Hemorrhagic diathesis is a group of diseases characterized by an increased susceptibility of the body to bleeding, which can occur spontaneously or after minor trauma. These hematological syndromes develop when one or another link of hemostasis is disrupted. Common signs for all forms of pathology: increased bleeding syndrome and posthemorrhagic anemic syndrome.
Causes
The tendency to spontaneous or inadequate traumatic factor bleeding and hemorrhage can be hereditary (congenital or primary form) or acquired (secondary). Congenital hemorrhagic diathesis is caused by a defect or deficiency, as a rule, of one blood coagulation factor. Examples of such diseases are: Glanzmann's thrombosthenia, hemophilia, Randu-Osler disease, Stewart-Prower disease.
Secondary hematological syndromes occur when several hemostatic factors are insufficient. The causes of such violations may be:
- diseases (liver cirrhosis, SLE, infective endocarditis);
- hemorrhagic fevers (dengue fever, Ebola, Crimean, Marburg, Omsk);
- deficiency of vitamins (C, K, etc.);
- iatrogenic factors (long-term or inadequate dose therapy with thrombolytics and anticoagulants).
Pathogenesis
The cause of hemorrhagic diathesis is a violation of one of the stages of hemostasis - a physiological process that stops blood loss. Depending on which stage was violated, HD is divided into:
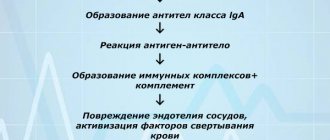
- Angiopathy (vasopathy). This includes diathesis caused by defects in the vascular walls. Normally, when damaged near the rupture site, the vessel contracts, then the properties of its walls change, they become sticky. This is necessary so that platelets can stick to them. This mechanism is disrupted in HD such as hemorrhagic vasculitis, Randu-Osler-Weber disease, as well as in the absence of vitamin C in the body.
- Thrombocytopathies, i.e. diseases associated with a defect in the platelet component of the coagulation system. Platelets may be produced in insufficient quantities or, as a result of changes in their functional properties, be destroyed too quickly. In both scenarios, platelet adhesion to the walls of blood vessels is difficult. This is typical for thrombocytopenic purpura, leukemia, thrombocytopenia, hemorrhagic aleukia, etc.
- Hemophilia (coagulopathy). In this group of diseases we are talking about a violation of the plasma component of hemostasis. That is, the stage when a successive cascade of reactions is launched in the blood, as a result of which the protein fibrinogen is converted into insoluble fibrin. This includes hemophilia, parahemophilia, disseminated intravascular coagulation syndrome, congenital afibrinogenemic purpura, etc.
The etiology of the hemostasis defects listed above may be different. There are congenital disorders associated with hereditary pathogenetic factors and acquired ones.
Hereditary ones appear in childhood. Parents usually bring a child to the pediatrician with symptoms.
Acquired ones are called symptomatic, because they are usually a manifestation or complication of some other disease: systemic lupus erythematosus, cirrhosis of the liver, etc. Their debut can only occur in old age.
Symptoms
The main symptom of hemorrhagic diathesis is bleeding, which can be:
- capillary (petechial-spotted rashes and bruises on the skin, hemorrhages in the mucous membranes, bleeding after tooth extraction, gingival, uterine, nosebleeds);
- hematoma (deep and painful soft tissue hematomas, hemarthrosis, hemorrhages in the subcutaneous fat and retroperitoneal tissue);
- capillary-hematoma (combines symptoms of petechial-spotted hemorrhages and soft tissue hematomas);
- microangiomatous (persistent recurrent bleeding of one or two localizations, often nasal, sometimes pulmonary or gastrointestinal, hematuria);
- vasculitic purpuric (small-point hemorrhages, with a symmetrical location on the limbs and torso).
Anemic syndrome with hemorrhagic diathesis is accompanied by the following symptoms:
- weakness;
- dizziness;
- pale skin;
- arterial hypotension;
- tachycardia;
- joint pain and swelling;
- nausea, cramping abdominal pain;
- lower back pain, dysuria, hematuria.
Prevention of diathesis in children
To achieve a sustainable result in the treatment of diathesis in children, doctors recommend reducing the exposure of the child’s body to allergens of all groups (not only food ones) as preventive measures.
For this it is proposed:
- refuse to keep pets;
- regularly carry out wet cleaning of the apartment;
- when choosing clothes for a baby, give preference to natural fabrics;
- reduce the number of soft toys as much as possible;
- use hypoallergenic skin and hair care products.
To prevent diathesis, other factors that provoke an allergic reaction and causes of pathology are also minimized.
