Hemorrhagic vasculitis is also called allergic purpura, capillary toxicosis, or, after the names of the authors who described it, Henoch-Schönlein disease. The disease is part of a large group of vasculitis, inflammation of blood vessels of various types and sizes.
The peculiarity of the reaction of the vascular wall is aseptic conditions (absence of a pathogen) and the dominant role of a pronounced allergic reaction. The disease is accompanied by increased thrombus formation, impaired blood microcirculation in tissues and internal organs, which leads to damage to the kidneys, joints, and digestive organs.
The term hemorrhoidal vasculitis is erroneous. The doctor will not make such a diagnosis. The disease does not affect the venous network of the hemorrhoidal ring; there are other reasons for this.
Men under 20 years of age and children from 7 to 13 years of age are more susceptible to capillarotoxicosis. The incidence in these populations ranges from 14 to 24 per 10,000.
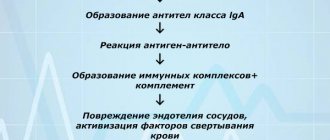
Mechanism of vascular damage
The main factor of damage in hemorrhagic vasculitis is special complexes formed from immune cells. They are called anaphylotoxins for their destructive properties. Under normal conditions they disintegrate. In a sick person, complexes accumulate and become antigens.
Deposition on the inner wall of blood vessels with a change in permeability causes blood circulation problems:
- platelets are activated;
- the plasma content of specific antithrombin decreases;
- the process of fibrinolysis is blocked.
As a result, a mass of microthrombi is formed in small vessels against the background of allergic inflammation and reduced blood clotting.
What kind of disease is this
This disease is of an infectious-allergic nature: the main cause of hemorrhagic vasculitis is the presence in the blood of patients of immune complexes and active components of the protective system of proteolytic enzymes. Immune complexes accumulate in the bloodstream, and with an excessive amount of antigens or a lack of antibodies, protein formations are deposited on the endothelium of the microvascular wall. Factors contributing to the development of the disease are:
- bacterial and viral respiratory infections suffered 2-4 weeks before the onset of the disease, which account for up to 60-80% of all cases of the disease;
- foci of chronic infection (sinusitis, tonsillitis, caries, etc.);
- some medications, mainly of antibiotic action;
- potentially allergenic foods (strawberries, citrus fruits, chocolate, eggs, etc.);
- administration of a vaccine or serum;
- hypothermia and dampness or prolonged exposure to the sun.
There is evidence of a hereditary predisposition to the disease. In some cases, it is impossible to find out which factor served as the “trigger” for the patient’s body.
Main reasons
The causes of the disease have not been precisely established. It is considered to be autoimmune. However, a connection with factors activating pathological processes has been identified. These include:
- transferred viral and bacterial infectious diseases, of particular importance is given to acute and chronic inflammation in the upper respiratory tract (influenza, ARVI, tonsillitis, sinusitis), measles, frequent sore throats, chicken pox, typhus, streptococcal diseases;
- traumatic damage to the skin and blood vessels;
- the influence of increased doses of solar radiation (with prolonged tanning), temperature fluctuations, radiation;
- allergic reactions to medications (usually antibiotics, sedatives and antihypertensive drugs);
- vaccinations during routine vaccination, prophylactic use of immunoglobulins;
- food allergies;
- household and professional poisoning, toxic infection;
- in children - helminthic infestations;
- reaction to insect bites;
- restructuring of the body during malignant and benign tumors;
- changes in women during pregnancy;
- metabolic disorders in endocrine diseases (diabetes mellitus);
- genetic predisposition in the family.
Hemorrhagic vasculitis in adults develops more often in old age, with weak and impaired immunity.
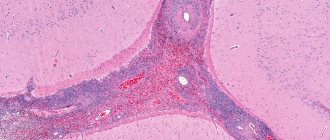
Thrombosis of the renal tissue leads to multiple infarctions, hemorrhages, and loss of organ function
About the development of the disease
Hemorrhagic vasculitis or Schenelein-Henoch disease is a disease in which autoimmune damage to small arteries occurs - they become fragile, their permeability increases, which causes impaired microcirculation, microthrombosis, multiple small hemorrhages (hemorrhages) as in the skin (hemorrhagic rashes on the skin and mucous membranes) , and in internal organs (gastrointestinal tract, kidneys, joints).
Most often the disease develops in childhood (6-7 years), but can also affect adults. Boys get sick 1.5 times more often than girls.
