Churg-Strauss syndrome
Also known as eosinophilic granulomatous vasculitis (angiitis), allergic angiitis and granulomatosis. This is a systemic vasculitis associated with allergic diathesis, most often affecting the lungs. Accompanied by asthma and eosinophilia. The pathology is close to periarteritis nodosa and Wegener's granulomatosis, but small vessels are more often affected, intra- and extravascular granulomas with a diameter of 1 mm develop, consisting of a central part with destroyed cells, altered collagen fibers and a peripheral part with macrophages, eosinophils and giant cells.
Symptoms
Asthmoid phenomena are noted - difficulty breathing and diffuse wheezing when inhaling. As the disease progresses, signs similar to those of periarteritis nodosa appear. Hemorrhages, papular-necrotic and ulcerative changes are detected on the skin. Arthralgia, abdominal pain, diarrhea, and hypertension develop. The main cause of death due to this pathology is heart disease due to cardiomyopathy.
Laboratory diagnostics
Eosinophilia, elevated IgE levels and, sometimes, rheumatoid factors are detected. When studying biopsy specimens, accumulations of eosinophils are observed in the extravascular space.
Treatment is symptomatic.
Behçet's disease
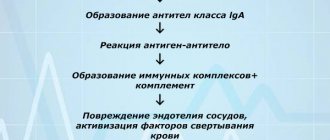
This is a chronic, relapsing systemic vasculitis, mainly affecting small and medium-sized arteries and veins, and is associated with HLA-B52. Autoantibodies to the epithelium of the mucous membranes appear, and immune complexes are formed. Lymphocytes infiltrate the walls of blood vessels and perivascular tissues. Swelling of the endothelium and narrowing of the lumen of blood vessels are noted.
Symptoms
Behçet's disease is accompanied by damage to the mucous membrane of the mouth (aphthae, stomatitis), the mucous membrane of the eyes (conjunctivitis), and the choroid of the eyes (uveitis). Recurrent ulcers of the external genitalia develop. Ulcers are sharply painful. The development of cutaneous vasculitis (erythema nodosum, papular rash, etc.) is possible.
Laboratory diagnostics
Autoantibodies to the epithelium of the oral mucosa and blood vessels are detected in the blood serum. The levels of certain classes of immunoglobulins, ESR and C-reactive protein levels increase.
Treatment
Colchicine, dapsone and non-steroidal anti-inflammatory drugs may be used.
Wegener's granulomatosis
The pathology is also known as malignant granuloma, a necrotizing granulomatous vasculitis of small vessels with damage to the respiratory tract, kidneys, skin and other organs and tissues
The mechanism of this rare disease is unknown. The development of pathology is promoted by microbial factors (herpes viruses, Staphylococcus aureus, etc.). Most patients with Wegener's granulomatosis have antibodies against proteinase-3 DR3) azurophilic granules of neutrophils, designated ANCA antineutrophil cytoplasmic antibodies). These antibodies are distributed diffusely in the cytoplasm of neutrophils. When cells are activated, this enzyme (PR3) is expressed on the membrane.
In addition, patients were found to have antibodies against other components of neutrophils, myeloperoxidase, elastase, lysozyme and lactoferrin. Antibodies against RRZ bound to neutrophils stimulate them to release activated oxygen radicals, hydrogen peroxide and enzymes that destroy the walls of blood vessels. These activated substances damage the glomerular basement membrane of the kidney. Cellular infiltrates, granulomas, hyalinosis and sclerosis of the vascular walls develop.
Symptoms (manifestations)
The clinical picture is characterized by common signs for different vasculitis. Sinusitis, rhinitis, inflammation of the middle ear, bronchitis, pneumonia, cavities in the lungs, damage to the organs of vision and kidneys (focal nephritis, necrotizing glomerulonephritis), erosion, infarction and necrosis of internal organs are noted. Ulcers of the oral mucosa occur. Weakness, night sweats and fever develop. Half of the patients are characterized by skin changes: palpable purpura, ulcerative necrotic lesions, granulomas. Muscle and joint pain appears. Body weight decreases. There is an alternation of exacerbations and remissions. An exacerbation occurs during the cold season of the year. Most patients die within 2 years.
Laboratory diagnostics
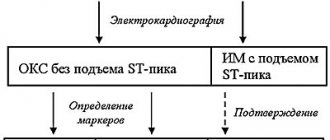
There is an acceleration of ESR and an increase in the content of C-reactive protein in the blood serum. Leukocytosis, thrombocytosis, and anemia develop. During a serological study, AKICA antibodies (cytoplasmic AKICA against RBZ) are detected in the blood serum.
