Transesophageal pacing
– a non-invasive procedure aimed at obtaining a recording of biological potentials from the outer surface of the heart, using special esophageal electrodes and recording equipment.
Carrying out special types of stimulation to study the electrophysiological properties of the conduction system, atrial and ventricular myocardium. Identification of arrhythmia substrates, their localization and electrophysiological characteristics. Monitoring drug and/or non-pharmacological therapy.
Non-invasive electrophysiological examination of the heart (TEPS)
The experience of using TEES in cardiology spans more than 30 years.
In our country, the first report on the use of TEES in patients with coronary heart disease appeared in the scientific medical literature more than 10 years ago.
Over this period of time, the attitude towards any research method has already become stable, and the capabilities of the method itself have been well studied.
It should be said that the attitude of cardiologists to the TEES method during this time changed depending on the development of cardiology itself and the technical capabilities of the stimulators used.
The increased interest in this method is currently due, on the one hand, to the rapid development of cardiology itself as a science, in particular its arrhythmology, as well as the emergence of modern stimulators with good technical characteristics that allow the study to be carried out with minimal discomfort for the patient.
The use of TEE helps solve three main problems: diagnosis, treatment
(therapeutic, selection of antiarrhythmic drugs) and
prognosis
in many clinical situations.
Scope of application of TEES in cardiology
In patients with coronary heart disease:
1) diagnosis of coronary insufficiency; 2) determination of the degree (functional class) of coronary insufficiency, 3) diagnosis of silent myocardial ischemia; 4) identification of a group of patients with coronary heart disease (CHD) who have a high risk of sudden cardiac death; 5) selection of the optimal effective dose of the antianginal drug and the most rational use of it during the day; 6) identifying a group of patients for whom it is most appropriate to undergo coronary angiography and subsequent surgical treatment of coronary artery disease; 7) verification of large focal scar changes in the myocardium in patients with WPW syndrome; simultaneous registration of an echocardiogram according to the stress echocardiogram program during dosed frequency loading during TEES makes it possible to diagnose latent forms of coronary and myocardial insufficiency.
2) determination of the degree (functional class) of coronary insufficiency, 3) diagnosis of silent myocardial ischemia; 4) identification of a group of patients with coronary heart disease (CHD) who have a high risk of sudden cardiac death; 5) selection of the optimal effective dose of the antianginal drug and the most rational use of it during the day; 6) identifying a group of patients for whom it is most appropriate to undergo coronary angiography and subsequent surgical treatment of coronary artery disease; 7) verification of large focal scar changes in the myocardium in patients with WPW syndrome; simultaneous registration of an echocardiogram according to the stress echocardiogram program during dosed frequency loading during TEES makes it possible to diagnose latent forms of coronary and myocardial insufficiency.
In patients with cardiac arrhythmias:
1) assessment of sinus node function: - diagnosis of sick sinus syndrome (SSNS); — diagnosis of functional dysfunction of the sinus node (most often associated with increased activity of the Vagus node) — assessment of the functional state of the myocardium before installing a permanent endocardial pacemaker;
2) assessment of atrioventricular (AB) node function;
3) differential diagnosis of paroxysmal supraventricular tachyarrhythmias using the method of tachyarrhythmia provocation and subsequent registration of the esophageal electrogram (PE);
4) diagnosis and study of the electrophysiological properties of additional, abnormal conduction pathways (Kent's bundle and James' bundle); — diagnosis of the syndrome of premature excitation of the ventricles in the case of the functioning of the Kent or James points; — diagnosis of paroxysmal tachyarrhythmias in Wolff-Parkinson-White (WPU) or Clerk-Levy-Cristescu (CLC), Lown-Ganong-Levin (LGL) syndrome; — identification of a group of patients with VPU syndrome and atrial fibrillation at risk of developing ventricular fibrillation;
5) selection of the optimal effective dose of an antiarrhythmic drug: - to relieve paroxysm of tachyarrhythmia; - to prevent the occurrence of paroxysmal tachyarrhythmia; — identification of the arrhythmogenic effect of the drug;
6) relief of paroxysmal supraventricular tachyarrhythmias (except for atrial fibrillation);
7) maintaining the required heart rate (HR) during surgery in case of initial bradycardia;
8] study of the electrophysiological properties of the supraventricular zone: atria, AV node, additional conduction pathways (refractory periods of structures);
9) registration of tachycardia-dependent extrasystole and intraventricular blockades;
CPES has a wide range of applications from outpatient clinics to inpatient units. The method for clinicians in their clinical activities is the most accessible and less burdensome for the patient.