Treatment of hemorrhagic diathesis
Therapy is based on a differentiated approach, taking into account the pathogenetic form of the disease. Treatment may include:
- measures to stop bleeding (application of a tourniquet, hemostatic sponge, cold heating pad, bandage, nasal tamponade);
- drug treatment (taking medications to improve blood clotting, increase the number of platelets, strengthen the walls of blood vessels);
- blood transfusion (erythrocytes, platelets, plasma);
- surgical intervention (elimination of a bleeding vessel, removal of the spleen, puncture of a joint to evacuate blood, drainage of soft tissues for hematomas);
- physiotherapy;
- therapeutic exercises.
If the problem is caused by an overdose of anticoagulants and thrombolytics, they are canceled or the dose is adjusted. Patients are prescribed vitamin K, aminocaproic acid, and undergo plasma transfusion.
In case of hereditary deficiency of blood coagulation factors, replacement therapy with their concentrations is carried out, fresh frozen plasma, red blood cells, and hemostatic therapy are used.
Treatment of autoimmune hemorrhagic diathesis involves the prescription of glucocorticoids, immunosuppressants, and plasmapheresis. If the effect of these measures is unstable, splenectomy (removal of the spleen) is performed.
In case of DIC, measures are taken to eliminate the cause of this condition, intravascular coagulation is stopped, hyperfibrinolysis is suppressed, and hemocomponent replacement therapy is carried out.
Clinical researches
The effectiveness, safety and tolerability of La-Cri products have been clinically proven. The products are recommended by the Union of Pediatricians of Russia; many products can be used in children from birth.
Sources:
- B.A. Shamov, I.G. Safiullina, A.B. Beshimova, T.B. Shamov, Differential diagnosis of atopic dermatitis, journal of Practical Medicine, 2011 https://cyberleninka.ru/article/v/differentsialnaya-diagnostika-atopicheskogo-dermatita
- Fokina R.A., Atopic dermatitis: stages of development of classification forms, Siberian Medical Journal, 2007 https://cyberleninka.ru/article/v/atopicheskiy-dermatit-etapy-razvitiya-klassifikatsionnyh-form
- A.N. Pampura, A.A. Chuslyaeva, Modern approaches to the treatment of atopic dermatitis in children https://cyberleninka.ru/article/v/sovremennye-podhody-k-terapii-atopicheskogo-dermatita-u-detey
Photos of diathesis
Photo album on the disease
Diagnostics
The examination is carried out to determine the etiological factors, the form of the disease and the prevalence of petechial-spotted rashes and bruises. The hematologist draws up a diagnostic plan together with a rheumatologist, traumatologist, infectious disease specialist, gynecologist, and surgeon.
The study includes:
- clinical and biochemical blood tests;
- stool occult blood test;
- Coombs test (determination of anti-erythrocyte antibodies);
- capillary fragility tests;
- determination of antiplatelet antibodies, lupus anticoagulant;
- sternal puncture of bone marrow, trepanobiopsy;
- radiography of joints;
- Ultrasound of the liver and kidneys.
Diet
Diathesis in children responds well to treatment if the recommended diet is followed.
During breastfeeding, the baby's mother should adhere to it. Allergenic foods (sweets, citrus fruits, eggs, honey, etc.) are excluded. During the introduction of complementary foods, in order to avoid the development of diathesis, the baby’s skin reactions to the new product should be monitored, and if signs of illness appear, exclude it for three to five months, until the next attempt. After the introduction of complementary foods, the basis of the menu should be cereals, lean meat and fish, vegetables and fruits. The consumption of sweets and foods high in food additives should be limited as much as possible. Contact us!
Specialists at the PsorMak Skin Diseases Center have been successfully treating diathesis in children for many years. Contact us for an initial consultation, our doctors will help you develop a complete understanding of how to properly treat the disease in the acute stage (with skin rashes). In addition, we will help you create a dietary diet and suggest what other measures to correct the child’s lifestyle should be taken to improve his health and effectively combat the disease. Make an appointment by calling +7 (495) 150-15-14,
Consequences
Complications of hemorrhagic diathesis do not occur in all patients. Their likelihood is determined by the nature of the pathology and concomitant diseases.
Among the consequences of such hematological syndromes are:
- iron deficiency in the body (leads to constant weakness and sleep disturbances);
- restrictions on joint mobility (due to hemarthrosis - accumulation of blood);
- paralysis (with extensive hematomas);
- infection with hepatitis, HIV (due to the need for frequent blood transfusions);
- loss of vision.
