- Thrombotic vascular lesions
- Fat embolism
- Air embolism
- Which vessels can be affected by embolism and how does it manifest?
- Carotid embolism
- Occlusion of mesenteric vessels and renal artery
- Peripheral vascular occlusion
- Treatment and prevention of pathology
- Prevention and treatment of fat embolism
- Prevention and treatment of air embolism
- Amniotic fluid embolism
- Causes
- Treatment and prevention
Vascular embolism is a condition in which the lumen of a blood vessel is completely or partially blocked. This leads to disruption of blood supply, which causes oxygen starvation of tissues. If left untreated, they gradually die off as the cells stop receiving oxygen and nutrients. Vessel blockage can be caused by:
- blood clots;
- particles of adipose tissue;
- air bubbles;
- foreign objects.
Regardless of the cause, vascular embolism poses a threat to the health and life of the patient. This condition requires treatment, which can be conservative or surgical.
General information
The amount of gas administered at a time must be at least 10-20 ml, otherwise the gas will dissolve in the blood without causing any harm. This pathology is considered quite rare; it accounts for no more than 2% of all possible vascular occlusions. It occurs with equal frequency in men and women and does not depend on age. Mortality with timely diagnosis and professional help ranges from 10 to 40%. Lack of medical care for thromboembolism of the pulmonary artery and brain leads to 90% mortality.
There are many reasons for such a malfunction, and a person may encounter a problem at home. The clinical picture is nonspecific, so it is possible to understand what happened only by comparing the picture, the symptom complex and the probable cause. This connection is used for urgent diagnosis, in addition, some objective methods are required. You need to act quickly, because there is usually no time to think longer.
Recovery depends on the form of the pathological process. As a rule, physiotherapeutic measures and manual manipulations are sufficient. Medicines are used later, when the health condition is at least partially normalized.
Causes
Spontaneous penetration of air into the circulatory system of a healthy person is practically impossible. The pressure in most vessels is too high compared to atmospheric pressure, so that gas will not be absorbed if the vessel wall is damaged. The exception is the internal jugular vein, where the pressure during inspiration is below atmospheric. The situation is different in patients with dehydration. Due to a decrease in the CEC, the pressure in the central tanks becomes negative; a violation of the integrity of the tank wall can lead to the ingress of gases from the environment.
There are two ways gas embolism during a dive occurs during ascent:
- Decompression sickness. DE develops when a diver is brought to the surface very quickly. When a person goes underwater, his body and the gases he breathes (oxygen and nitrogen) are under increasing pressure. The diver constantly uses oxygen, and nitrogen accumulates in the tissues of his body. If it rises to the surface too quickly from a great depth, due to a sharp pressure drop, the nitrogen does not have time to leave the body and forms gas bubbles in the vessels. It is convenient to explain this process using the example of a bottle of sparkling water. When the bottle is closed, the water contains no gas bubbles because it is under pressure. When opened, the pressure drops quickly, causing carbon dioxide to form visible gas bubbles in the water. As you gradually unscrew the cap, the pressure in the bottle will slowly drop and no air bubbles will form.
- Barotrauma of the lungs. If a diver holds his breath while quickly ascending from great depths, this can damage the lining of the lungs. When pressure drops as you rise, the volume of air in your lungs increases. If you hold your breath at this point, the air sacs in your lungs may rupture, allowing air to enter your bloodstream.
The most common causes of airway obstruction include:
- Injury. Atmospheric gases enter the bloodstream if the ventilator is not installed correctly or if the chest is damaged and blood vessels rupture. VE is also associated with injury to other anatomical sites if severe bleeding is not stopped promptly.
- If the venous sinuses rupture, gases can enter the placenta. During uterine contractions, air under pressure is forced into the damaged vessels. The disease develops regardless of the value of central venous pressure. Symptoms may appear not only immediately after childbirth, but also 1-2 days later.
- Healing procedures. Procedures with a high risk of developing VE include vascular, thoracic, and cerebral surgery if the venous sinus is opened during the procedure. In addition, air may enter the circulatory system if the infusion set is loosely connected to the central venous catheter or during infusion therapy. This can also occur with a negative IAP.
Air embolism can also be caused by iatrogenic causes, including:
- Hemodialysis is a treatment for kidney failure.
- Tissue filling during laparoscopic surgery.
- Open heart surgery.
- Lung biopsy.
- Contrast administration for X-ray studies.
- C-section.
Air embolism
Key points
- Air embolism can be either venous or arterial
- Risk factors can be classified into patient, operative and anesthetic factors
- Air embolism is sometimes difficult to detect - a high index of suspicion is required, taking into account possible differential diagnoses
- There are specific monitoring techniques to improve early detection of air embolism
- Management includes prompt recognition, minimization of further air entry, and support of affected organs
Introduction
There is a high mortality rate associated with air embolism.
Therefore, it is important for anesthesiologists to have an understanding of the risk factors, clinical presentation, risk reduction and recognition methods in order to promptly cope with pathological consequences. Any gas can lead to embolization if it is present in the vessel. Its characteristics, mainly solubility and volume, will determine the clinical manifestations. Air is the most common cause of this predominantly iatrogenic complication. Below are basic definitions of the different types of embolism. The clinical implications are different for each type.
Venous air embolism : Entry of air into the venous circulation causing occlusion or obstruction to distal flow.
Arterial air embolism : entry of air into the arterial circulation, occlusion of arterioles and distal hypoxemia resulting.
