Difference between ECG and Holter monitoring
A conventional electrocardiograph (ECG) records and evaluates the work of the heart in a short period of time. An ECG reveals only persistent changes in the myocardium, which are not affected by general health, physical activity, or emotional background (stress, anxiety). Even if the day before a person had an attack of pain or heart rhythm disturbances, the cardiograph may not show any pathological changes.
With Holter monitoring, the electrical activity of the heart is recorded for 1–3 days, which makes it possible to see changes in the functioning of the heart while the patient is active, as well as during periods of rest and sleep. The Holter study is more informative and detects the slightest deviations from the norm that occur spontaneously and irregularly.
The latest models of the device are equipped with additional devices for recording daily blood pressure.
How to behave during monitoring
A few recommendations for monitoring:
- During the examination, the patient should lead a normal lifestyle without reducing physical activity to a minimum;
- The recorder and sensors on the body cannot be wet, that is, while wearing the device, it is necessary to completely avoid water procedures;
- Avoid mechanical and thermal damage to the halter;
- It is not advisable to travel, fly on an airplane or go on attractions during the examination;
- Typically, other electrical devices do not affect the operation of the Holter monitor, but it is still best to keep it away from microwave ovens, magnets, metal detectors, etc.
In addition, the patient must keep a special diary and record all actions performed during the day, indicating the time.
For example, the following actions should be noted in the diary:
- Time of administration and name of all medications taken during the day;
- Meal times, stressful situations;
- Time of going to bed, number of awakenings at night, time of getting up;
Climbing stairs is recommended as physical activity. For example, this can be done in your own entrance, going up to the 5th-10th floor. You need to indicate in your diary the start time of the climb and the end time. If you feel any discomfort while wearing the halter, this should also be noted in the diary.
List of indications for a Holter study:
- The absence of pathological changes on a traditional ECG when the patient complains of burning chest pain, shortness of breath, that is, symptoms indicating cardiac ischemia.
- Symptoms indicating arrhythmia: dizziness, fainting, rapid heartbeat, interruptions in heart function.
- Analysis of the effectiveness of treatment of coronary heart disease and arrhythmias.
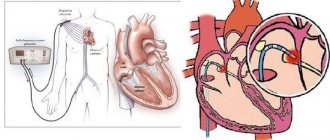
- Monitoring the functions of the pacemaker.
- Dynamic monitoring of people at risk for arrhythmias and coronary heart disease.
- Arterial hypertension in combination with cardiovascular failure.
- Preparation for surgery in people with myocardial pathology.
Important! Holter monitoring to assess the condition of the heart muscle is recommended for persons who have undergone chemotherapy or radiotherapy for cancer.
Introduction
Dear Colleagues!
The manual has a purely practical orientation, so you will not find here extensive discussions about the nature of the electrical axis of the heart and other phenomena. I invite those who want to gnaw on the theory to the pages of numerous books about ECG; there are plenty of them freely available on the Internet.
The manual is illustrative. The main thing in the presentation of each item in the table of contents is the corresponding picture, to which is attached the minimum possible description. On this site, small pictures are enlarged and moved using the left mouse button! Give it a try. (By the way, this picture shows an ECG machine. Would you like to work on one?)
In the conditions of market medicine, the ECG is forced to take its place among other, more informative methods, so here you will not find “shamanism” like “ECG for alcoholic heart disease.” I will describe only those facts about the ECG that I am 100% sure of.
The mass of electrocardiographic signs is “probabilistic” in nature and is not 100% proof of pathology (including elementary hypertrophy of the LV myocardium). Therefore, a cardiologist who has an ultrasound scanner with a cardiac sensor in his office will not “shamanize” the ECG regarding the P-mitral, but will simply look at the mitral valve with his eye and measure the blood flow on it using EchoCG.
Very often, ECG pathology is not detected during a 20-second recording of a standard resting ECG, but manifests itself only during a 24-hour recording (Holter ECG monitoring). Therefore, in this manual, most of the illustrations are taken from Holter recordings.
I was lucky enough to work with 12-channel Holter monitors, which are essentially a full-fledged ECG device with the ability to record 24 hours, so the concepts of “ECG” and “HM (Holter monitoring)” are very close to me, hence the name of the course.