The diagnostic capabilities of TEE are limited to stimulation of the left atrium. In some cases, stimulation of the left ventricle can be achieved, but for this it is necessary to apply a voltage with an amplitude of 30-60 V (mA), which is practically impossible without the use of anesthesia.
to the top of the page
Information for patients.
Transesophageal electrophysiological examination (TEPE) is carried out only as prescribed by a doctor.
Patients with attacks of tachycardia (fast pulse) are indicated for this study if they experience episodes of rapid heartbeat that cannot be recorded on an ECG.
During the study, an attack of tachycardia is provoked, which is recorded and analyzed. As a result, the presence of tachycardia is not only confirmed and documented, but its type is also determined. This is an important point in the further treatment of the patient, as well as in determining the indications for radical treatment of tachycardia - radiofrequency ablation of the tachycardia focus.
It is important to know that most tachycardias can now be completely cured. But to do this, you first need to make sure that they really exist and make a diagnosis, which is why a transesophageal electrophysiological study is performed.
In patients with bradycardia (slow pulse), TEE can provide additional information useful for clinical assessment of the disease and choice of treatment. In this case, during the study, the function of the sinus node, which is the source of normal heart rhythm, is assessed. An assessment of the conduction of impulses through the heart through the atrioventricular node is also performed. Typically, patients are referred for TPE if a rare pulse is detected based on ECG data and 24-hour heart rate monitoring.
TPEFI is carried out as follows:
The study is performed in a specially equipped room using a modern automated complex “Astrocard-Polysystem EP/L” (Moscow, Russia) and a bipolar electrode PEDSP-2 from SKB MET (Kamenetsk-Podolsky, Ukraine). This equipment is rightfully considered the most convenient and informative for conducting research.
Transesophageal electrophysiological study is performed strictly on an empty stomach. Before the study, it is necessary to discontinue antiarrhythmic drugs, because they change the electrophysiological parameters of the heart. The doctor must tell you how long you should not take the medication, since it depends on the type of drug.
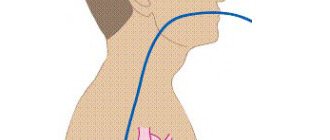
To conduct the study, a special electrode is inserted into the esophagus. Usually the electrode is inserted through one of the nasal passages, less often through the mouth. Next, the electrode is connected to the complex for performing TPE. When the electrode is installed correctly, its tip is located in the esophagus at the level of the heart.
The study is based on the anatomical features of the location of the esophagus, which is a hollow collapsed tube closely adjacent to the posterior surface of the left atrium and partly the left ventricle. The mucous membrane of the esophagus has relatively low pain sensitivity. A special transesophageal ECG is recorded from the tip of the electrode, which clearly shows processes that are difficult to assess on a regular ECG. After correct installation of the electrode, the transesophageal electrical stimulation protocol is carried out. It involves step-by-step execution of different pacing modes to determine cardiac electrophysiological parameters. To do this, short series of electrical pulses are applied across the electrode. Typically, the applied pulses have an amplitude of 12-25 mA with a duration of 10 ms. During stimulation, patients may feel a tingling and slight burning sensation behind the sternum, but there is no severe pain if the procedure is performed correctly. During stimulation episodes, the patient is asked not to swallow.
During the study, some patients are tested with intravenous atropine. The question of whether this test is necessary is decided during the research process, based on the results obtained.
After receiving all the data, a research protocol is drawn up. Typically, the entire study with registration of results takes 30-60 minutes.
There are contraindications for conducting transesophageal electrophysiological studies:
- inability to insert the electrode into the esophagus (high gag reflex);
- diseases of the esophagus (tumors, strictures, diverticula, esophagitis, varicose veins and others);
- atrial fibrillation at the time of examination, persistent AV block of the third degree;
- circulatory failure II b – III stage;
- valve prostheses;
- acute infectious diseases.
Over the years of successful work, doctors in our department for the surgical treatment of arrhythmias and pacemakers have acquired unique experience in conducting research not only in adults, but also in children.