Paradoxical air embolism : Air passes from the venous to the arterial circulation, either through a congenital defect (eg, patent foramen ovale) or through the pulmonary circulation to the left side of the heart.
Risk factors
Any procedure carries a risk of air embolism if the surgical field is located above the right atrium and the vasculature is affected. The addition of a pressure gradient between the surgical field and the right heart increases the risk significantly. A small pressure difference of 5 cm water column. will result in 100 ml of air per second entering the bloodstream through a 14G cannula. When performing central venous catheterization, it is rational to position the patient with the head end down. Hypovolemia and the negative intrathoracic pressure that occurs during spontaneous inspiration also increase the pressure difference and therefore the risk.
Additional risks include circulatory access interventions such as central venous catheterization (causing air embolism) or the use of carbon dioxide during laparoscopic surgery (causing CO2 embolism). Air may also be involuntarily introduced through the vascular access.
Risk factors for air embolism can be classified into patient, operative, and anesthetic factors.
Operational factors
Venous embolism
- Craniotomy in a sitting position
- Posterior fossa surgery
- Spine surgery
- Shoulder surgeries
- Laparoscopic surgery (CO2 embolism)
- C-section
- Removal of the uterus from the wound
Arterial embolism
- Cardiopulmonary bypass surgery
- ECMO/installation of assistive devices
- Cardiac ablation
- Intracardiac bypass
- Carotid endarterectomy
- Laparoscopic surgery
- Interventional radiology
Anesthetic factors
Venous embolism
- Central venous access
- Pressure infusion
- Unidentified catheterization of epidural veins
Arterial embolism
- PEEP (paradoxical embolism)
Patient factors
Venous embolism
- Trauma: blunt and penetrating
- Hypovolemia
Arterial embolism
- Patent foramen ovale
Surgical procedures with a high risk of gas embolism include sitting craniotomy, posterior fossa surgery, and laparoscopic surgery.
It is important to note that air embolism can be detected without clinical manifestations, as shown in a study of cesarean sections by Law et al. The true incidence of air embolism associated with cardiac surgery is unknown, but cardiac surgery is considered an intermediate-risk surgical procedure for air embolism, with an estimated incidence of 5–25%. The neuropsychological consequences of open heart surgery and their relationship to air embolism have had a significant influence on the development of modern surgical approaches and lower-flow cardiopulmonary bypass designs.
The use of positive end-expiratory pressure (PEEP) during patient ventilation to minimize the risk of air embolism is controversial. The concept that increasing central venous pressure with PEEP (>5 cmH2O) minimizes the risk of air entry seems logical. Animal studies also suggest that PEEP may prevent venous air embolism in supine and head-elevated positions.
However, PEEP is a risk factor for paradoxical air embolism in patients with patent foramen ovale. In addition, PEEP may also have a significant effect on reducing preload due to decreased venous return secondary to increased intrathoracic pressure. A sudden decrease in PEEP may increase the rate of air entry into open venous vessels in the surgical field.
Clinical manifestations
Clinical manifestations depend on the rate of entry and volume of air. The venous route of air penetration leads to emboli entering the right side of the heart. A volume of 5 ml/kg is sufficient to cause an “air lock” in the outflow tract of the right ventricle, resulting in cardiovascular collapse and a catastrophic decrease in cardiac output. The critical volume of air that is lethal to humans is unknown, but based on animal experiments and case reports, it is estimated to be approximately 200-300 ml in adults.
The clinical effect of arterial embolization is highly site dependent. Air in small arterioles is usually compensated by collateral circulation and may be quite well tolerated in some organs. However, the heart, lungs and brain are especially sensitive and small volumes of air will lead to significant complications.
The immediate clinical manifestations of air embolism can be addressed using an organ system approach
Cardiovascular
A conscious patient may experience chest pain and palpitations associated with arrhythmia, and brady and tachyarrhythmia are possible. Ischemic changes may appear on the ECG. Small volumes of air accumulating in the right heart and pulmonary vessels will lead to a gradual increase in pulmonary artery pressure, which in turn leads to an increase in the tension of the right heart. Continued air entry is likely to be critical because the large volume of air in the right ventricle (RV) will lead to outflow obstruction and acute right ventricular failure. Decreased right ventricular outflow impairs left ventricular preload, leading to cardiovascular collapse.
In the left side of the heart, small volumes of air drawn into the coronary circulation, especially the left anterior descending artery, quickly lead to ischemia and cardiac arrest. There is also a risk of paradoxical air embolism in patients with a patent foramen ovale. Patent foramen ovale is accidentally discovered during postmortem examination in 35% of healthy people. Paradoxical air embolism usually results in symptoms of angina and/or embolic stroke.
Respiratory
A patient under anesthesia experiences a sudden drop in end-tidal carbon dioxide due to increased dead space caused by air in the pulmonary circulation. The degree of ventilation-perfusion mismatch is determined by the levels of hypoxemia and hypercarbia on arterial blood gas analysis. Air embolism can also trigger an inflammatory cascade, leading to acute lung injury and ARDS. The conscious patient develops sudden shortness of breath and pleural chest pain, and a dry cough may occur. Hemoptysis is a relatively late sign.
central nervous system
Arterial air embolism can lead to ischemic stroke, which may manifest clinically as an inability to awaken after general anesthesia. Rarely, abnormal pupillary response to light may occur if there is significant paradoxical embolism, leading to large ischemic infarction with subsequent mass effect. If the blood supply to the brainstem is disrupted, cardiac arrhythmia and apnea may occur. An awake patient may experience a sudden attack of confusion, dysarthria, or hemiparesis. The patient may fall into a coma as cerebral edema develops in the postoperative period. Gas bubbles can rarely be observed in the retinal vessels during fundoscopy.