Kinds
The following types of Holter monitoring have been developed:
- Full-scale monitoring , in which the procedure lasts 1-3 days. The device transmits the received data to a specialist for the purpose of quickly deciphering the results.
- Fragmentary method , when recording is made only at moments when a person feels pain or feels symptoms of arrhythmia. If health deteriorates, the patient himself presses the start button of the device.
ECG waves and waves
I suggest sticking to a simple rule: the teeth are sharp and the waves are smooth. What kind of waves and waves can be detected on an ECG?
As you can see, there are only eight of them (I do not count the possible splitting R).
The P wave reflects atrial contraction.
The delta wave is not normally observed and is pathognomonic for WPW.
QRST - waves of the ventricular complex, are very variable. R can split into 2 teeth, for example, with blockade of the right bundle branch in V1-V2.
The epsilon wave is commonly seen in arrhythmogenic right ventricular cardiomyopathy.
The U wave is an intermittent manifestation of ventricular repolarization, most often detected in V5.
Preparation stages and features
The procedure does not require special preparation.
To obtain reliable research results, the patient must be informed about the features of the procedure and the rules that he needs to follow.
The recorder is a complex electronic device, therefore it is unacceptable for it to be exposed to the following factors: water, electric, magnetic fields, low and high temperatures, which may adversely affect its operation.
The patient must ensure the correct placement of the electrodes, and if they become detached from the skin, put them back in place.
It is mandatory to keep a diary, which records periods of a person’s physical and emotional activity, times of sleep, meals, medications, and indicates the nature and duration of complaints (chest pain, dizziness, shortness of breath).
The study has no contraindications, does not disrupt the patient’s usual lifestyle, and does not cause any unpleasant sensations or discomfort.
When is Holter prescribed?
In cardiology, there are a huge number of indications for which daily ECG monitoring can be prescribed. Moreover, a holter can be prescribed not only if there are any deviations, but also for preventive purposes.
A doctor may prescribe this study in the following cases:
- Sudden fainting, loss of consciousness for no apparent reason;
- Frequent dizziness;
- The pulse is too high, or, conversely, low;
- Complaints about heart failure;
- Evaluation of the effectiveness of antiarrhythmic therapy;
- Assessment of heart rhythm after installation of a pacemaker;
- Complaints of shortness of breath or chest pain;
- Idiopathic hypertrophic cardiomyopathy;
- The presence of various types of arrhythmia, including atrial fibrillation;
- Feeling of “missed heartbeats”;
- Suspicion of angina pectoris;
- Unsatisfactory electrocardiogram readings;
- Chronic heart failure;
- Preventive examination of athletes, endurance testing;
- Determining the degree of compliance of a person’s physical capabilities with the requirements of the profession
Holter monitoring has no contraindications, except for acute inflammatory processes on the skin in the chest area (where the sensors are attached). The Holter test method can be performed on people of all ages, including pregnant women. There are no restrictions on the number of studies or intervals between them. In order to monitor the progress of treatment, the study is carried out repeatedly.
Decoding the results
The received data is processed by a computer program - a decoder. After studying the results, the doctor gives a conclusion that includes information about the heart rate, the presence of extrasystoles and arrhythmias, changes in the blood supply to the myocardium, the reaction of the heart muscle to stress and other parameters. All identified pathologies are confirmed by ECG printouts for the monitoring period.
If you are worried about dizziness, aching pain in the heart, shortness of breath of unknown origin, contact a cardiologist at the Caring Doctor clinic, who will prescribe a heart study using Holter monitoring. This modern technique will allow the doctor to detect heart disease in the early stages, prescribe the correct treatment and prevent serious complications such as heart attacks and strokes.
What the study will show
After the holter is removed, the doctor deciphers the data using a computer program. A graph is created on the monitor with cardio indicators, which are studied by a specialist. Typically, a 24-hour ECG provides a comprehensive report of cardiac activity. Typically the decryption procedure takes about 2 hours. You can wait for the results or get them the next day.
Using Holter monitoring, you can record various heart rhythm disturbances, tachycardia, arrhythmia, extrasystoles, etc. Please note that the conclusion of a Holter study is not an official diagnosis. To make a diagnosis, you will need to consult your doctor, and possibly additional diagnostic methods.
