a load of 150 watts with a heart rate less than submaximal.
Features of the event
An ECG for a child is performed in the same way as for an adult. The difference lies in the use of relatively small skin electrodes, the structure and shape of which takes into account the anatomical features of the baby. In our clinic, instead of traditional “suction cups” for children, we use “sticker” electrodes, which eliminates unpleasant sensations during ECG recording. The procedure involves the use of a certified device that has many functions and capabilities.
One of the important conditions is the correct mood of the baby, his calmness. This requires the right atmosphere, confidential communication with the doctor, and a friendly attitude towards the child. If these conditions are not present, the study is difficult to consider informative - a crying little patient may simply not allow him to be examined, and tachycardia, which occurs during severe anxiety, will distort the picture.
The Family Doctor clinic employs specialists who can find an approach to patients of any age. Creating a favorable environment ensures the reliability of the survey results.
Uninformative test
The test can be stopped due to severe shortness of breath, pain in the joints or legs until the patient reaches a submaximal heart rate when performing a low or medium power load (less than 150 watts), while clinical and electrocardiographic criteria for stopping the test are not noted. As a rule, patients in these cases do not achieve submaximal heart rate. The results of such tests are regarded as uninformative.
Exercise tolerance allows you to evaluate the effectiveness of treatment and rehabilitation measures.
During physical activity, blood pressure increases. At initial systolic blood pressure 160 mm Hg. Art. or more, the test should be abandoned if during the test the blood pressure rises to 230 mm Hg. Art., the test should be stopped. The test results are assessed according to generally accepted criteria; the type of circulatory response to stress is additionally assessed as hypertensive (inadequate increase in blood pressure at each level of load).
Who is the procedure indicated for?
In addition to healthy people who want to assess the speed of adaptation of the body and the functionality of the cardiac system after physical effort, an ECG with stress is necessarily performed on patients for diagnosis:
- coronary heart disease (CHD) at an early stage;
- myocardial infarction;
- heart block at an early stage;
- arrhythmias;
- chronic heart failure (CHF) at an early stage;
- hypertension;
- disorders in the circulatory system.
For people suffering from cardiovascular diseases, stress tests are performed to:
- control over the condition of the heart muscle during ischemic heart disease and heart failure;
- determining tolerance to various physical activities;
- assessment of the condition after myocardial infarction during treatment;
- monitoring the work of the heart with a pacemaker;
- assessing the rate of health recovery after surgery;
- definitions of disability.
Where to do the research
If you notice that you have heart
, you need to seek help from a therapist or cardiologist.
The specialist will definitely write out a referral for an ECG.
In Moscow, you can get examined at the Doctor Nearby network of clinics.
The medical center employs competent diagnosticians, and high-precision equipment is installed. research is carried out at the highest professional level. If necessary, an orthostatic test is performed with an ECG.
Comfortable conditions have been created for patients; diagnostic results with interpretation are given to them
.
Treadmill
It is similar to the bicycle ergometry method, but a treadmill with a changing angle of inclination of the plane is used as a simulator - simulating uphill running. The diagnostic method is acceptable for children - the simulator has no restrictions on the height and weight of the subject, unlike an exercise bike.
Treadmill is a diagnostic method similar to a bicycle ergometer, invented by American scientists
Indications of changes are taken during exercise and after exercise, after which an analysis of changes in the norm is carried out.