Gastrointestinal
Arterial air embolism can lead to abdominal pain and intestinal ischemia.
Leather
Crepitation may be palpable over superficial vessels. Surgical emphysema is not usually associated with venous embolism unless it is a complication of a laparoscopic procedure.
In all cases of air embolism, a high level of suspicion is required and possible differential diagnoses .
Cardiovascular
- Myocardial ischemia/infarction
- Other causes of cardiogenic shock/failure
- Bleeding/hypovolemia
- Arrhythmia due to ischemia/electrolyte disturbances/conduction abnormalities/drugs
Respiratory
- PE/other embolism (eg, amniotic fluid)
- Pneumothorax
- Bronchospasm
- Pulmonary edema
central nervous system
- Hemorrhagic stroke
- Disorders secondary to medications/hypoxia/hypoglycemia/electrolyte imbalance
Immunological
- Sepsis
- Anaphylaxis
Prevention
High-risk procedures should be identified in advance and discussed prior to the surgical date and during the surgical team briefing. The discussion should include positioning the patient for the proposed procedure, as this may alter the preoperative evaluation (eg, performing transthoracic or transesophageal echocardiography to rule out a patent foramen ovale before sitting craniotomy). The anesthesiologist should consider the need for a central venous catheter or an air suction catheter. Contact between the surgeon and anesthetist is vital, especially during high-risk stages of surgery, as this will allow rapid action to be taken if air entry is suspected.
Careful attention to volemic status is important and maintaining preload will help reduce the risk of air infiltration. Various new approaches have been tried to minimize the risk of air embolism in recognized high-risk procedures by reducing the pressure gradient between the circulation and the air entry site. For example, the use of an anti-shock compression suit to increase systemic venous pressure. Recently, the use of intrajugular balloon catheters has been demonstrated in pigs to be effective in preventing air passage and partially effective in aspirating air.
Monitoring
Careful monitoring of patients is critical in the early detection of air embolism, allowing for early aggressive therapy and measures to prevent further air entry. It is the anesthesiologist's responsibility to remain vigilant and pay close attention throughout the operation.
Monitoring methods for detecting venous air embolism are discussed below. In routine clinical practice, specific monitoring methods are not used to detect arterial air embolism. Detection of arterial air embolism requires a high index of suspicion, close monitoring of clinical signs, coupled with prompt recognition of changes in routine monitoring, such as changes in end-tidal CO2 and ECG.
Changes in clinical parameters are not specific and often occur late, after a significant volume of air has entered the bloodstream. Therefore, although clinical judgment is important, it should not be relied upon solely unless resource limitations permit the use of the monitoring methods described below (minimum air volumes detected by this method are indicated in parentheses). Some methods can be used together to improve sensitivity (eg petCO2 with Doppler).
Non-invasive monitoring
Physical signs
- Advantage – regular monitoring, no additional costs
- Disadvantage – low sensitivity and specificity, late manifestation
End tidal carbon dioxide level (0.5 ml/kg)
- Advantage – affordable, high sensitivity
- Disadvantage – not specific to air, influence of perfusion pressure and respiratory pathology
End tidal nitrogen level (0.5 ml/kg)
- Advantage – high sensitivity and specificity
- Disadvantage - expensive and not always available, depends on perfusion and air ingress rate
Transthoracic Doppler (0.05 ml/kg)
- Advantage – sensitive and specific, easy to position
- Disadvantages - influence of obesity, interference from diathermy, lack of air volume indication, hidden by ambient noise, requires greater vigilance
Transcranial Doppler (0.05 ml/kg)
- Advantage – high sensitivity and specificity
- Disadvantages – training required to achieve competence in use, equipment located nearby/in the surgical field in some cases, limited availability
Invasive monitoring
Transesophageal echocardiography (0.02 ml/kg)
- Advantage: Excellent sensitivity and can detect embolus size, gold standard for detecting PFO
- Disadvantages – difficult to distinguish air from fat/thromtosis, limited availability and training required, expensive, equipment in/near the surgical site, risk of esophageal injury
Pulmonary artery catheterization (0.25 ml/kg)
- Advantage: widely available and quite sensitive
- Disadvantage – limited specificity for venous air embolism, risk associated with placement, does not promote air aspiration, expensive
Central venous catheter
- Advantage: Cheap and readily available, can help remove air from the right atrium, administer inotropes
- Disadvantage: installation complications, risk of air embolism during installation and removal
Future developments may include the simultaneous use of infrared spectroscopy as a means of monitoring regional saturations along with other monitoring techniques such as electroencephalography. These methods are still in the experimental phase of animal studies and require confirmation according to current monitoring standards.
In cardiac surgery, there are algorithms that use transesophageal echocardiography to detect and treat air embolism during surgery. Transesophageal echocardiography has the highest sensitivity of all air embolism monitoring devices, with volume detection of 0.02 mL/kg—approximately 10 times the sensitivity of transthoracic Doppler.
Clinical management
Supportive care forms the basis of clinical management of venous and arterial air embolism diagnosed in the perioperative period. Leading can be further divided into three elements, which are invariably applied simultaneously:
- Immediate resuscitation
- Preventing further air entry
- Efforts to remove incoming air
Immediate resuscitation is best achieved by approaching the airway, breathing and circulation. In an anesthetized patient, the airway should be secured by endotracheal intubation if this has not already been done. It is important to ensure that the oxygen fraction is increased to 1.0 and that adequate ventilation is maintained. This can be confirmed by an arterial blood test. Profound cardiovascular collapse and cardiac arrest may quickly follow significant venous or arterial air embolism.