Clinical classification
Clinicians distinguish the following forms of the disease:
- simple or cutaneous - the whole process is limited to skin manifestations;
- skin-articular - in addition to the characteristic skin rashes, there are signs of inflammation of the joints;
- skin-abdominal - against the background of skin changes, symptoms of dysfunction of the stomach and intestines appear;
- renal - rare, accompanied by damage to the renal vessels with impaired filtration and urine excretion;
- mixed (combined) - there are changing symptoms of different forms.
Based on the type of disease, the following are distinguished:
- fulminant form - characterized by a rapid course, lasts several days, occurs in children under 5 years of age;
- acute - the disease has a sudden onset and lasts up to 30 days;
- subacute - lasts up to three months;
- protracted - clinical manifestations last for six months;
- recurrent - characterized by the repetition of symptoms at least four times in the next few years;
- chronic - the clinical picture of the disease lasts several years with periodic exacerbations.
Forecast
The prognosis is generally favorable and in 75% of cases patients recover within 1-2 years after the disease. In a number of patients with a chronic relapsing course, the disease can continue indefinitely with periodic relapses of one (skin) or several syndromes. The frequency of relapses throughout the entire period can vary from one to monthly, acquiring a monosyndromic character over time: mainly in the form of cutaneous purpura or a skin-articular form, less often - chronic nephritis in the form of a hematuric form with preservation of kidney function over a long period.
The prognosis is less unfavorable with the development of nephritis , especially when the process becomes chronic with manifestations of glomerulonephritis and transition to chronic renal failure. Purpura fulminans has a poor prognosis.
General and skin symptoms
Symptoms of hemorrhagic vasculitis usually appear suddenly without a prodromal stage. The clinic grows over several weeks. In most cases (especially in adults), a high temperature rises or a low-grade fever is maintained. Patients feel unwell, weak, and have a headache. These are the initial signs of intoxication. The diagnosis is still unclear, since many diseases occur this way.
A more typical sign is a variety of rashes on the body. It can appear on the back of the feet, buttocks, and legs. Less often on the stomach, arms, back. Usually symmetrical in nature.
For hemorrhagic vasculitis, skin manifestations on the face, neck, palms and soles of the feet are uncharacteristic. This sign is taken into account in differential diagnosis.
According to the description, the elements of the rash are different:
- bright red small blisters;
- papules that turn pale when pressed;
- possible location of red papules on the mucous membrane of the mouth and pharynx;
- purple nodules;
- minor bruises.
The diameter of small elements of the rash reaches 1 cm. They last up to four days, then turn pale and disappear. The next wave of skin manifestations should be expected after 7–10 days.
Initial manifestations most often appear as a small petechial rash, localized on the legs and tops of the feet.
Gradually the rash reaches the thighs and buttocks
Much less often the arms, back and stomach are involved in the process. At the same time, patients feel severe itching in the area of the rash, on the surface of the head covered with hair, around the eyes.
On examination, swelling of the lips, eyelids, and perineum is noted. The rash area is painful when touched. After the spots disappear, pigment spots remain, and during relapse they begin to peel.
Other symptoms
Among the symptoms of hemorrhagic vasculitis, it is important to highlight damage to internal organs and joints.
Classic signs of arthritis include:
- painful movements;
- swelling;
- redness.
Articular syndrome can develop simultaneously with skin rashes or appears gradually in 70% of patients, becoming more pronounced with each exacerbation. For adult patients it is more typical; in ¼ of patients it is preceded by skin rashes, and the pain is migrating in nature.
Depending on the intensity of pain, options are possible: from moderate discomfort during movements to severe inflammation with subsequent change in shape due to severe swelling. There are no joint deformities or persistent movement disorders. The pain lasts for several hours.
From the digestive organs the following are observed:
- short-term cramping abdominal pain (colic);
- nausea and vomiting;
- an admixture of blood in the stool due to bleeding of the intestinal mucosa.
In children, enlargement and tenderness of the inguinal lymph nodes are detected.
Abdominal syndrome is present in 23% of sick children. The pain is associated with swelling and rashes along the peritoneum. They usually do not cause serious bowel problems. They appear simultaneously with skin rashes or later, do not cause a significant deterioration in the patient’s condition, and are often identified during a targeted interview.
If the treatment of hemorrhagic vasculitis is delayed, then the adult patient experiences vomiting and diarrhea with blood as signs of gastric and intestinal bleeding.
Moderate, harmless bleeding occurs in half of patients. Cases of massive blood loss occur in 5%. Rarely, serious complications are possible:
- perforation of the wall with the development of peritonitis;
- intussusception.
