Hypercholesterolemia is a disease in which the level of cholesterol in the blood rises to pathological levels. From the point of view of normal physiology, this compound is important and useful. Normally, most of it is produced by the body (up to 80%). Cholesterol ensures the stability of cell membranes and is involved in the synthesis of vitamins, bile acids, and hormones. However, with hypercholesterolemia, its level increases, it is deposited on the walls of blood vessels, affects metabolic processes and leads to the development of serious complications, including heart attack, stroke, hypertension, etc.
What is the cause of hypercholesterolemia?
The most common cause of increased cholesterol levels is excess nutrition and a sedentary lifestyle. Modern man spends too few calories with a “full” diet. Hereditary predisposition plays a certain role.
In addition, hypercholesterolemia can be secondary and provoked by diseases such as:
- diabetes;
- decreased thyroid function (hypothyroidism);
- kidney damage in the form of nephrotic syndrome;
- liver dysfunction;
- genetic diseases (familial hypercholesterolemia).
Hypercholesterolemia can also occur while taking certain groups of pharmacological drugs.
These include:
- progestins;
- anabolic steroid;
- different types of immunosuppressants.
Risk factors for the development of hypercholesterolemia are:
- hereditary predisposition;
- excess body weight;
- low physical activity;
- chronic or acute stress.
Normally, cholesterol ensures the stability of cell membranes and participates in the synthesis of vitamins, bile acids, and hormones. If its level is high, especially for low-density lipoproteins, it is deposited in the walls of blood vessels, which entails an increased risk of developing severe cardiovascular accidents.
Why do lipid metabolism disorders occur?
The reasons that contribute to the development of hypercholesterolemia (a disorder of lipid metabolism in the human body, which leads to increased cholesterol levels in the blood) can be divided into primary and secondary. In the first case, we are talking about hereditary (family) forms.
Andrey Pristrom, Head of the Department of Cardiology and Rheumatology of BelMAPO, Doctor of Medical Sciences, Professor.Andrey Pristrom, Head of the Department of Cardiology and Rheumatology of BelMAPO, Doctor of Medical Sciences, Professor:
In the familial form of hypercholesterolemia, the metabolic processes of cholesterol synthesis are disrupted at the genetic level. Such forms are quite rare. However, they can lead to the development of cardiovascular accidents already at a young and even childhood age. There are often cases when the diagnosis of a hereditary form is established after one or another cardiovascular event has already occurred.
There are two forms of familial hypercholesterolemia: homozygous and heterozygous.
The homozygous form is rare but very severe. The prevalence rate is 1 case per 200-300 thousand people. With this form, the risk of developing some kind of vascular accident and even death is high already in adolescence (on average 12 years).
The heterozygous form is more common, but the prognosis is more favorable compared to homozygous dyslipidemia.
Andrey Pristrom:
If we talk about heterozygous dyslipidemia, then the average age when the first cardiovascular catastrophe develops is on average 35 years. These are young and able-bodied people who may outwardly appear absolutely healthy. For comparison: usually an atherosclerotic complication develops on average by the age of 55, that is, the difference in the timing of the development of adverse events is 20 years.
Among the secondary reasons are the following:
- the presence of an underlying disease that leads to increased cholesterol levels (hypothyroidism, diabetes mellitus, other endocrine disorders). When the underlying disease is corrected, cholesterol levels stabilize;
- pregnancy (after childbirth, as a rule, cholesterol returns to normal);
- taking certain medications (for example, glucocorticosteroids, hormonal contraceptives, beta-blockers).
In addition, there are a number of risk factors that can contribute to the development of hypercholesterolemia. This is smoking (the earlier a person starts smoking, the faster pathological changes occur), excessive consumption of foods rich in animals and refined fats, overweight and obesity, and low physical activity.
Diagnosis of hypercholesterolemia
As such, there are no specific complaints with elevated cholesterol levels. The main diagnostic method is a lipid profile (total cholesterol, high- and low-density lipoprotein cholesterol, triglycerides are determined). The emphasis is on the level of low-density cholesterol (LDL-C).
In a practically healthy person, this figure should not exceed 3 mmol/l. To confirm the diagnosis, a lipid profile is performed at least twice every one to several weeks.
In the case of a hereditary form, the LDL-C level is usually above 5 mmol/l.
Clinical manifestations are important:
- xanthomas (dense yellow formations) on the upper or lower eyelid or near the nose;
- xanthomas on the tendons (in the form of growths), can form on the Achilles tendon;
- the so-called lipoid arc of the cornea of the eyes - a rim of cholesterol (white or grayish-white).
Andrey Pristrom:
If the LDL-C level is above 5 mmol/l, there are clinical manifestations - there is a high probability of a hereditary form. In this case, family ties are important, in particular, identifying cardiovascular problems in first-degree relatives: father, mother, brother, sister. Hereditary forms are the most potentially dangerous. If a familial form of hypercholesterolemia is established, such patients automatically belong to a group of high cardiovascular risk. And if the patient already has a history of a cardiovascular accident, then the risk increases to very high.