Circulatory support should be started immediately to increase venous pressure. This includes fluid infusion through large bore intravenous cannulas, vasopressor or inotropic support if required. If cardiac arrest is imminent or has occurred, the initial rhythm may be pulseless electrical activity or asystole, in which case an advanced life support protocol for rhythms not requiring defibrillation should be followed. When paradoxical or arterial embolism is suspected, signs of cardiac ischemia should be monitored and a 12-lead ECG should be performed postoperatively.
Attention should be given to preventing further air entry by lowering the surgical field relative to the level of the heart and by stopping any process that may allow air entry (eg, drilling into bone during prosthetic surgery). Air flow can also be reduced by temporarily compressing major blood vessels, applying bone wax, flooding the surgical site with liquid, and applying wet wipes to suspected areas. Any cavity with gas pressure (eg pneumoperitoneum) should be drained. The supply of nitrous oxide should be interrupted as it can expand any gas filling the intravascular space.
You can try to aspirate air through a central venous catheter or an air suction catheter (a 16G multi-perforated catheter that can be inserted centrally or peripherally if it is long enough). It is preferable to use a catheter with a multi-perforated tip to increase the chances of aspirating air. The tip of the multiperforated catheter should be positioned approximately 2 cm distal to the junction of the superior vena cava and the right atrium. If a single-lumen catheter is used, it should be positioned 3 cm from the superior vena cava/atrium junction. Radiological or intravenous ECG monitoring is recommended but is not always used in practice or available.
To aspirate air emboli most effectively, use the Trendelenburg and left lateral positions, since any air inside the heart should then theoretically move to the right atrium. In practice, it is not easy to perform such rapid aspiration unless a suction catheter or central venous line is already in place. The logistics of moving the patient can also be difficult due to the simultaneous resuscitation and open surgical field. If a pulmonary artery catheter is in place, it is unlikely to be effective at aspirating air because the lumens in the catheter are small and the catheter will not be in the optimal position for aspiration due to the nature of their intended use.
Air embolism syndrome
Case reports suggest that air embolism may lead to systemic inflammatory response syndrome with subsequent multiple organ dysfunction.
Two pathophysiological theories have been proposed. The first suggests that air emboli cause microvascular occlusions leading to tissue ischemia with subsequent inflammation and organ dysfunction. This does not, however, explain why some patients with seemingly low air intake develop such a severe systemic inflammatory response. This is especially true in cases of paradoxical embolism.
The second theory is related to the mismatch of the gene environment. Infection with some gas-producing pathogens results in the formation of intravascular gas, which can act as a trigger for the innate immune system. The same mechanism that may benefit the body during such an infection can have detrimental effects during an air embolism. The presence of an air bubble in the circulation activates platelets, which can lead to systemic inflammation, disseminated intravascular coagulation, and multiorgan dysfunction.
Treatment of air embolism syndrome is based on organ-conserving therapy in the intensive care unit.
Summary
Air embolism can occur in the venous, arterial system, or paradoxically, when air passes from the venous to the arterial circulation. Risk factors can be considered operative, anesthetic and patient factors. Monitoring methods allow early detection of venous air embolism. Management includes resuscitation, prevention of further air entry, and support of organ function.
Dr. Adam Low, Dr. Naginder Singh Anaesthetic Registrars, Queen Elizabeth Hospital Birmingham, UK Dr. Hari Krovvidi Consultant Anaesthetist, Queen Elizabeth Hospital Birmingham, UK Edited by Dr. Clara Poon Consultant Anaesthetist, Queen Mary Hospital, Hong Kong
2016
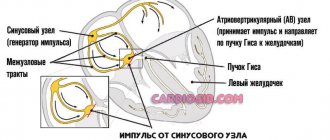
Pathogenesis
Large air bubbles in the bloodstream can block any blood vessel. The most commonly blocked veins are the pulmonary veins, the vessels of the heart, and the arterial trunks that supply blood to the brain. When the pulmonary artery is damaged, regional intravascular hypertension, RV overload and acute right ventricular failure are observed. Subsequently, the left ventricle is damaged, cardiac output decreases, peripheral circulation is impaired and shock occurs. PA air embolism is accompanied by bronchospasm, ventilation-perfusion imbalance, pulmonary infarction and respiratory failure.
When blood flow in the vessels of the brain is disrupted, the formation of pathology occurs as an ischemic stroke. The blood supply to a certain area of the brain is disrupted, the nerve tissue is depleted of oxygen and dies. An area of necrosis forms, and numerous small hemorrhages appear in the brain tissue. The further course of the disease depends on the location of the lesion. Paresis, paralysis, cognitive deficits and dysfunction of internal organs are possible.
Etiology
The immediate cause of a pulmonary embolism is a blood clot. It is formed under the influence of various factors. The most common among them are:
- Stagnation of blood in the venous vessels of the lower extremities,
- Inflammatory changes in the venous wall,
- Chemotherapy and hormone therapy that increase blood clotting,
- Hypercoagulation,
- Prolonged immobility, disrupting normal blood circulation,
- Venous stents and prostheses,
- Long-term use of diuretics, leading to dehydration and blood thickening,
- Surgical operations and invasive procedures with catheterization of large veins,
- Pregnancy, childbirth, postpartum period,
- Smoking,
- Elderly age,
- Sedentary lifestyle,
- Excess weight.