You can obtain more detailed information about a 24-hour Holter study during an in-person consultation with a doctor. Be healthy!
How is monitoring carried out?
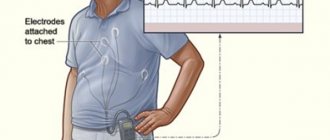
Recording an ECG using the Holter method is not difficult. Before starting the study, the cardiologist conducts an external examination of the patient. Then the sensors of a compact portable recorder are attached to his chest, after which they are fixed with an adhesive plaster. Nowadays, such a device is available in two types:
- three-channel models;
- twelve-channel models.
If the patient has had cases of allergic reactions, the doctor conducting the study should be warned about this, since sometimes an allergy to the patch with which the electrodes is attached is possible.
The fixing device itself is located on the patient’s belt. You need to wear it without taking it off throughout the day - this is the only way to get objective, accurate information about the state of the cardiovascular system. During monitoring, you should adhere to the following rules:
- do not take a shower or bath;
- do not get close to power lines;
- protect the device from overheating or mechanical damage;
- slightly limit physical activity so as not to cause excessive sweating;
- keep a diary of self-monitoring of blood pressure fluctuations.
In some cases, patients ask themselves: is it sometimes possible to fool the device? The doctors answer is unequivocal - no, this is impossible.
Ankle-brachial pressure index - ABI
The ankle-brachial index is a parameter that allows you to assess the adequacy of blood circulation in the lower extremities.
For this purpose, blood pressure is measured in the shoulder and ankle area. After this, these indicators are compared, as a result of which the doctor receives the ankle-brachial index. Typically, the pressure in the shoulder and ankle areas is the same. However, if the pressure in the ankle area is lower than in the shoulder area, this means that the arteries in the lower extremities may be narrowed. To determine the ankle-brachial index, the doctor uses a conventional blood pressure measuring device or an ultrasound machine. However, this parameter does not allow determining the location of arterial blockage. The ankle-brachial pressure index reflects the degree of stenosis or occlusion of the arteries of the lower extremities due to atherosclerotic obliteration. ABI <0.9 in both legs is considered positive for the diagnosis of peripheral atherosclerosis.
Methods for diagnosing transient myocardial ischemia in patients with coronary artery disease
N.V. Shestakova
Department of Cardiology, Russian Medical Academy of Postgraduate Education, Moscow
V.A.Shestakov
Department of Propaedeutics of Internal Diseases, Moscow Medical Dental Institute
Early and timely diagnosis of coronary heart disease (CHD) is an important clinical, social and economic problem. According to American statistics, direct and indirect costs for this group of patients amount to $14 billion per year. Early detection of ischemia, as well as its detection in patients with asymptomatic, latent ischemic heart disease, can bring tangible benefits to the patient [1]. It is well known that in a fairly significant number of patients suffering from coronary artery disease, even with an in-depth survey, its specific subjective signs (angina attacks) cannot be identified or they are of an atypical nature. Detection of transient ischemia is also important in patients with documented ischemic heart disease.
To diagnose myocardial ischemia, various methods can be used: ECG recording at rest, Holter ECG monitoring, various stress tests (treadmill test and bicycle ergometry - VEM), pharmacological tests, stress echocardiography, radioisotope methods.
The choice of method for detecting myocardial ischemia should be determined primarily by the clinical picture and specific tasks facing the doctor [2]. In addition, it is necessary to take into account the features of each specific method: indications and contraindications for its use, advantages and disadvantages, limitations in use, depending both on the characteristics of the method itself and on the patient’s condition, the method’s capabilities in assessing the nature and severity of coronary and myocardial damage , its prognostic capabilities [1,2].
It is very important to consider the cost of the study, as well as whether, in each particular case, a more expensive study is more adequate and informative [2]. The objective value of each test is determined by its sensitivity and specificity.
Sensitivity is the percentage of true positives in the presence of CAD; specificity is the percentage of true negative results in the absence of CAD. The sensitivity and specificity of any test can vary significantly.
The resting ECG is normal in about half of patients with stable angina. Nonspecific changes in the terminal part of the ventricular complex (ST segment and T wave), according to the Framingham study, are quite common in the general population (8.5% of men and 7.7% of women).