Treatment
Treatment is the same for systemic vasculitis. Angioprotectors, corticosteroids and immunosuppressants (cyclophosphamide, etc.) are prescribed.
Treatment with folk remedies
If you visit any thematic forum, you can learn about many methods of treating vasculitis using traditional methods. But it is always important to remember that such treatment methods are only auxiliary in the process of main therapy. Before using them, it is better to consult a doctor about the advisability of such actions.
- If it is necessary to treat superficial vasculitis, herbal preparations are used that have a positive effect on the permeability of vascular walls and produce an anti-inflammatory effect. This effect is possessed by: Japanese sophora, buckwheat, water and bird knotweed, horsetail, and nettle.
- The use of decoctions and infusions of herbs that produce a general stimulating effect is also indicated: oat grains and straw, yarrow, rowan and black currant leaves, rose hips.
- The following will help reduce swelling in deep forms of vasculitis: string, stinging nettle, and cinquefoil erecta.
- In order to stimulate the function of the adrenal cortex, which is important in severe forms of vasculitis, treatment with drugs and decoctions containing ginseng, black elderberry, and eleutherococcus is recommended. Often patients are prescribed alcoholic infusions of ginseng and eleutherococcus.
- It is also recommended to drink green tea, which strengthens the walls of blood vessels and reduces their permeability, and also has a positive effect on metabolic processes in the body. It should be drunk every day, alternating with other herbal teas.
The following herbal remedies can be used:
- First collection. Knotweed, stinging nettle, sophora thick-fruited - 4 parts each, yarrow - 3 parts, black elderberry - 1 part. The infusion is prepared by pouring 5 g of the mixture with 1 cup of boiling water. Drink half a glass twice a day.
- Second collection. Black elderberry, horsetail - 3 parts each, peppermint - 2 parts. The infusion is prepared by pouring 5 g of the mixture with 1 cup of boiling water. Drink the infusion warm, half a glass 4 times a day. This infusion is also used for lotions. Applications are applied to the affected areas and kept for 15 minutes. This procedure can be carried out several times a day.
- The third gathering. is used as a general tonic and provides the body with vitamin K. To prepare it, St. John's wort, plantain, lungwort, black currant and rose hips are mixed in equal proportions. 10 g of product should be poured into 1 tbsp. water and boil for a few minutes. Drink half a glass 2 times a day.
Products for external use:
- Compresses made from pine resin. They are applied to the affected areas when applied to the skin. To prepare the product, 200 g of resin must be melted and added to it 40 g of unrefined vegetable oil, 50 g of beeswax. Mix everything, and when the mixture has cooled, apply it to the affected areas without removing it for 24 hours.
- Birch buds and nutria fat. To prepare the product you need to take 1 tbsp. grated dry or fresh birch buds and mix them with 500 g of nutria fat. Leave the product in a clay container for a week, keeping it on low heat in the oven for 3 hours every day. Place in jars and use every day as an ointment.
Micropolyangiitis
This is a necrotizing vasculitis, starting with inflammation of small vessels (microscopic polyarteritis). The average age of patients is 40 years. The pathology is associated with the formation of autoantibodies against the cytoplasmic components of neutrophils. The lungs, kidneys, intestines and skin are affected.
Symptoms and complaints
Severe weakness, fever, loss of body weight. With kidney damage, hematuria and proteinuria are noted, and with lung damage, cough with bloody sputum, dyspnea, and pleurisy. A purple rash and hemorrhages appear on the skin due to injury, and sometimes necrosis. If the gastrointestinal tract is affected - abdominal pain, diarrhea, intestinal bleeding. 1/4 of patients have keratoconjunctivitis and episcleritis.
Laboratory diagnostics
Anemia and neutrophilia, hyperglobulinemia, elevated ESR and C-reactive protein are detected.
Treatment
High-dose corticosteroids and cyclophosphamide are prescribed.
Takayasu arteritis
Also known as nonspecific aortoarteritis, or pulseless disease, is an obliterative vasculitis that affects the aorta and the vessels that arise from it.
Immune complexes are deposited in the walls of blood vessels. Inflammatory granulomas develop in the adventitia and outer layers of the middle lining of the vessels, including accumulations of lymphocytes, monocytes and, partially, neutrophils, giant cells, etc. Granulomas become fibrotic. Thrombosis occurs, sclerosis of the middle membrane, proliferation of the intima and, as a result, narrowing of the lumen of blood vessels.
Symptoms
Mostly young women suffer. The pathological process involves the thoracic aorta and its branches. The vessels of the neck and upper extremities are often affected. An aneurysm and thrombosis are formed. Vascular stenosis causes lameness, decreased or absent pulse, hypertension (frequent damage to the renal artery), and a discrepancy in blood pressure between the right and left arms. Fever, myalgia, arthralgia, headache and ophthalmological disorders may develop.
