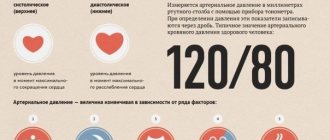
The generally accepted norm for blood pressure is a tonometer reading of 120/80, but deviations in both directions of these numbers are considered acceptable if they are isolated and do not accompany a deterioration in a person’s well-being. Regular pressure surges in one direction or another, if they occur at least several times a month, are considered hypertension or hypotension. But what if the device recorded a pressure of 110 over 90? What to do, whether you need to see a doctor right away and whether this condition is dangerous - today we will talk about this in detail.
What does the strange combination of numbers on the blood pressure monitor mean?
The normal upper limit for a person's blood pressure is 120 mmHg, but it can be lowered by several factors. This is hot weather, general malaise due to a cold, the first trimester of pregnancy and simply chronic lack of sleep. Therefore, if the systolic reading has dropped to 114–115 units, there is no reason to panic.
But a lower pressure of 90 against the background of a normal upper pressure, especially if such instrument marks are recorded regularly, already indicates existing malfunctions in the body. What do the numbers on the tonometer mean? Pressure measurement indicators characterize two phases of cardiac muscle activity:
- the first indicator describes the functioning of the heart at the moment of its tension, with what force the blood is pushed from the ventricles into the arteries - it is called systolic (or upper);
- the second indicator indicates the moment of relaxation of the main organ of the human body, when the heart is ready to accept a new portion of blood - it is called diastolic (or lower).
No less important is the pulse pressure indicator - this is the difference between the upper and lower blood pressure numbers. Normally, the difference between systole and diastole is 35-55 mmHg. A single deviation from the indicators is not pathological. But how do you understand that a pressure of 110 over 90 is observed on a regular basis?
Doctors may suspect the cause of such tonometer readings in the following factors:
- borderline norm of pulse pressure with a minimum difference of 20 units;
- the initial stage of isolated diastolic hypertension, when only the lower pressure indicator increases;
- absence of serious diseases, but a signal from the body about the need to change lifestyle - give up junk food, play sports, quit smoking and drinking alcoholic beverages;
- the first signs of severe pathologies such as malignant neoplasms, atherosclerosis of the heart and blood vessels and other diseases of the cardiovascular system.
In any case, if blood pressure constantly rises only at lower levels, you should not delay visiting a doctor. Isolated diastolic hypertension is a diagnosis that doctors are increasingly making due to poor nutrition, frequent stress, and bad habits.
Examinations that need to be completed
Diagnosis is carried out on an outpatient or inpatient basis. Depending on the patient's condition.
Full list of studies:
- Orally questioning a person about his complaints.
- Anamnesis collection. Lifestyle, existing diseases, not necessarily those of the cardiovascular system, family history, and other factors are taken into account.
- Measurement of blood pressure and heart rate. Calculating PD does not present any great difficulties. Heart rate will additionally indicate the nature of the activity of cardiac structures.
- Electrocardiography. Allows you to assess the functional state of the myocardium. Makes it possible to identify developmental defects, as well as various types of arrhythmias. The ideal moment for this is the peak of the pathological condition.
- Daily monitoring. Blood pressure and heart rate are to be examined. The only difference is that they are recorded over 24 hours, over time. While the patient lives in familiar conditions, his health status is recorded.
- Echocardiography. Ultrasound research technique. Used to detect anatomical defects. Against the background of defects, congenital and acquired, these are obvious.
- General blood test, hormones and biochemical.
- Urine examination as needed.
- MRI of the brain.
- EEG.
- Scintigraphy.
It is possible to expand the presented list. Not only the cardiologist is involved in the diagnosis. If a cardiac origin of the drop in pulse pressure is excluded, other specialists are involved.
Causes of pathology
If a cardiologist diagnoses isolated diastolic hypertension, this means that the pathology occurs in one of two types. The disease can be symptomatic, that is, it is considered as a response to internal problems and pathological processes occurring inside vital organs. Or the pathology is independent, when an isolated increase in lower pressure entails consequences from other organs and systems.
What reasons can cause an increase in the lower reading of the tonometer:
Blood pressure 110 over 100 - what does this mean?
- Diseases of the kidneys and adrenal glands. Hormones secreted by the adrenal cortex take part in vital processes in the body. If too many substances are produced, various diseases develop, for example, hypertension or excess potassium in the blood plasma. To determine the relationship between isolated diastolic hypertension and problems with the renal system, computed tomography or magnetic resonance imaging is performed. Although not only an increase in the production of hormones by the adrenal glands is dangerous for humans, their deficiency also adversely affects the condition of all organs and systems.
- Pathologies of the thyroid gland. Women are more susceptible to them than men due to constant changes in hormonal levels (during body growth, gestation, menopause). The thyroid gland directly affects a person’s emotional and physical health, his mood, appearance and well-being. Fluctuations in diastolic pressure may indicate an excess of hormones produced by the thyroid gland (thyrotoxicosis) or a lack of them (hypothyroidism).