The causes of false-positive results may be hypertrophy and dilatation of the left ventricle, electrolyte disturbances, cardiac arrhythmias and conduction disturbances, taking antiarrhythmic drugs, hyperventilation, etc. Transient ischemic changes in ST - T during an attack of angina in patients with documented ischemic heart disease are of greater importance. However, the sensitivity and specificity of this method in diagnosing transient myocardial ischemia is low.
Holter ECG monitoring is used along with stress tests to detect transient myocardial ischemia. The value of this technique lies in the ability to detect transient myocardial ischemia in everyday life. The criterion for myocardial ischemia during Holter ECG monitoring is ischemic-type ST segment depression of 1 mm or more with a duration of ST segment depression of at least 1 minute and time between individual episodes of at least 1 minute. This is the so-called “1x1x1” rule [1]. The method is particularly useful for identifying episodes of vasospastic or spontaneous ischemia, as well as asymptomatic myocardial ischemia. Asymptomatic myocardial ischemia is often a poor prognostic sign. Considering that Holter ECG monitoring often gives false-positive results in patients without angina, it is recommended to use this method as a screening method in patients with a large number of risk factors for coronary heart disease or with a family predisposition to coronary artery disease [1], as well as for assessing individual prognosis.
Due to the fact that the ability to detect transient myocardial ischemia by recording an ECG at rest is very limited, stress tests become much more important.
Load tests
Stress tests provoke myocardial ischemia by increasing myocardial oxygen demand (treadmill test, VEM, dobutamine test) or reducing oxygen delivery to the myocardium (tests with dipyridamole and adenosine). Load testing in the form of a treadmill test or VEM is still the most common research method. This is a relatively simple and inexpensive method for detecting transient myocardial ischemia in patients with suspected or established coronary heart disease [1,3].
The treadmill test has both advantages and disadvantages compared to VEM. The advantage lies primarily in the fact that the load is more physiological and is perceived by patients as more familiar. In addition, when using the standard Bruce protocol, it is possible to perform a greater load than with VEM and more quickly achieve the desired result [4]. The treadmill test is often used in the USA and relatively rarely in Europe and Russia. Possible reasons for this are the higher cost of the treadmill, which is 2–4 times more expensive than a bicycle ergometer, and its large dimensions.
Load on a bicycle ergometer. In case of positive results of the VEM test, the likelihood of a diagnosis of IHD increases. The higher the initial probability of coronary heart disease, the higher the value of this stress test for the patient’s ability to perform adequate physical activity. The most reliable sign of transient myocardial ischemia with a VEM test is horizontal or oblique ST segment depression of 1 mm or more. The probability of diagnosing coronary artery disease is close to 90% if, during exercise, ST segment depression of the ischemic type reaches 2 mm or more and is accompanied by a typical attack of angina pectoris [1]. In patients with an initially high probability of coronary artery disease, detection of myocardial ischemia is more important for assessing the severity of coronary lesions and prognosis.
A positive result of the VEM test in such patients is combined with a significantly higher risk of coronary complications and death (the latter by 3.5-6 times) [5]. When the ST segment rises to 1 mm at the third stage of load according to the Bruce protocol, mortality in the group of such patients is less than 1% per year, and when the ST segment rises by more than 1 mm at the first stage of load it exceeds 5% per year.
The criteria for a high risk of coronary complications when performing a VEM test include:
•depression of the ST segment by 2 mm or more;
•early appearance (at the first stage of load) of ST segment depression of 1 mm or more;
•ST segment depression in several leads;
•reduced tolerance to physical activity;
•ST segment elevation in leads where there is no pathological Q wave;
•long-term persistence of depression or elevation of the ST segment after cessation of exercise (more than 8 minutes);
• low maximum heart rate (HR) during exercise, no more than 120 per minute;
•the appearance of life-threatening ventricular arrhythmias;
•decrease in blood pressure or absence of its increase during exercise.