To prevent pulmonary embolism, people at risk need to take medications that thin the blood and reduce its viscosity. Office workers, truck drivers and flight attendants are most susceptible to blood stagnation in the legs. They develop embolism more often than others. To avoid serious pathology, they need to periodically undergo medical examinations and special examinations that detect vein thrombosis. Lifestyle changes and feasible physical activity are the main preventive measures for pulmonary embolism.
Diseases in which pulmonary artery blockage most often occurs:
- thrombophlebitis of the deep veins of the leg, thrombosis of the inferior vena cava and its tributaries;
- Varicose veins;
- cardiovascular pathologies – ischemic heart disease, rheumatism, heart defects, arrhythmia, hypertension, infective endocarditis, cardiomyopathy, myocarditis, heart failure;
- sepsis;
- cancer of internal organs;
- oncohematological diseases - hemoblastosis, erythremia;
- DIC syndrome;
- acute cerebrovascular accident;
- some autoimmune processes;
- congestive cardiac and respiratory failure;
- endocrinopathies and metabolic disorders;
- hemostasis disorders - thrombophilia;
- injuries with fractures of large bones;
- inflammatory bowel diseases;
- nephrotic syndrome;
- obesity;
- epilepsy.
Classification
There are several criteria for VE classification. Air embolism is classified depending on the nature of the course (fulminant, acute and subacute), the way air enters the bloodstream (iatrogenic, traumatic) and the direction of embolism (orthograde, retrograde, paradoxical). In clinical practice, a division of the form of the disease is used depending on the type of damaged vessel, including the following pathology options:
- Arterial. There is blockage of large arterial trunks (coronary, pulmonary, cerebral). Occurs in 30-35% of cases, occurs suddenly, severely and with clear clinical symptoms. The patient dies within hours and sometimes minutes. More than 40-50 cm3 of gas is required to produce AVE, and it enters the bloodstream at the same time.
- Ven. Detected in 65-70% of cases. This leads to disruption of venous outflow. Symptoms progress relatively slowly and life-threatening conditions are rare. Tendency to subacute course. Occlusion of small veins and vessels can be asymptomatic; blood flow occurs through the collateral system. An exception is obstruction of the airways of the pulmonary veins, which carry oxygenated blood from the lungs to the heart.
A comment
The team of authors provides a clinical observation of the development of venous and paradoxical air embolism in a patient with a brain stem tumor. This is a very serious and sometimes fatal complication of neurosurgical operations performed on patients in a sitting position. The article discusses various approaches and methods previously published by domestic and foreign researchers, aimed at both preventing the development of air embolic complications and their treatment. Algorithms for pre- and intraoperative examination and patient management are discussed. During the discussion of this clinical observation, the authors provide literature data on the possible causes of venous and paradoxical air embolisms in neurosurgical practice.
In the presented clinical case, a paradoxical air embolism that developed during neurosurgical intervention in a sitting position led to the formation of acute myocardial infarction and cerebrovascular accident, which ultimately caused the death of the patient. The authors focus readers' attention on methods for pre- and intraoperative diagnosis of these complications, pointing out that effective methods for treating venous and paradoxical air embolism have not currently been developed. The authors come to a conclusion, one of which indicates the need to switch to performing neurosurgical interventions in the supine position in all technically possible cases and to avoid surgery in the sitting position as much as possible to reduce the risk of developing air embolic complications.
The article may be useful not only to neurosurgeons and anesthesiologists-resuscitators, but also to all related specialists involved in the treatment of patients with brain damage.
S.V. Sviridov (Moscow)
Symptoms and clinical manifestations
The clinical picture is nonspecific. Without special techniques it is impossible to understand the nature of the underlying disorders. The symptom complex depends on the location and type of damaged vessel.
Venous embolism
When veins are affected, a fairly large volume of air is required before any obvious disturbance occurs. Approximately 2-3 ml is potentially fatal. The venous form usually develops against the background of trauma or iatrogenic (therapeutic) interventions.
An approximate list of symptoms of air embolism in veins:
- Pain at the location of the vessel. Usually these are the elbow bends, places where catheterization was performed, places of injury with a violation of the anatomical integrity. The intensity varies. From minimal, barely noticeable pain and pressure to unbearable shock, depending on the body and the degree of blood flow impairment.
- Muscle weakness. It is specified by a violation of local tissue nutrition. This does not always occur and is not considered a universal symptom.
- Contractions. Painful cramps, muscle spasms. Associated with severe damage to the central nervous system or the blood vessels themselves due to insufficient tissue nutrition. These are usually myoclonic contractions. They are practically painless. One way or another, people experience them from time to time. A classic example is a tic or twitching of the eyelid. Only in this case does spontaneous contraction of the muscles or tissues of the limb occur, which were the “gate” for the air bubble.
- Fall in blood pressure. Not always either. It rarely reaches critical levels. Caused by disruption of the small circulatory system and pulmonary structures.
- Increased fatigue. Asthenia. That is, the inability to perform household duties, lack of energy to perform professional functions, increased drowsiness, problems with coordination of movements, decreased speed of thought processes.
- Nausea, vomiting. These are quite rare events.
Usually this is limited. It is relatively rare that such a large amount of air enters the body that the right ventricle becomes overloaded, which leads to critical impairment of blood oxygenation and increased pressure in the pulmonary artery. This process can lead to the death of the patient. Urgent treatment and resuscitation are required.