- Excess fluid in the body. Lower pressure in this situation increases due to improper functioning of the kidneys, which control the level of fluid in the tissues. If the balance between sodium ions and water is disturbed, the body tries to dilute the amount of the element in the cells and accumulates water. The most common causes of fluid stagnation and increased diastolic pressure are pregnancy, menstruation, hot weather, allergic predisposition and excessive consumption of salty foods.
- Diseases of the spinal column. The spinal canals narrow due to congenital or acquired diseases, and problems arise more often in old age. The pathology is indicated by constant pain in the lumbar region, radiating to one leg, which is aggravated by physical activity. At a young age, increased lower pressure and problems with the spine are caused by congenital defects in the structure of the organ.
- Atherosclerosis. If the body's production of renin (a hormone that controls blood pressure levels) is impaired, diastole surges can be permanent. In addition to isolated diastolic hypertension, the patient will experience signs of narrowing of the lumen of the capillaries, a decrease in vascular tone and the formation of atherosclerotic plaques.
Less serious causes of pathology include poor diet, exposure to stress, smoking, alcohol abuse and obesity. A person is able to regulate such factors himself, after which blood pressure levels return to normal and general well-being improves.
Recommendations
Next, we consider the recommendations of specialists in the case of hypotension in elderly patients and pregnant women, as well as in cases of hypertension in children under 5 years of age.
For pregnant
If hypotension is physiological in nature and does not manifest itself as a violation of the woman’s condition, then the patient does not need treatment. It is imperative to monitor your blood pressure levels every time you visit an obstetrician-gynecologist or therapist. To normalize blood pressure, pregnant women will benefit from morning exercises, physical therapy exercises, water procedures (showers, douses, contrast foot baths), and massage. It is important to normalize sleep, the duration of which should be at least 9-10 hours a day.
For insomnia, the doctor may prescribe mild sedatives, but not barbiturate-based sleeping pills, as they are dangerous for the child. You should also diversify your diet. It should be rich in protein foods, fruits and vegetables. You can drink tea or coffee with milk only in the morning or afternoon; it is not recommended in the evening so as not to disturb your sleep. Women are also advised to take a closer look at herbal medicine recipes.
Important! The use of any remedies (both traditional medicinal and folk) during pregnancy should be discussed with an obstetrician-gynecologist.
For the elderly
The recommendations are as follows:
- Every day it is necessary to measure readings on both hands and record the data in a personal diary.
- You should get out of bed slowly so as not to provoke the development of orthostatic hypotension.
- It is important to have a hearty breakfast and drink a cup of weak coffee. Your daily diet must include foods rich in vitamins and minerals. If there are no contraindications, you need to drink enough liquid; you should not completely give up salt unless your doctor says otherwise.
- It is necessary to avoid prolonged stay in stuffy rooms, protect yourself from stress and significant physical exertion.
- Make time for walking and light exercise every day.
- If significant symptoms of hypotension appear, seek help from specialists.
Before using folk remedies to normalize blood pressure, it is necessary to exclude the presence of contraindications
For children
It is important to conduct a comprehensive examination to identify the cause of the pathology and select the necessary treatment, trying to return the numbers on the tonometer to normal without medications. What do we have to do? First of all, non-drug methods are used: changing the daily routine, adjusting the child’s menu, normalizing the ratio of rest and physical activity, etc.
Symptoms
Normal upper pressure and elevated lower pressure often go unnoticed at the initial stage. Even if a high diastole was once recorded during a routine examination by a cardiologist, a small number of patients pay attention to this and undergo the examination. Only in the second and third stages, during surges in lower pressure, does a person begin to experience pronounced symptoms of hypertension:
- attack of nausea with the urge to vomit;
- high pulse - 100 beats per minute;
- dizziness and nosebleeds;
- release of cold sticky sweat;
- noise and ringing in the ears;
- feelings of fear and anxiety;
- dyspnea;
- a rush of blood to the face, a feeling that the cheeks are burning;
- feeling of discomfort and pain behind the sternum.
When the lower pressure rises to critical levels, a person gets a headache, his vision may become blurred, and the picture before his eyes becomes double. Another characteristic symptom is a lack of coordination in space, when dizziness leads to fainting.
Why is increased lower blood pressure dangerous?
With a constant increase in diastolic pressure to 85–90 mmHg, the vessels experience enormous stress. They lose their usual tone, become fragile and inelastic. As a result, a person develops new pathologies and worsens existing ones.
If you ignore the symptoms of isolated diastolic hypertension, when the lower value is constantly growing, the risk of atherosclerotic plaques forming in the vessels and completely blocking their lumen increases. Plaques form only in arterial capillaries; venous ones are not affected by this pathology, since they do not consist of muscle tissue and do not experience excessive stress.
If earlier diastolic pressure was not given due attention, believing that only the upper reading of the tonometer was important, now doctors have come to the conclusion that both numbers are important. Increased diastole has three stages:
- first - the lower indicator rises to 90–100 mmHg;
- second – diastolic numbers reach 101–110 units;
- third – the lower threshold exceeds 110 mmHg.
This condition is constantly getting worse, which is why the risk of developing atherosclerosis increases, the condition of the capillaries worsens, and the body experiences a lack of oxygen. Dangerous consequences of untreated isolated diastolic hypertension are hemorrhage in the brain and retina, loss of visual function, and myocardial infarction.