Laboratory diagnosis is not critical. There is an increase in ESR.
Treatment . Corticosteroids (prednisolone) are prescribed.
Giant cell (temporal or cranial) arteritis
Also known as cranial arteritis, Horton's disease is a systemic granulomatous vasculitis affecting mainly extra- and intracranial arteries in the elderly.
There are two types of giant cell arteritis, the pathogenesis of which remains unclear:
- giant cell (temporal) arteritis involving the large cranial arteries in the pathology;
- Takayasu arteritis with damage to the aorta and its branches.
In both types, massive thickening of the arterial walls or severe arterial stenosis occurs, and multinucleated giant cells are detected. Genetic predisposition (HLA-DR4) and the Cl4+ cell-mediated immune mechanism lead to the formation of granulomas, possibly with the participation of infections.
In normal medium-sized arteries, the resident population of dendritic cells is located exclusively in the adventitia and has a profile of immature cells. Immature dendritic cells are involved in maintaining immunological tolerance of T lymphocytes. Unlike mature dendritic cells, which induce a T cell response, immature dendritic cells do not express the co-stimulatory molecules CD80 and CD86. T lymphocytes that encounter antigen on immature dendritic cells receive an inhibitory signal.
With arteritis, dendritic cells are activated in the affected areas of the vessels and CD4+ T-lymphocytes that produce IFN-γ predominate. The latter activates macrophages and giant multinucleated cells. Macrophages produce inflammatory interleukins (IL-1, IL-b), metalloproteinases and reactive oxygen radicals. Infiltration of the vascular wall with mononuclear cells occurs, and giant multinucleated cells appear. The internal elastic layer of the vascular wall is destroyed. The lumen of the artery decreases. Fibrosis develops. In the intima and tunica media of medium-sized arteries, granulomas are formed, consisting of lymphocytes, plasma and epithelioid cells, histiocytes and giant cells.
Symptoms
The disease occurs in people over 50 years of age. The highest risk is age 75-85 years. The primary arteries involved are the head arteries (eg, temporal artery, retinal arteries, and cerebral arteries). Fatigue, fever, weight loss, dizziness, headache, hyperplasia, anorexia, and induration of the temporal artery develop. Due to damage to the retinal artery, sudden blindness develops. About 20-40% of patients with giant cell arteritis have concomitant symptoms of polymyalgia rheumatica: stiffness develops, bilateral symmetrical soreness of the muscles of the shoulder, pelvic girdle and proximal limbs appears.
Laboratory diagnostics . An increase in ESR of more than 50 mm/h, moderate anemia, and thrombocytosis are noted.
Treatment . Corticosteroids (prednisolone) are prescribed. In some cases, cytostatics are used - azathioprine or methotrexate.
Kawasaki disease
Kawasaki disease is a systemic arteritis of large, medium and small arteries, combined with mucocutaneous syndrome. More common in children than in adults. The arterial endothelium produces autoantibodies that bind to the Kawasaki antigen of endothelial cell membranes. Immune complexes are formed and immune inflammation develops.
Symptoms
Children aged 2-3 years are most often affected. The onset of the disease is acute - a 10-day high body temperature is accompanied by lymphadenopathy in the neck. Dry lips with redness and cracks, bilateral congestion of the conjunctiva, and conjunctivitis are noted. A red rash similar to hives appears on the skin, first on the palms and soles, then on the torso and limbs. Symptoms of systemic vasculitis and myocarditis appear after 2-4 weeks. Then, after 2 weeks, symptoms of fibrosis are added to the decreasing picture of vasculitis. Arthritis, arthralgia, uveitis, and photophobia develop. In subsequent years, aneurysms and blood clots form.
Causes
Until now, the causes of the development of this disease have not been studied enough. The causes of the manifestation of the primary form of the disease are determined only tentatively. It can develop due to viral and chronic infections, allergies , chronic autoimmune diseases, taking certain medications and contact with chemicals. The factors that provoke this disease are hypothermia, burns, radiation, trauma, and hereditary factors. However, these phenomena are not the causes of the disease, but its triggering factors.
Classification
According to the causes of occurrence, vasculitis is divided into 2 types:
- primary (independent disease);
- secondary (complication due to other diseases, medications, intoxications).
Depending on the size of the blood vessels where the pathology is observed, lesions are distinguished:
- small vessels (capillaries, arterioles, venules);
- middle vessels;
- large vessels (aorta, pulmonary artery);
- different types of vessels at the same time;
- a certain organ.
There are more than 25 types of vasculitis in the world, each of which differs in symptoms, treatments and prognosis.