But more often there are blockages with small air bubbles. Then there is no clinical picture at all. The abnormal factor enters the lungs through the veins and is excreted naturally.
However, patients must be closely monitored. If even minimal symptoms appear, immediate medical attention is required. This is a good precaution because if you are in a hurry, you may misjudge the situation.
Arterial embolism
This is a little more common for many other reasons. This is extremely dangerous for the health and life of the patient and is always characterized by a clear clinical picture.
- Discomfort in the limbs where the air bubble enters the body.
- Loss of sensation in the arms and legs, muscle weakness and loss of control of movement. Full or partial. Talk about paralysis or paresis respectively.
- Arrhythmia. A type of sinus tachycardia in which the number of heartbeats increases to 90 or more. Other abnormal changes in the body are also possible. The condition itself is fatal. If cardiac arrhythmia is not corrected in time, it can be fatal.
- Skin vitality. This happens when, on the one hand, there is a pronounced disturbance in tissue nutrition, and on the other, disturbances in the functioning of the heart. Both are equally dangerous. Otherwise it is called cyanosis.
- Neurological symptoms. Decreased visual acuity, hearing, coordination of movements and other similar problems.
- Reduced speed and efficiency of thinking, fatigue and asthenic phenomena, insomnia at night and the urge to lie down during the day, apathy is also included.
- This also applies to behavioral and mental disorders. They are caused by a decrease in the quality of brain nutrition. May be caused by a stroke, the nerve fibers of the brain structures die. The embolism is accompanied by a hallucinatory syndrome, the patient sees pictures and hears what is not there. There is also a delusional component. Both of these symptoms are very unfavorable from a prognosis point of view and indicate poor oxygen supply to the brain. Hypoxia leads to the death of nerve fibers and soon leads to death. Immediate treatment is required.
- Itchy skin. Relatively rare, but also possible.
- Trembling of fingers, hands, head. The so-called tremor.
- Shortness of breath, disruption of the natural process of gas exchange. This occurs when the pulmonary artery or the heart itself is damaged. This is life-threatening as it can cause spontaneous cardiac or pulmonary arrest. Both are deadly.
- Chest pain. How does angina occur? Hard, intense. Less than half of the situations involve minimal discomfort.
- The cough is productive, producing foamy sputum with traces of blood.
Symptoms of air embolism due to arterial occlusion are much more varied and expressive. The danger is also much greater. The pathological process requires immediate attention. In some cases there is no time for emergency measures.
Symptoms
Pulmonary embolism has no specific symptoms and is often not recognized in time. The disease is easily confused with a dysfunction of the cardiovascular and bronchopulmonary systems. Without the results of laboratory and instrumental studies, it is impossible to make a diagnosis.
The main manifestations of acute pulmonary embolism are distinguished by their sudden occurrence and lack of relationship with other pathologies - pneumonia, myocardial infarction, cardiovascular failure. Symptoms of the disease:
- Chest pain, reminiscent of “cardiac toad” and intensifying with a deep breath, coughing, or changing body position.
- Shortness of breath, suffocation – intermittent and difficult breathing that occurs suddenly even with the slightest physical activity.
- Cough with bloody brown sputum.
- Arterial hypotension up to collapse.
- Rapid and irregular heartbeat - tachycardia, arrhythmia.
- Pale skin with acrocyanosis.
- Swelling and pain in the calf muscles of both legs.
- Sticky and moist skin is hyperhidrosis.
- Fever is a rise in body temperature to febrile levels.
- Dizziness, convulsions, loss of consciousness.
typical view of a patient with pulmonary embolism
Pulmonary embolism may be asymptomatic
. In severe cases, patients experience nothing but pain and quickly die.
There are several clinical forms of pathology, which differ in the leading syndrome:
- The pulmonary-pleural form is manifested by shortness of breath, cough, hemoptysis, chest pain, cyanosis of the face and neck.
- Cardiac – discomfort and pain in the chest, tachycardia, arrhythmia, swelling of the neck veins, systolic murmur, strong heartbeat, arterial hypotension, collapse.
- Abdominal - is rare and is accompanied by epigastric pain, vomiting, belching, hepatomegaly, heaviness in the right hypochondrium, stool disturbances, bloating, rumbling and other signs of intestinal paresis.
- Cerebral - occurs with atherosclerotic damage to the cerebral arteries, mainly in elderly people. Its symptoms are: headache, tinnitus, nausea, seizures, loss of consciousness, hemiparesis, psychomotor agitation or coma, involuntary release of feces and urine.
- Renal - development of secretory anuria after the patient recovers from a state of shock.
- Febrile - prolonged and febrile fever is caused by inflammation of the pleura and lungs.
- Immunological - the presence of CEC and eosinophilia in the blood, the development of pleurisy and pneumonitis, the appearance of a characteristic rash on the skin.
Clinical signs of pulmonary embolism are very diverse and non-specific. Their severity depends on the size, location and number of emboli, as well as the initial cardiorespiratory status of the patient.
Diagnostics
The most important part of diagnosing gas embolism is interviewing the patient, as the symptoms are similar to many other diseases. The presence of a diving expedition or a specific surgical procedure at the interview indicates the possibility of air embolism. Surgeries such as craniotomy, caesarean section, hip replacement and heart surgery with cardiopulmonary bypass are considered to be potentially dangerous in the development of this condition.
If an air embolism is suspected or the above procedures are performed, the following tests are usually recommended:
- Chest X-ray. Gas bubbles sometimes show up on X-rays.