During endoscopic examination, patients show signs of hemorrhagic or erosive gastritis, duodenitis, and less often - other localization in the intestine.
The elements are capable of merging and forming widespread areas of purple color
Anemic syndrome is caused by a decrease in the content of hemoglobin and red blood cells. It manifests itself:
- dizziness;
- weakness;
- noise in the head;
- fainting states;
- flashing “flies” before the eyes;
- tachycardia.
Kidney damage occurs in 10–60% of patients and causes:
- acute glomerulonephritis of autoimmune nature;
- there is an admixture of blood in the urine (red blood cells pass through the wall of inflamed arterioles).
Usually begins 1-3 weeks after the skin rash. The isolated form is rare.
If the respiratory tract and lobes of the lungs are affected, the patient experiences coughing and shortness of breath. The sputum may contain an admixture of blood due to increased bleeding of the capillary bed.
On the part of the cardiovascular system, pronounced tachycardia and a tendency to arrhythmias are noted.
Damage to the nervous system is considered an unfavorable consequence of the disease. They are caused by the transition of inflammation from blood vessels to the meninges. Therefore, they manifest themselves as symptoms of meningitis, encephalitis (severe headaches, loss of coordination, convulsions).
Prevention
The main measures to prevent hepatitis B in its relapses include:
- Adequate treatment of acute infectious diseases of the upper respiratory tract and timely sanitation of infectious chronic foci of ENT organs.
- Exclusion/minimization of contacts with allergens (if there is a history of allergic reactions) and control of medications.
- Preventing hypothermia of the body.
- Strengthening the immune system (hardening, rational nutrition).
- Dispensary observation of ill persons for 2 years.
How does the disease progress depending on the degree of activity?
To choose the correct therapy for hemorrhagic vasculitis, the doctor needs to know the degree of activity of inflammatory phenomena in the blood vessels. According to the clinic and the simplest laboratory tests, it is customary to distinguish 3 degrees:
- Grade I - the patient’s condition is satisfactory, the temperature is not elevated or slightly above 37, there are moderate non-widespread skin rashes, the ESR in the blood is not higher than 20 mm/hour, there are no other manifestations.
- Stage II - the patient’s condition is moderate, skin manifestations are intense, body temperature is over 38 degrees, there are signs of intoxication (muscle and headaches, weakness), there are clear signs of articular syndrome, abdominal and kidney symptoms are moderate. In the blood test: leukocytosis with eosinophilia and neutrophilia, ESR increases to 40 mm/hour, the ratio of protein fractions is disturbed towards a decrease in albumin.
- Degree III - the patient’s condition is objectively assessed as severe, there is a constant high temperature, intense symptoms of intoxication. The patient suffers from the simultaneous manifestation of skin, articular, renal and abdominal syndromes. Possible brain damage. Blood test: high leukocytosis due to neutrophils, ESR exceeds 40 mm/hour, possible decrease in red blood cells, hemoglobin and platelets (anemic syndrome).
The ankle and knee joints are most often affected, rarely the elbows and wrists.
Diagnosis of vasculitis
The earlier the examination is carried out, the diagnosis is established and treatment is started, the greater the chances of avoiding damage to vital organs and disruption of their functions.
If necessary, consultations with a vascular surgeon, therapist, ophthalmologist, neurologist, otolaryngologist, etc. are scheduled.
The diagnosis is made based on a number of data:
- physical examination;
- laboratory tests.
Tests for vasculitis (see also rheumatological examination)
The following tests are required:
- general blood test (usually an increase in ESR is noticed);
- biochemical blood test (protein fractions, etc.);
- immunological tests (gamma globulin, C-reactive protein, rheumatoid factor, ANCA, etc.);
- blood for HBsAg if viral hepatitis is suspected.
In addition, instrumental methods such as:
- Doppler ultrasound;
- radiography;
- angiography (examination of blood vessels using X-ray contrast agents);
- CT scan.
1 General blood test
2 Doppler ultrasound
3 Plasmapheresis procedure
How does the lightning form proceed?
The basis of the pathology of the fulminant form is determined by a hyperergic reaction with the subsequent development of acute necrotic thrombosis and vasculitis.
The pathology most often affects children 1 to 2 years old and accompanies childhood infections (chickenpox, rubella, scarlet fever). It manifests itself as typical extensive areas of hemorrhages on the skin, necrosis, cyanotic large confluent spots on the hands, feet, buttocks, and face. Next, gangrene of the hands and feet, a state of shock, and coma develop.