Doctors perform TPE and also program pacemakers (PACs):
- Ivashkova Irina Yurievna - cardiologist,
- Shupan Emilia Dmitrievna – Ph.D. cardiologist,
- Pushkareva Irina Alekseevna – cardiologist.
Registration for studies is carried out by nurse coordinator Zinaida Vasilievna Zueva by phone (812) 24-600-14 (from 09:00 to 16:00 on weekdays).
Application of TEES for cardiac arrhythmias
The use of TEES for cardiac arrhythmias was justified as a result of the rapid development of arrhythmology and based on its problems.
The use of TEES in this category of patients solved many problems of supraventricular arrhythmias and fully replaced such a research method as intracardiac electrophysiological study (EPS).
Therefore, indications for EPI are currently narrowed and can be determined by the following conditions:
1 Clarification of the diagnosis and selection of therapy for patients with ventricular tachycardia. 2. Syncope, unknown etiology. 3. Before surgical treatment of arrhythmias. 4. Before implantation of a pacemaker or cardioverter-defibrillator in patients with tachyarrhythmias. 5. To carry out cryodestruction of abnormal conduction pathways in case of their right-sided passage. 6. Patients with WPW syndrome and paroxysmal atrial fibrillation, which occurs with loss of consciousness and the threat of transformation into ventricular fibrillation.
Rice. Transesophageal electrogram, bipolar recording
When starting a study on the rhythm disturbance program using the TEES method, the doctor conducting it must be sure that everything is prepared in case of resuscitation measures: the defibrillator is prepared and turned on, there is the necessary set of resuscitation drugs and supplies.
In addition, the doctor conducting the study must be well trained in such disciplines as clinical cardiology with arrhythmology, clinical electrocardiography, know the electrophysiology of the myocardium, issues of emergency cardiology and resuscitation.
It should be especially emphasized that the study of PPES according to the program for cardiac arrhythmias must be carried out in the presence of at least two medical workers - a doctor and a nurse who have undergone special training.
TEES can be performed for diagnostic and therapeutic purposes. In the event of a diagnostic study, all antiarrhythmic drugs should be discontinued.
Rice. A. Paired stimulation of the atria causes paroxysm of AV reciprocal orthodromic tachycardia. The RP'-interval on TEE is less than 1/2 the RR-interval and = 120 ms. B. Relief of paroxysm by paired stimulation.
to the top of the page
Assessment of coronary circulation using the TEES method
This stimulation program is the basis from which the TEES method began as one of the stress tests (rhythm load) in cardiology.
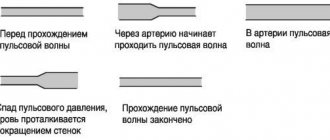
The use of a stimulation program allows you to gradually and dosedly increase the frequency of ventricular contractions with constant assessment of changes in the final part of the ventricular complex on the monitor and when recording an ECG.
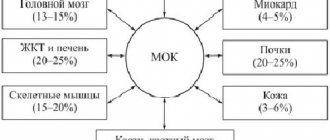
The use of TEES to assess coronary circulation allows the cardiologist to solve a number of important problems:
1. establish the very fact that the patient has coronary heart disease (CHD) and its forms, in particular, determine painless myocardial ischemia; 2. determine the degree of coronary insufficiency; 3. determine the optimal effective dose of the antianginal drug and the frequency of its administration; 4. to identify a group of patients with coronary heart disease with severe coronary insufficiency, for whom coronary angiography and possible surgical treatment of coronary artery disease are strongly recommended; 5. determine the prognosis and management tactics for patients with coronary artery disease after myocardial infarction; 6. identify a group of patients with coronary artery disease who have a high risk of sudden cardiac death for the purpose of preventive treatment; 7. carry out differential diagnosis of post-infarction cardiosclerosis in patients with Wolff-Parkinson-White syndrome; 8. identification of hidden forms of rhythm and conduction disorders; 9. when dynamically performing TES in the same patient with coronary artery disease, indirectly judge the rate of progression of coronary atherosclerosis and the effectiveness of the treatment.