- Stethoscopy (auscultation of the lungs using a stethoscope). “A trained ear can hear a peculiar symptom - the “rustle of a mill wheel.”
- Measuring the gas composition of exhaled air. If the patient is under anesthesia, the anesthesiologist may detect a decrease in the amount of carbon dioxide exhaled.
- Dopplerography. A test that evaluates blood flow through blood vessels. This type of ultrasound is typically used for surgeries with a high risk of air embolism.
- Transesophageal echocardiography. This technique uses sound to produce a highly detailed image of the heart and surrounding vessels.
When diagnosing the disease, it is important to determine the area of the vessel affected by the embolus. The first step is a physical examination of the patient. The most effective physical examination methods are precordial, transesophageal, or transcranial Doppler.
Diagnostic measures
Diagnosis of pulmonary embolism is aimed at detecting a blood clot, assessing hemodynamic disturbances, and identifying the cause of the process to prevent relapses. To solve these problems, specialists carefully examine patients: collect complaints and anamnesis, study risk factors and clinical symptoms. To make a diagnosis and prescribe treatment, the results of laboratory and hardware tests are necessary. General clinical and biochemical parameters, gas composition, blood clotting factors and enzymes are determined in the blood.
A highly sensitive but nonspecific laboratory method is the detection of D-dimer, a fibrin breakdown product. If its level increases, recent thrombus formation is assumed. A normal D-dimer value helps rule out pulmonary artery thrombosis in patients.
Instrumental research methods play a more important diagnostic role. These include:
- Electrocardiography - detection of sinus tachycardia with a high P wave, deviation of the electrical axis to the right, increased amplitude of the R and S waves, displacement of the ST segment, negative T wave.
- X-ray examination of the lungs - with embolism, the pulmonary arteries are dilated, the number of contrasted peripheral branches is reduced, and the pulmonary pattern is deformed.
X-ray signs of pulmonary embolism (Fig.: NSC “Institute of Cardiology N.D. Strazhesko”)
- Pulmonary angiography is a radiopaque examination of the pulmonary artery, which allows one to detect blood clots and damage in it.
- Perfusion scanning of the lungs is a highly informative method that determines perfusion defects, their area, and the degree of reduction in radioactivity. A decrease in the accumulation or complete absence of an isotope preparation in the lung area indicates a circulatory disorder in this area.
- SCT is a standard non-invasive technique that allows you to visualize the pulmonary artery, assess its condition, and detect blood clots in it. This procedure is easy to perform, highly sensitive and specific.
- Echocardiography - detection of blood clots in the cavities of the heart, identification of signs of pulmonary hypertension, exclusion of heart defects and myocardial pathology. The right chambers of the heart are dilated, the interventricular septum bulges to the left and makes paradoxical movements during the relaxation phase.
- Angiography of pulmonary vessels is an invasive diagnostic method that reveals a filling defect in the lumen of the artery or complete obstruction with “amputation” of the vessel and breakage of its contrast. In this case, the branches of the pulmonary artery are sharply narrowed. Slow removal of the contrast agent is observed.
Diagnosis of pulmonary embolism is a complex process. Nonspecific symptoms of the pathology often mislead doctors.
Standard methods of examining a patient can only exclude other diseases: inflammation and pulmonary edema, acute coronary insufficiency. An untimely or incorrect diagnosis is the cause of death of the patient.
Features of therapy
The consequences of air entering the blood vessels are treated with medications and devices. The amount of care required depends on the patient's condition, the severity of the impairment of vital functions and the availability of the necessary equipment in the clinic. Typically, the rehabilitation scheme includes the following treatment methods:
- Nonspecific drugs. Treatment is aimed at minimizing the clinical symptoms of the disease and preventing complications. The patient is prescribed steroid hormones, cardiotonics, loop diuretics, vasodilators, and antioxidants. At the recovery stage, multivitamin complexes and nootropic drugs are used. In case of severe respiratory failure, the patient is transferred to a ventilator in forced ventilation mode.
- Equipment. Hyperbaric oxygen therapy and controlled hypothermia are used to treat air embolism. Hyperbaric oxygen therapy is carried out at a pressure of 2 to 3 atmospheres, and the number of sessions varies from 5 to 12. The duration of each session is 45 minutes. In case of hypothermia, the patient's body is cooled to 34 ° C. Both barotherapy and cold help increase the solubility of gases in the blood, which allows the removal of clots that cannot be removed surgically.
- Effective. The best method for clearing intracardiac PE blockage is aspiration through a subclavian catheter. This involves removing several hundred milliliters of blood, which may require massive fluid resuscitation or blood transfusion. If the blockage is precisely located, the vessel or venous sinus can be opened.
If a dangerous condition occurs, you must immediately take action and begin treatment. To do this, the patient should lie on his left side and slightly lower his upper body. The person will be taken to the ambulance on a stretcher, lying on his stomach with his head tilted to the side.
Treatment can only be carried out in a hospital setting and under the strict supervision of a doctor. The situation is complicated by the fact that it is not always possible to take effective measures in a timely manner. Death often occurs before first aid is provided.
If a critical condition occurs within the walls of a medical institution, for example, during an operation or an injection, the nearest doctors have time to take all necessary measures to save the person. In this case, the chances of recovery are many times greater.
To save the patient, doctors will take the following steps, taking into account the cause and complexity of the disease:
- Stopping further air supply to the vessels. To do this, surgical hemostasis is performed, treating the affected area and affected vessels with saline solution.