You can learn more about the clinical manifestations of Henoch-Schönlein disease in children here.
Diagnostic signs
The international community of rheumatologists has established the main diagnostic signs (criteria) of Henoch-Schönlein disease, which form the basis for differential diagnosis with other vasculitis:
- purpura - rashes that rise above the surface, which can be felt on palpation, and are not associated with low platelet levels;
- patient age under 20 years;
- abdominal pain, especially after eating, signs of intestinal ischemia, bleeding;
- The result of the biopsy is granulocytes in the wall of small vessels (arterioles and venules).
It is believed that if a patient has 2 or more signs, the accuracy of the diagnosis is 87%.
List of sources
- Lyskina G. A. Systemic vasculitis. In the book: Pediatric rheumatology. Guide for doctors / Ed. A. A. Baranova, L. K. Bazhenova. M.: Medicine, 2002. pp. 221–270.
- Kulaga V.V., Romanenko I.M., Afonin S.L. Allergic diseases of the blood vessels of the skin. Lugansk: “Etalon-2”, 2006. 168 p.
- A practical guide to childhood diseases, edited by prof. Kokolina V.F. and prof. A.G. Rumyantsev, volume IV. Hematology/oncology of childhood (edited by Rumyantsev A.G. and E.V. Samochatova). Medical practice – M. Moscow 2004 Zinovieva G.A., Frolkova E.V. Hemorrhagic vasculitis. Clinic and treatment // ros. pediatrician, journal — 1998. -N12. P.24-26.
- Krivosheev O.G., Gulyaev CB, Semenovykh A.G. Modern principles of treatment of Henoch-Schönlein purpura // Doctor. 2007. No. 4. -P.54-55.
How is the treatment carried out?
Treatment of hemorrhagic vasculitis begins with the doctor’s recommendations on the regimen and diet.
In case of exacerbation, strict bed rest is necessary. It is advisable to hospitalize the patient in a hospital, since correction and selection of medications are necessary. They are often administered by drip and intramuscular injection.
Outside of exacerbations, patients should not be in the sun and physical activity should be limited.
The diet for hemorrhagic vasculitis should exclude foods that cause allergies and increase blood clotting.
Not recommended for use in food:
- coffee and cocoa;
- candies;
- citrus fruits;
- eggs;
- spicy seasonings, mayonnaise;
- red varieties of berries;
- fried and smoked meat and fish dishes.
Chocolate is considered a strong food allergen
With the development of abdominal syndrome, the patient is prescribed nutrition with intravenous administration of special solutions. Dietary dishes are prepared according to the principle of table No. 1 (exacerbation of peptic ulcer disease).
Typically, hemorrhagic vasculitis is treated and observed in a clinic by a rheumatologist. Medicines of different groups are used.
To prevent hypercoagulability, the following is prescribed:
- disaggregants (Curantil, Trental);
- Heparin (dose is calculated based on the patient’s weight);
- as an activator of the fibrinolysis process - nicotinic acid in injections.
To relieve inflammation, corticosteroids are used, possibly a combination of tablets and intramuscular injections.
To limit the autoimmune process, cytostatics (Azathioprine, Cyclophosphamide) are rarely used. They are prescribed only in severe cases, for example, with autoimmune glomerulonephritis.
The dosage is selected individually in each case. You cannot change or cancel it yourself.
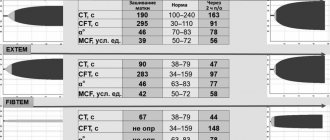
According to indications, plasmapheresis and transfusion of blood components are performed.
Diet
Hypoallergenic diet
- Efficacy: therapeutic effect after 21-40 days
- Timing: constantly
- Cost of products: 1300-1400 rubles. in Week
Diet Table No. 1
- Efficacy: therapeutic effect after 3 weeks
- Terms: 2 months or more
- Cost of products: 1500 - 1600 rubles. in Week
Diet 7 table
- Efficacy: therapeutic effect after a week
- Terms: 1 month or more
- Cost of products: 1200-1300 rubles per week
A hypoallergenic diet is prescribed, which involves excluding obligate allergens from the diet: milk, fish, citrus fruits, chocolate, cocoa, orange and red vegetables/fruits, as well as extractive substances. For abdominal syndrome, a modified Table No. 1 according to Pevzner is indicated until it is completely relieved. For nephritis - dietary Table No. 7 with a gradual transition to a hypochloride diet.