Due to the relatively low sensitivity of the VEM test for ischemic heart disease, its negative result does not exclude this diagnosis. The rate of false positive results reaches 15%. Numerous studies have reported lower sensitivity of VEM and higher false-positive rates in women compared to men [6]. However, when men and women are stratified according to the prevalence of CAD, the study results are similar [7]. The sensitivity and specificity of the treadmill test and the VEM test are approximately the same. Exercising on a bicycle ergometer poses obvious difficulties for patients who do not have cycling experience. The advantages of VEM include the ability to perform a load both sitting and lying down, which is sometimes necessary according to the research protocol when solving some specific problems. Exercise on a bicycle ergometer and treadmill is an accessible and common test, but from 20 to 40% of patients cannot perform them if necessary due to orthopedic and neurological disorders or vascular diseases of the extremities [3].
Stress echocardiography is a new method widely used in the diagnosis of coronary artery disease. A treadmill or bicycle ergometer, as well as pharmacological drugs, are used as a load. Stress echocardiography using a treadmill or bicycle ergometer competes with radioisotope methods in accuracy and equivalence. This technique should be used if the ECG is initially altered (signs of left ventricular myocardial hypertrophy, intraventricular conduction disturbances, electrolyte disturbances, drug effects, etc.). In these cases, local contractility disorders that occur during the development of myocardial ischemia can be detected using echocardiography [4]. The normal response of the left ventricle to exercise is an increase in the rate of contraction and systolic thickening of the left ventricular myocardium. When ischemia occurs, these indicators can change to varying degrees.
The criteria for a strongly positive test are:
•reduction of ejection fraction to 35% or less;
• increase in ejection fraction at load by less than 5%;
•the appearance of disturbances in local contractility of the left ventricle at a low level of load or at a heart rate of less than 120 per minute;
•the appearance of contractility disorders in several segments of the left ventricle.
The advantages of this test over radioisotope methods: low cost and safety, availability of portable equipment, lack of radiation, quick results, the ability to identify other causes of patient complaints (pain and other sensations in the chest, shortness of breath, weakness). Limitations of the method: the need for a good ultrasound window, difficulties in assessing the basal segments with maximum dyskinesia under heavy load. A significant drawback is that echocardiography is performed immediately after the end, and not at the height of the load; if dyskinesia is detected after the load, it is unclear at what stage of the load it began. In addition, a well-trained ultrasound specialist is required to conduct the study. The sensitivity and specificity of this test have been evaluated in a large number of studies. According to one multicenter study (1150 patients), sensitivity ranged from 74 to 97%, and specificity from 64 to 100% [4]. In a study by R. Cohn et al. (1987, 390 patients) sensitivity averaged 80% and specificity 91%.
Pharmacological stress echocardiography is performed to provoke and identify myocardial ischemia, as well as to determine the functional state of the myocardium and prognosis in a patient with coronary artery disease.
Indications for stress echocardiography are [8]:
• inability to perform a treadmill test or exercise on a bicycle ergometer;
•lack of ability to perform physical activity to the required capacity;
•false-positive results of the exercise test in patients without symptoms of coronary artery disease.
The most commonly used drugs in this test are dobutamine, dipyridamole, adenosine and arbutamine.
Dobutamine is a synthetic catecholamine that predominantly stimulates b-adrenergic receptors, giving a strongly pronounced positive inotropic and to a small extent chronotropic effect. Blood pressure does not change significantly. An increase in myocardial oxygen demand provokes ischemia with significant narrowing of the coronary arteries. The resulting disturbance of local myocardial contractility is detected using echocardiography.
Administration of dobutamine is contraindicated in valvular stenosis, idiopathic hypertrophic obstructive cardiomyopathy, ventricular tachyarrhythmias, and severe arterial hypertension (AH) [3]. The number of side effects is relatively small, but in 10–36% of patients, arrhythmias appear during the test [11].
Dipyridamole, a coronary vasodilator, dilates unchanged coronary arteries to a greater extent, resulting in the development of the phenomenon of intercoronary steal, i.e. the resulting myocardial ischemia is the result of decreased oxygen delivery to the myocardium. The administration of dipyridamole is safe, side effects are rare and are observed in 1 - 2% of cases [3]. Contraindications for the administration of dipyridamole are obstructive pulmonary diseases, severe intraventricular conduction disorders, and severe hypertension.