The danger comes from hemorrhages in the brain and adrenal glands, as well as profuse internal bleeding. With uncontrolled blood loss, the patient may fall into a coma.
Causes of diathesis in children
Diathesis in an infant on the cheeks or other parts of the body is not a specific disease, but a predisposition to the development of pathological reactions to irritants. This is considered a feature of the body that determines its reactivity. At the same time, against the background of diathesis, certain diseases may develop under the influence of unfavorable factors.
The causes of diathesis itself can be:
- unfavorable course of pregnancy;
- past infectious diseases during pregnancy;
- abuse of medications and bad habits during pregnancy;
- hypoxia or asphyxia of the fetus during childbirth;
- too little or too much birth weight;
- pathologies of the central nervous system;
- artificial feeding;
- dysbacteriosis;
- chronic diseases;
- insufficient or poor care;
- vaccination.
Hemorrhagic syndrome in newborns
Pathology of blood coagulation occurs not only in adults, but also in newborns, in whom the risk of its occurrence is somewhat higher due to the imperfection of hematopoiesis and many other organs and systems.
Children in the first days of life are characterized by increased vascular permeability, decreased coagulability and immaturity of the hemostatic system, however, these features are considered physiological and do not contribute to hemorrhagic syndrome.
If in the first hours and days of life a hemorrhagic syndrome appears and rapidly increases in a baby, then most likely it is associated with genetic disorders. Medicines that the pregnant woman took before giving birth (salicylates), hypoxia during pregnancy, and the state of prematurity can also predispose to increased bleeding during the neonatal period.
Often, signs of hemorrhagic syndrome are detected a week after the birth of the baby, when he has already been discharged home, so further observation and determination of the cause of hemostatic pathology lies in the area of responsibility of the pediatrician.
Classic symptoms of hemorrhagic diathesis in newborns include delayed healing of the umbilical ring with bleeding, nosebleeds, discharge of blood from the genital tract in girls, and the presence of blood in stool and urine. Severe forms of pathology occur with intracerebral and intraventricular hemorrhages, damage to the lungs and gastrointestinal tract.
HOW TO MAKE AN APPOINTMENT at the PsorMak Institute for Healthy Skin
1. Click the button you see below -
Make an appointment
2. Fill in the fields in the form that appears. Be sure to check the correct phone number so that our specialist can reach you. After filling out, click on the “Submit” button.
3. Wait for our specialist to call. He will answer any of your questions and agree on the date and time of your visit to PsorMak.
The initial appointment includes:
- Visual examination , which will allow the specialist to get a general understanding of the condition of your skin and the pathology itself.
- Collecting anamnesis - finding out information about the development of the disease, living conditions, previous diseases, operations, injuries, chronic pathologies, allergic reactions, heredity, etc. Together with a general examination, this allows you to make a fairly accurate diagnosis and choose a method of treatment and/or prevention.
Treatment methods for adults
When diathesis is detected in adults, treatment consists of:
- taking medications that alleviate the patient’s condition - antiallergic, immunostimulating, hormonal;
- avoiding interaction with allergens;
- compliance with nutritional rules and daily routine;
- using traditional medicine in accordance with doctor's recommendations.
Great importance is attached to normalizing the emotional background, eliminating stress, reducing anxiety, and avoiding negative emotions.
How to identify diathesis
The most common developmental anomaly of children in the first year of life is the exudative-catarrhal type of diathesis, the symptoms of which are well known to almost every mother. Among them:
- bright red spots on the cheeks, then on the arms, neck, legs, behind the ears;
- the appearance of small bubbles filled with liquid;
- weeping skin;
- severe itching and peeling.
Children drink a lot of fluids but produce relatively little urine because the fluid accumulates in the tissues. They often develop allergic rhinitis. After 2 years, skin manifestations are localized on the flexural surfaces and in the folds of the skin, acquiring the character of thickenings, papules, and pigmentation disorders.
In adolescents, starting from the age of 12, dry and flaking skin is observed, localized mainly on the face and upper torso. In adults, the skin most often affected is the arms and legs, forehead, neck and other parts of the body. Skin manifestations may be accompanied by conjunctivitis with redness of the eyes, photophobia, lacrimation and severe itching of the conjunctiva of the eyes.
Clinical diagnosis of diathesis depends on its type. As a rule, the patient is prescribed laboratory tests of blood and urine (general and biochemical), immunological tests are performed, and feces are examined to identify dysbacteriosis. To identify the lymphatic-hypoplastic form of the anomaly, an ultrasound scan of the thymus, liver, spleen and adrenal glands is performed, and the lymph nodes are examined.
Are you experiencing symptoms of diathesis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call