In addition to general contraindications, performing TES according to the coronary circulation assessment program is not advisable in the following cases:
1. in the presence of persistent complete blockade of the left bundle branch; 2. when recording an obvious (manifesting) syndrome of premature excitation of the ventricles caused by the functioning of the Kent bundle on a resting ECG; 3. a patient with coronary artery disease with 3-4 functional class; 4. in a patient with new-onset angina during the first 4 weeks and in a patient with unstable angina; 5. during the first 3 weeks of uncomplicated myocardial infarction; 6. with pronounced hypertrophy of the left ventricular myocardium with secondary changes in the final part of the ventricular complex on the ECG. TEES is carried out as prescribed by the attending physician 2 hours after a meal against the background of withdrawal of coronary drugs in the case of a diagnostic study. In this case, the patient’s consent to perform TES, recording a resting ECG and echocardiogram (EchoCG) is required.
The stimulation program for the purpose of assessing coronary circulation is quite simple. After obtaining a stable pacemaker rhythm that exceeds the natural heart rate by 20 pulses/min, continuous stepwise stimulation is performed. The duration of each stage is 1 minute.
If there are no changes at the end of the step, the stimulation frequency is increased by 10-20 pulses/min. until a maximum frequency of 160 pulses/min is reached. After each stage of stimulation, the coronary circulation is assessed by changes in the ST segment on the ECG.
If, after reaching the maximum frequency (160 pulses/min.), no ischemic changes are observed on the ECG, then the stimulation time is extended to 2 minutes, after which a final assessment of the study is carried out. It is considered inappropriate to assess coronary circulation at a stimulation frequency of more than 160 pulses/min. at the same time, the number of false-positive results increases significantly, which is partly due to the so-called post-depolarization syndrome.
Post-depolarization syndrome is expressed in the occurrence of ST segment depression and T wave inversion on the ECG after the cessation of high ventricular frequency. The development of this syndrome after relief of paroxysm of ventricular tachycardia is well known.
In the absence of verified coronary artery disease in a patient, this syndrome indicates disturbances in the processes of ventricular repolarization not associated with deterioration of coronary circulation.
to the top of the page
Complications during TEES
It should be noted right away that paroxysmal rhythm disturbances, which were previously considered as a complication of the TEES method, are not currently such.
This is due to the rapid development of arrhythmology and changes in ideas. However, it must be borne in mind that the doctor conducting the study may encounter two problems:
1. when conducting TEES, the doctor consciously tries to provoke a paroxysm of supraventricular tachyarrhythmia using various stimulation modes, i.e. induction of tachycardia is the goal of the study itself. It is unlikely that this situation should be considered as a complication of the method;
2. when conducting TEES, the induction of tachycardia is a surprise for the doctor conducting the study and occurs for the first time in the patient’s life. Paroxysmal tachycardia can occur when using any stimulation mode. In this situation, the issue is not resolved unambiguously, but depending on the specific form of paroxysm.
The very fact of the possibility of provoking tachycardia indicates that all the necessary prerequisites for the implementation of the re-entry mechanism have been formed in the patient’s heart and only a trigger is needed for the occurrence of tachycardia.
This triggering mechanism was PPES. However, the same paroxysm can occur independently when certain conditions arise - most often the appearance of a supraventricular extrasystole in a certain phase of the cardiac cycle. Thus, provoking tachycardia for the first time in a patient’s life confirms only what may happen to him in the future and, to a certain extent, helps the doctor adjust treatment taking this fact into account.
The specific form of provoked paroxysm should also be taken into account, based on the complexity of treatment and possible complications of this paroxysm. Thus, a paroxysm of nodal AV tachycardia or a paroxysm of reciprocal AV tachycardia in a patient with WPW syndrome (orthodromic or antidromic variant) can be quite easily stopped using the TEES method and, as a rule, does not require intravenous administration of drugs (we must not forget about the possibility of stopping these paroxysms with using vagal tests).
Inducing a paroxysm of atrial fibrillation for the first time in a patient’s life requires further use of medications to stop it, since the TEES method does not stop atrial fibrillation.
Provocation of atrial fibrillation in a patient for the first time in his life often indicates either critical dilatation of the atria or pronounced dystrophic changes in the atrial myocardium [after myocarditis or chronic alcohol intoxication), after which maintaining sinus rhythm becomes a difficult task.
Particular attention should be paid to the development of two forms of paroxysmal tachyarrhythmia - ventricular tachycardia and atrial fibrillation in a patient with WPW syndrome, which, if they develop, should undoubtedly be considered as a complication of the method, associated in turn with a possible error in the study.