Adenosine, like dipyridamole, dilates non-stenotic coronary arteries and increases the perfusion of the segments they supply. This leads to pronounced heterogeneity of the blood supply to the myocardium and provokes ischemia. The vasodilating effect appears quickly and disappears quickly. Despite the fact that the administration of adenosine is safe, various adverse reactions often occur (hot flashes, shortness of breath, headache, dizziness, parasthesia), which are subjectively difficult to tolerate by patients.
Arbutamine is a new non-selective β-adrenergic receptor agonist with moderate α1-sympathomimetic activity, developed specifically for stress testing and is well tolerated [3]. Like other beta-agonists, which increase myocardial oxygen demand, it increases heart rate and myocardial contractility. To administer arbutamine, a special system (GenESA) is required that automatically adjusts the dose of the drug based on heart rate.
The system provides constant monitoring of heart rate, blood pressure, heart rhythm, ECG and ECG signs of myocardial ischemia, and conducts their computer analysis.
Dobutamine stress echocardiography. Numerous studies [2] have reported high sensitivity and specificity of this test. In comparison with the results of coronary angiography when dobutamine was administered at a dose of 40 mcg/kg per minute, the sensitivity of the test ranged from 72 to 86%, specificity from 77 to 95%, and accuracy from 76 to 89%. It is noted that reducing the dose of dobutamine was accompanied by a decrease in the accuracy of the study. Many studies indicate that the sensitivity of dobutamine stress echocardiography is higher for multivessel disease than for single-vessel disease, and for stenosis of 70% or more than for vessel stenosis of 50% or less. However, there are other data [7]. A meta-analysis of 7 published studies using high-dose dobutamine in 703 patients shows that dobutamine stress echocardiography has a higher sensitivity (75% versus 63%) in single-vessel disease. In patients with angiographically unchanged coronary arteries, dipyridamole stress echocardiography is characterized by higher sensitivity in combination with high specificity (91 and 83%, respectively). The sensitivity of these two tests for multivessel disease is approximately the same, being 79% with dipyridamole and 81% with dobutamine.
Adding atropine to dobutamine increases the sensitivity of this test. Sensitivity in detecting transient ischemia in patients who have had myocardial infarction is lower. Dobutamine stress echocardiography is used in patients after coronary artery bypass grafting to identify the functional state of the shunt; its sensitivity is 80% and specificity is 90%. A direct comparison of dobutamine stress echocardiography and stress echocardiography with vasodilators in the same patients showed that the test is more sensitive when using dobutamine, dipyridamole (78 and 67%) and adenosine (82 and 52%).
Dipyridamole stress echocardiography is the easiest to interpret among other pharmacological tests. Its accuracy is comparable to that of dobutamine stress echocardiography. Safety and prognostic value have been demonstrated in large multicenter studies [8]. S. Severi et al. (1994) note that the sensitivity of dipyridamole stress echocardiography is higher in multivessel lesions, in patients with well-developed collaterals and in patients with reduced regional myocardial perfusion. The sensitivity of this test, according to R. Mazeika et al. (1992), varies widely: from 0% with single-vessel disease to 100% when using the transesophageal technique, even with single-vessel disease. According to S. Beckmann et al. [4], it averages 57 - 75%. Specificity ranges from 80 to 100%. For multivessel disease, sensitivity reaches 79%.
Adenosine stress echocardiography. The sensitivity of this test averages 40 - 85% and is quite variable in patients who have not had myocardial infarction, and low in patients with single-vessel disease. The specificity of adenosine stress echocardiography ranges from 87 to 100%. The relatively low sensitivity of this test and the frequent occurrence of adverse reactions that are poorly tolerated by patients, although not dangerous, prevent the widespread use of this test.
Arbutamine stress echocardiography is a fairly accurate and safe method for detecting myocardial ischemia, diagnosing coronary heart disease and determining the prognosis in these patients. The results of a multicenter study that assessed the clinical suitability and safety of arbutamine showed that the sensitivity of the test in detecting myocardial ischemia reaches 71%, and in diagnosing coronary artery disease - 82%; the specificity is 100 and 50%, respectively. In a study by Cohen et al., performed in 143 patients, the sensitivity of this test in provoking myocardial ischemia is 76%, in diagnosing coronary artery disease - 84%, and its specificity reaches 96% [9].