- The patient will have to take a different body position. If the air bubble pierces the heart, the patient is tilted to the left and the tip of the head is lowered. This is necessary to ensure that air enters the right atrium or right ventricle. The air will then be aspirated through the catheter or lancing device.
- If necessary, the patient will be given additional oxygen inhalation.
- If air has moved from the vessels into the brain, oxygen therapy will be prescribed and the patient may be placed in a pressure chamber.
- In cases where an air embolism causes circulatory problems, cardiopulmonary resuscitation is used. This procedure is based on artificial respiration and chest compressions.
- In some cases, the doctor may try to aspirate air from the vein using a catheter.
- Pressure on the neck and increased venous pressure will help block the flow of blood from the veins, preventing further air flow and allowing blood to flow into open veins.
- Your doctor may prescribe medications to stimulate your heart.
- In case of cerebral edema, treatment with steroid drugs is recommended.
- After treatment, the patient should be under the supervision of the attending physician for as long as necessary to avoid complications.
Treatment of VE in divers
If a diver develops VE after a rapid ascent from deep water, the only effective treatment is immediate recompression therapy in a pressure chamber (hyperbaric chamber). The diver must be in a horizontal position and breathing 100% oxygen before entering the pressure chamber.
Recompression involves staying for several hours in a pressure chamber in which a person breathes a mixture of gases and oxygen under high pressure. Increased blood pressure can restore normal blood flow and oxygen supply to tissues, as well as reduce the size of air bubbles in blood vessels.
After recompression, the pressure is gradually released, allowing excess gases to escape from the housing without forming bubbles. Treatment may take several days depending on the severity of symptoms.
Treatment of iatrogenic (medical) EV
If VE is caused by medical procedures and air has accumulated in the heart, interfering with its function, the patient must be placed in a certain position:
- Trendelenburg position - the person lies on his back, the pelvis and legs are elevated above the level of the heart.
- Left-sided position - the patient lies on his left side, as a result of which the air in the heart moves towards the apex of the right ventricle. This prevents or minimizes obstruction (blockage) of the pulmonary artery.
- If the patient has a central venous catheter, you can try to aspirate (“draw in”) air from the right side of the heart.
- The patient is also prescribed oxygen therapy. This accelerates the compression of the gas bubble. In such cases, repeated compression in the pressure chamber is also useful.
Treatment
With the development of decompression sickness, it is recommended to place the victim in a pressure chamber for several hours. This will naturally dissolve gas bubbles in the bloodstream.
The effect directly depends on the severity of the lesion. As a rule, a positive result is achieved in more than 80% of situations.
Against the background of iatrogenic, medically caused lesions, it is necessary to place the patient in a horizontal position. He should lie on his back with his legs raised above the level of the heart or on his left side to reduce the load on the pulmonary artery.
Doctors suggest that the problem is gradually being reduced and will disappear.
In the absence of a clinical effect within 2-3 hours, the issue of surgical treatment is decided; in this situation, doctors take measures to mechanically “suck in” the air bubble in order to eliminate the blockage of the vessel, normalize tissue trophism and cellular respiration.
The procedure itself is not easy, because there is a high probability of making a mistake with the location of the source. For this reason, a thorough assessment of the patient’s condition, diagnostics and verification of the results using several instrumental methods are required.
Other methods do not make much sense in the acute phase. Therefore, neither drugs nor other methods are used.
- As you recover, cerebrovascular drugs such as Actovegin and Piracetam may be prescribed. They normalize brain nutrition.
- Nootropics to restore the speed of metabolic processes.
- Antihypertensive drugs of several groups, cardioprotectors (Mildronat, Riboxin). Allows restoration of cardiac function, disturbances during gas embolism.
- It is possible to use glucocorticoids in the development of inflammatory processes and edema.
In the future, it is recommended to regularly see a cardiologist for preventive examinations. There may be tissue damage that is not obvious at first, but makes itself known later.
It makes sense to get checked every six months or a little less often. Avoidance of injuries, caution when diving, and safety precautions are mandatory. If the patient intends to continue this activity.
In case of severe damage to the lungs, brain, heart and blood vessels, there is no talk of diving or immersion in water.
Complications
Embolization of peripheral arteries leads to the formation of trophic ulcers and necrotic zones. Violation of venous outflow in the extremities leads to edema. Changes in the blood supply to internal organs make them weak or stop working altogether. Acute renal or liver failure, intestinal paresis, heart and pulmonary failure may occur. Damage to blood vessels in the brain can cause irreversible harm to the body. Paralysis, psychoemotional disorders and changes in the functioning of internal organs innervated by the damaged part of the brain are possible.
Prognosis and prevention
The result will be favorable if it is possible to remove air from a minimally traumatic subclavian access. With intracranial or pulmonary embolism, the prognosis is worse, since it is almost impossible to remove surgically. The use of HBOT and hypothermia does not quickly normalize blood flow, so the likelihood of irreversible consequences increases. Changes in peripheral veins and arteries are usually not life-threatening, but recovery of the affected tissues takes a long time, and complete recovery is not always achieved.
Most often, air embolization occurs during medical procedures, so preventing embolization is the sole responsibility of medical facility personnel. During procedures on the superior vena cava, the patient should be in the Trandelenburg position, catheterization of the subclavian vein, when the needle remains open at the end (disconnecting the syringe, removing the guide), is performed with deep exhalation. In case of low IOP, discontinued infusion systems should be promptly turned off.