These situations should be reviewed and studied in detail to avoid their recurrence in the future. Provoking ventricular tachycardia using the TEES method is a difficult task due to many circumstances. It must be remembered that when affecting the atria, TES can provoke the development of ventricular tachycardia only indirectly through a combination of two unfavorable factors - deterioration of coronary circulation and electrical instability of the ventricles.
Knowing this, the doctor should be especially careful when, with the appearance of significant ischemic depression of the ST segment, ventricular extrasystole of high gradations (according to Lown) appears - frequent, paired, early. In this situation, the study should be stopped immediately, and the identified violations are reflected and emphasized in the study protocol as dangerous in terms of the development of paroxysm of ventricular tachycardia, and the patient himself should be considered as at risk of sudden cardiac death. Thus, the situation with the development of paroxysm of ventricular tachycardia during TEES can and should be controlled, the main thing is that the doctor conducting the study knows about it.
Complications of the TEES method
The problems that a doctor conducting a study may encounter are:
1. Insertion of the esophageal electrode into the trachea instead of the esophagus.
This complication usually occurs among doctors who are just beginning to independently conduct TEES research and is usually associated with their haste when inserting the probe into the esophagus. This complication extremely rarely occurs when the probe is slowly inserted at the moment of swallowing saliva, when the epiglottis rises and the trachea closes.
If the probe gets into the trachea, the patient experiences sudden suffocation, coughing, and redness of the face - the probe should be immediately removed, and the probe should be reintroduced only a few minutes after the described symptoms cease. In extremely rare cases, the erroneous insertion of a probe into the trachea is not accompanied by pronounced reactions on the part of the patient and stimulation is carried out from the trachea. In our practice, we observed one such patient (a former mountaineer, Honored Master of Sports).
To avoid such cases, it is necessary to pay attention to the extremely low amplitude of the “P” wave on the esophageal electrogram at the beginning of the study, as well as the appearance of cough when stimulation is turned on.
2. A burning sensation in the esophagus, behind the sternum.
The appearance of these sensations is mandatory when stimulation is turned on, and their absence in the patient should be associated with a malfunction of the equipment. The patient's level of sensation is usually low or easily tolerated. If the sensations are pronounced and the patient refuses the study, the study is stopped.
3. During stimulation, the patient feels pain in the back associated with contraction of the spinal muscles. In case of severe pain, the study is stopped.
4. When the stimulator is turned on, effective stimulation of the diaphragm occurs, which is accompanied by its rhythmic contractions with the frequency that the stimulator gives at a given time. The patient feels frequent hiccups or shortness of breath, and the doctor conducting the study observes frequent contractions of the diaphragm, which disappears immediately after the stimulator is turned off.
This complication most often occurs in patients with a hypersthenic physique or obesity, because the location of the heart in the chest in such patients is such that the heart practically lies on a highly located diaphragm and the poles of the esophageal electrode during TEES are located in close proximity not only to the atria, but also to the diaphragm. As a rule, the study is stopped when this complication occurs.
A technique in which the esophageal electrode is advised to be pulled up, thereby removing the electrode poles from the diaphragm, rarely gives a positive result, because by removing the probe from the diaphragm, we thereby remove the electrode poles from the zone of their optimal location in relation to the left atrium, and this in turn will require an increase in current strength and, as a result, the re-emergence of effective stimulation of the diaphragm. We observed a patient in whom contraction of the diaphragm during TEES occurred at the very minimum voltage and from the upper part of the esophagus.
5. Electrode getting stuck in the nose is the most unpleasant complication during TEES, as it injures the patient and leads to loss of the electrode.
The esophageal electrode gets stuck in the nose, usually when it is removed after stopping the study. The electrode gets stuck in the area of their poles, because their diameter is larger than the diameter of the probe itself. Electrode getting stuck is associated with injury to the nasal mucosa and its swelling when the probe is inserted. If it is impossible to remove the electrode after applying vasoconstrictor drops into the nose, it is removed as follows: holding the distal part of the probe through the mouth with a special clamp (used in the ENT office), bite the probe near the wings of the nose and remove the probe through the patient’s mouth. It should be emphasized that this complication occurs only among doctors who begin to independently perform TEES, who often forget the “golden rule” - insertion of the probe through the nose should be free and painless for the patient, and therefore atraumatic for the nasal mucosa. This is why anesthesia of the nasal mucosa not only does not help, but also harms when inserting a probe, since it is very important to know about pain when inserting a probe.