In addition, some studies have demonstrated that arbutamine is potentially better in its pharmacological properties, effect on hemodynamics and tolerability than dobutamine, dipyridamole and adenosine [7]. However, the cost of the system used to administer it and evaluate the results is significantly higher than that of other pharmacological stress tests. However, in some European countries this new method is highly valued and is practically the only officially accepted stress echocardiogram test.
Radionuclide stress tests. Myocardial perfusion scintigraphy with thallium-201 or technetium-99m makes it possible to detect defects in their accumulation in the myocardium. The capabilities of the method increase significantly when perfusion scintigraphy is combined with physical or pharmacological stress. The need for this study arises if the patient cannot perform an exercise test, the test has not been brought to diagnostic criteria or its results are questionable, stress echocardiography cannot be performed or its conduct does not give the desired result (for example, poor visualization of the lateral wall of the left ventricle during EchoCG). When comparing perfusion scintigraphy with thallium-201 or technetium-99m with stress echocardiography, one should first of all note the high cost of the study, primarily due to the need for a special laboratory and expensive equipment [3]. Poldermans et al. (1993) provide data on the comparative cost of dipyridamole-thallium-201 perfusion scintigraphy and dobutamine stress echocardiography: 530 and 185 US dollars, respectively. In addition, the study involves radiation and a lot of time. False-positive results reduce the diagnostic value of the method. Their most common causes are: obesity, leading to poor image quality; large mammary glands and a high diaphragm, which contribute to the appearance of overlay artifacts. In addition, perfusion scintigraphy visualizes the posterior wall of the left ventricle worse. But the method also has undoubted advantages: automation of the process, the ability to quantify the results obtained and determine the location of the lesion. When combining myocardial perfusion scintigraphy with thallium-201 and exercise on a bicycle ergometer or treadmill, the appearance of an accumulation defect during exercise indicates the presence of transient myocardial ischemia. The combination of myocardial perfusion scintigraphy with a pharmacological load (dipyridamole or adenosine) leads to pronounced inhomogeneity of thallium absorption and its subsequent redistribution, which is also a sign of transient myocardial ischemia.
In both cases, the criteria for a sharply positive test associated with a high risk of complications are:
•the appearance of accumulation defects against the background of low load or at a heart rate of less than 120 per minute;
•multiple accumulation defects;
•increased accumulation of thallium in the myocardium.
Comparative data on the diagnostic value of stress echocardiography and myocardial perfusion stress scintigraphy with thallium-201 or technetium-99m, based on the results of seven independent studies (390 patients), in which a treadmill test or VEM test was used to provoke myocardial ischemia, show that that the sensitivity of stress tests averaged 80 and 84%, respectively. At the same time, the sensitivity of stress perfusion scintigraphy was higher in single-vessel lesions (80 versus 69%), but the specificity was higher when performing stress echocardiography (91 and 83%, respectively) [2].
Dobutamine stress echocardiography and dobutamine perfusion scintigraphy were compared in four studies in 318 patients. The sensitivity of these methods in detecting myocardial ischemia was comparable (76 and 81%). At the same time, a higher sensitivity of both methods was revealed for single-vessel lesions (83 and 85%) than for multi-vessel lesions (68 and 76%). The specificity of dobutamine echocardiography (85%) was higher than that of stress perfusion scintigraphy (71%) [2].
Stress echocardiography and myocardial perfusion scintigraphy with vasodilators (dipyridamole or adenosine) were compared in five studies in 222 patients. Myocardial perfusion scintigraphy has been shown to be superior in results to stress echocardiography. Its sensitivity is higher than the sensitivity of stress echocardiography and is 90 and 66%, respectively, and specificity is 79 and 91%. The results of the comparative assessment are shown in the table. T. Marwick et al. (1993) reported that the sensitivity of these tests depends on the severity of coronary lesions. According to their data, the sensitivity of perfusion scintigraphy with vasodilators in single-vessel lesions is higher (81%) than the sensitivity of echocardiography with vasodilators (52%). Sensitivity for multi-vessel lesions increases and is 93 and 64%, respectively.