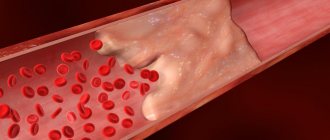
In addition to the lipid profile, it is also recommended to perform an ultrasound of the brachiocephalic arteries in people with severe lipid profile disorders. This study is carried out to identify atherosclerotic plaques (deposits in the walls of blood vessels that are caused by elevated levels of LDL cholesterol), assess its location and condition, changes in the diameter and lumen of the vessel. Atherosclerosis, developing against the background of lipid metabolism disorders, is a systemic process. Therefore, the resulting changes in the brachiocephalic arteries will also occur in other vessels.
Prevention of cardiovascular diseases
With hypercholesterolemia, the issue of preventing the development of cardiovascular accidents is acute. Low-density cholesterol levels are crucial.
Andrey Pristrom:
There is a clear connection between the level of LDL cholesterol and cardiovascular complications: the lower this indicator, the lower the number of cardiovascular accidents. The key value for most patients is LDL-C – 1.4 mmol/l. Therefore, it is necessary to achieve indicators below this figure. Why is that? Studies have shown that at this level of cholesterol, processes in the atherosclerotic plaque are stabilized. The most important thing is that it stops expanding and growing and becomes stable, which, in turn, prevents the development of acute vascular adverse events.
The likelihood of developing cardiovascular accidents is determined by the SCORE scale (cardiovascular risk scale). With 5 or more points it is considered high.
The LDL-C target for patients directly depends on the level of risk:
- with low risk – less than 3 mmol/l;
- with moderate risk – less than 2.6 mmol/l;
- with a high level of risk – less than 1.8 mmol/l;
- with a very high risk level – less than 1.4 mmol/l.
The idea that too low LDL-C levels can have negative consequences for a person's health is erroneous. Although it is believed that the physiological level of LDL cholesterol is above 0.65 mmol/l.
Andrey Pristrom:
Today, thanks to the use of many modern drugs, it has been proven that even with very low LDL-C levels, no additional adverse events occur. Therefore, there is no limit as such below which risks increase. However, the literature has described cases of genetic disorders in individuals whose systems involved in cholesterol synthesis are damaged. Because of this, their LDL-C levels were very low. Observation of them showed that such people practically do not have vascular accidents or other complications.
Treatment of hypercholesterolemia
The main basic class of drugs used to treat lipid metabolism disorders are statins. Their action is aimed at reducing the formation of cholesterol in the liver, thereby reducing its level in the blood.
The algorithm of actions for choosing drug therapy consists of three steps. The first step is to use statins and increase the dose to the maximum (so-called high-intensity statin therapy). If such treatment is effective, therapy remains.
If the response to statins is insufficient, the next step is to add the drug Ezetimibe.
If the two previous prescriptions are ineffective, the regimen is replenished with drugs that block the synthesis of the PCSK-9 protein.
Andrey Pristrom:
If we are talking about those patients who develop an adverse reaction to statins, the algorithm of actions is different. In such cases, Ezetimibe is prescribed first. However, since its intensity in monotherapy is low, a second step is usually needed - drugs that block PCSK-9 protein synthesis.
Side effects of statins include a small risk of developing diabetes, muscle symptoms (weakness and muscle pain), and increased levels of liver enzymes. The true prevalence of such complications is low and often exaggerated (for example, the incidence of significant liver damage is 1 case per 100 thousand).
However, they cannot be ignored, as this can significantly worsen the patient’s quality of life. Therefore, lipid-lowering therapy requires annual laboratory monitoring of muscle and liver parameters. If statins are contraindicated, the question of prescribing other medications is raised.
If none of the drugs has an effect, it is possible to use a method such as plasma apheresis. Its effect is temporary. As a rule, the procedure should be carried out once every 10-14 days, in severe forms - more often.
This information is intended for medical and pharmaceutical professionals only. This information is subject to distribution at the venues of medical or pharmaceutical exhibitions, seminars, conferences and other similar events or direct transmission to medical and pharmaceutical workers. Dissemination of information by any other means that opens access to it to an indefinite number of persons is prohibited. The images used are not of actual patients. BY/CARD/10.2021/pdf/ 312868
What can hypercholesterolemia lead to?
First of all, high cholesterol is the main factor in the development of atherosclerosis. Its deposits on the walls of blood vessels with the formation of atherosclerotic plaques pose a direct threat to all organs and systems of the patient.
Firstly, the lumen of the vessel itself narrows, which means that it begins to let in less and less blood, causing ischemia (oxygen starvation) of the organs that it supplies. The heart, kidneys and brain are primarily affected. The diameter of the vessels supplying these organs narrows due to the presence of atherosclerotic plaques, causing ischemia. With severe damage to the arteries of the legs, chronic insufficiency of blood supply develops, which can lead to the appearance of foci of necrosis and tissue ulceration.