In conclusion of the presentation of this topic, it should be said that if the doctor conducting the study has good knowledge of TEES, arrhythmology, issues of cardiology, myocardial electrophysiology, the TEES method is safer compared to other methods of functional diagnostics that use physical activity or the administration of drugs as a load .
to the top of the page
Electrophysiological study of the heart - EPS
Contraindications
This type of research is strictly prohibited under the following circumstances:
- acute infectious disease or simply the presence of fever;
- heart attack or stroke in the acute stage;
- severe angina that occurs for the first time and progresses;
- in acute surgical pathology;
- in severe chronic heart failure or in its acute form;
- the presence of certain types of heart defects;
- if there is a suspicion of pulmonary embolism;
- diseases of the esophagus;
- the presence of cardiac or aortic aneurysms.
Proper preparation for the procedure
To undergo this procedure, the patient is referred after a complete examination by a cardiologist, arrhythmologist or cardiac surgeon. Before performing EPI, the attending physician conducts the following studies:
The patient will first of all have to carry tests for HIV, hepatitis, syphilis and blood clotting. These tests are necessary, since diagnosis using the electrophysiological study method will take place in a hospital, and the patient will have to be hospitalized.
- MRI or CT, these examinations are especially necessary if the patient experiences fainting, the doctor excludes the presence of brain pathologies;
- Ultrasound of the heart;
- 24-hour Holter monitoring;
- discharge summary with justification for the need for this procedure.
In addition, the patient himself must prepare for the upcoming examination. To do this he will need:
- fast for 8 – 10 hours;
- within a few days, stop drinking caffeine, alcohol and cigarettes;
- The doctor will stop the use of any medications.
Progress of the procedure
Considering that there are two types of research - invasive and non-invasive, there will be two ways to carry out the procedure.
Methodology for non-invasive EPI
The most commonly used non-invasive examination method, in which a catheter with an electrode is inserted through the nose or mouth, which is used somewhat less frequently. This method is also called transesophageal EPI or TEE. It is carried out in functional diagnostic departments, usually in the morning. The examination takes place as follows:
- Preliminary blood pressure measurement.
- Taking an ECG.
- The doctor explains the procedures and specifies what the patient will experience during the examination. There is usually a burning sensation in the chest, and this is normal.
- All manipulations usually take about half an hour.
- Through the nasal opening or, in rare cases, through the mouth, the doctor inserts a probe with an electrode into the patient, which is connected to special devices. Using equipment, stimulation of the heart muscle is carried out with electrical impulses. During this procedure, the heart begins to contract vigorously, as if under increased stress. All received data is recorded.
- An electrogram is recorded.
- The doctor carefully removes the catheter.
- A complete analysis of the collected information is carried out and a conclusion is made, which is sent to the attending physician.
- The tachycardia caused by the procedure will go away after some time, but if the discomfort continues for a long time, the doctor can provide medication.
Method of performing invasive EPI
In cases where TEE does not produce results or for some reason it is contraindicated, the doctor will prescribe endocardial or epicardial EPI.
Endocardial EPI
Before the procedure, the patient is placed in the department of cardiology, cardiac surgery or cardiac arrhythmology. EndoEPI itself is done in the department of X-ray surgical diagnostic methods. The patient is given an antisedative and taken to the operating room. Local anesthesia is performed. In complete sterility, the doctor makes an incision to insert a catheter into the femoral or subclavian vein. An introducer (metal or plastic guide) is inserted into the incision. A probe with an electrode is passed through it. The passage of the probe is observed on the screen. This is possible due to the available contrast agent. The probe is passed to the atrium or ventricle. The doctor performs electrical stimulation. All data is recorded using a computer.
This entire medical procedure lasts approximately half an hour. The patient should feel absolutely no discomfort. After removing the probe, apply a tight bandage to the insertion site.
Epicardial EPI
This study is carried out in the cardiac surgery department. The entire operation is performed under general anesthesia. The doctor dissects the chest and gains access to the pericardial cavity. Using electrodes, the doctor stimulates the epicardium. All data is recorded and then the wound is sutured. Typically, the operation lasts about an hour and is the most difficult area of examination using the EPI method.