Only two studies (T. Marwick et al., 1993; M. Takeuchi et al., 1993) compare data from dobutamine stress echocardiography and myocardial perfusion scintigraphy with vasodilators. It was shown that both tests have approximately the same sensitivity (85 - 86 and 85 - 89%). However, the specificity of dobutamine stress echocardiography is higher (93 - 85 and 82 - 71%). Based on these results, the authors suggest that the use of dobutamine stress echocardiography will increase in the future.
Assessment of the severity of CAD using dobutamine stress echocardiography and dobutamine perfusion scintigraphy was carried out in two centers. Senior et al. (1997) revealed signs of multivessel disease in 70% of cases with stress echocardiography and in 77% with perfusion scintigraphy. The specificity of the results obtained was 90 and 94%, respectively. T. Marwick et al. (1993) examined patients who had suffered acute myocardial infarction. Signs of multivessel disease were detected using stress echocardiography in 18% of patients, and using myocardial perfusion stress scintigraphy - in 34% of patients. The capabilities of each test were compared with the results of coronary angiography. The results of stress echocardiography and perfusion scintigraphy correlated with angiography data (correlation coefficients 0.45 and 0.35, respectively). These data show that stress echocardiography and perfusion scintigraphy are quite accurate in recognizing multivessel disease. Based on the results obtained, the authors suggest performing dobutamine stress echocardiography in patients with suspected CAD or with documented CAD in the following cases:
• if it is impossible to perform the load;
•if there are contraindications to the use of vasodilators;
•if other studies pose an increased danger to the patient;
•if the degree of coronary stenosis is unclear;
• in the presence of concomitant left ventricular hypertrophy or left bundle branch block;
•to assess the effectiveness of antianginal therapy.
In all these cases, stress echocardiography is more specific than perfusion scintigraphy.
Thus, methods for diagnosing transient myocardial ischemia are numerous. When determining the objective value of a particular method, it is necessary to focus on its sensitivity and specificity. They differ for different methods. Equally important is taking into account the cost of the study. However, the low cost of the method should not be the determining argument when choosing it. Taking into account the specific features of the methods, including their diagnostic value, as well as based on practical expediency, the examination should begin with simpler methods (VEM, daily ECG monitoring). If they cannot be performed or do not solve the assigned tasks, stress echocardiography is necessary. And only if this study does not solve the problem, it is advisable to use stress perfusion scintigraphy of the myocardium with thallium-201 or technetium-99 m.
Literature:
1. Gottlieb SO. Diagnostic procedures for myocardial ischemia. Eur Heart J 1996;17(suppl G):53-8.
2. Geleijnse ML, Salustri A, Marwickt TH, et al. Should the diagnosis of coronary artery disease be based on the evalution of myocardial function or perfusion? Eur Heart J 1997;18(suppl D):68-7.
3. Elhendy A, Geleijnse ML, Roelandt JRTC, et al. Dobutamine without transient wall motion abnormalities: Less severe ischemia or less severe stress? J AM Coll Cardial 1996;27:323-9.
4. Beckmanns, Scharti M, Boksch W, et al. Diagnosis of coronary artery disease and viable myocardium by stress echocardiography. Diagnostic accuracy of different stress modalities. Eur Heart J 1995; 16 (suppl J): 10-8.
5. Scharte M, Beckmann S, Bocksch W, et al. Stress echocardiography in special groups: in women, in left bundle branch block, in hypertension and after heart transplantation. Eur Heart J 1997;18(suppl D):63-7.
6. Proceedings of an WHLBJ Conference: Exercise ECG testing with and without radionuclide studies. Jn Cardiovascular Health and Disease in women. Greenwich, CT, Le Jacg Communications, inc 1993: 74.
7. Picano E, Ostojic M, Sicari R et al. Dipyridamole stress echocardiography: state of the art 1996. Eur Heart J 1997;18 (suppl D):16-23.
8. Afridi J, Kleiman NS, Rainzer AE, et al. Dobutamine echocardiography in myocardial hibernation. Circulation 1995;91:663-70.
9. Ketteler T, Krahwinkel W, Wolfertz J, et al, Arbutamine stress echocardiography. Eur Heart J 1997;18(suppl D):24-30.
Published with permission from the administration of the Russian Medical Journal.