Hypercholesterolemia leads to the formation of plaques in the wall of the largest vessel in our body - the aorta, leading to a loss of its elasticity and thickness. As a result, the wall is stretched under blood pressure and an aortic aneurysm occurs. And this, in turn, can lead to delamination or rupture, which is an extremely dangerous condition for the patient’s life.
Signs and symptoms
Hypercholesterolemia is detected using a laboratory blood test for biochemistry. In addition, there are some external signs by which the presence of this pathology can be determined. The main one is the presence of xanthomas - skin neoplasms formed from pathologically altered cells consisting of lipid inclusions.
They look like dense nodules. Xanthomas accompany all forms of the pathology in question and are one of the external signs of fat imbalance. They do not cause unpleasant or painful sensations in a person. They can dissolve on their own.
How to donate blood for cholesterol?
The following classification of xanthomas is distinguished:
- Tuberous - large plaques are located in the elbows, buttocks, knees, on the back of the fingers, scalp and on the face and have a brown or purple tint with a cyanotic or reddish border.
- Eruptive - small yellow papules. They tend to appear on the buttocks and thighs.
- Tendon - localized mainly in the tendon area.
- Flat – spots of a light orange hue rise slightly above the surface of the skin. In most cases they appear on the palms.
- Xanthelasmas are flat yellow xanthomas of the eyelids. Occurs predominantly in women. They do not disappear on their own.
Another sign of hypercholesterolemia is the appearance of peculiar cholesterol deposits along the border of the cornea of the eyes. They have the shape of a grayish-white or white rim and in medical practice are called lipoid arcs. It appears more often in people who smoke. It is irreversible.
Persons with this sign of hypercholesterolemia are at risk for developing coronary artery disease. With homozygous familial hypercholesterolemia, a significant increase in blood cholesterol levels is observed. In people with this form of pathology, symptoms and signs of the disease develop already in childhood.
During puberty, they often experience atheromatous lesions of the aortic mouth, as well as narrowing of the lumen of the coronary arteries of the heart. They also experience all the clinical manifestations of IHD. The cause of premature death in this case is often acute coronary insufficiency.
The heterozygous form of hereditary hypercholesterolemia has a long and asymptomatic course. Cardiovascular insufficiency manifests itself only in adulthood. According to statistics, the first signs of pathology appear earlier in women by about 10 years than in men.
A long-term increase in blood cholesterol levels over many years, accompanied by such phenomena as arterial hypertension, diabetes mellitus, and smoking, accelerates the formation of atherosclerotic plaques on blood vessels. They narrow the lumen to the point of complete blockage. This, in turn, is fraught with deadly consequences.
These are the main external signs of hypercholesterolemia
How to treat hypercholesterolemia?
The patient must be prescribed a diet low in fat and carbohydrates. As drug therapy, doctors at the CELT clinic use a wide range of lipid-lowering (lowering fat-lipid levels) agents. Their purpose, as well as the regimen of use, is selected individually and depends on the results of the examination of each individual patient.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Types of hypercholesterolemia and its diagnosis
Classification of hypercholesterolemia is carried out according to the main reasons for the development of this pathology. In accordance with the specific features of the course of the disease or according to symptoms, the division of this disease is not carried out. There are 3 types of hypercholesterolemia:
- Primary, or hereditary. It is inherited from parents to children and is caused by gene mutation. It is divided into homozygous and heterozygous. Otherwise known as familial hypercholesterolemia.
- Secondary, or acquired. It is formed as a result of the development of certain pathologies occurring in the body.
- Nutritional. Occurs as a result of overusing foods rich in animal fats.
Familial hypercholesterolemia is often asymptomatic and is characterized by a pronounced increase in the level of low-density lipoproteins in the blood. It is characterized by earlier development of coronary artery disease. Accompanied by symptoms such as chest pain, the formation of subcutaneous cholesterol deposits around the eyes, on the arms and in the tendon area.
WHO classifies hypercholesterolemia into the following types:
- Type 1 – hereditary primary hyperchylomicronemia and hyperlipoproteinemia.
- Type 2a – hereditary polygenic. It is less common and its development can be triggered by poor nutrition. It is characterized by the early development of cardiovascular pathologies and the appearance of xanthomas.
- 2b type. Combined hyperlipidemia. It results from excessive production of triglycerides, apolipoprotein and acetyl-CoA. Characterized by a significant increase in triglycerides in the blood.
- Type 3. Hereditary dys-beta-lipoproteinemia. It is rare and develops as a result of homozygosity of apolipoprotein E.
- Type 4. Endogenous hyperlipidemia. In this case, there is an increase in triglyceride levels.
- Type 5. Hereditary hypertriglyceridemia. The main symptom is an increase in the concentration of very low density lipoproteins and chylomicrons.
And it is also classified according to severity into moderate and severe hypercholesterolemia. In the first case, the level of cholesterol in the blood does not go beyond 7.8 mmol/l. This condition requires additional examination and diet.
Severe hypercholesterolemia corresponds to a cholesterol level higher than 7.8 mmol/l. She requires drug treatment. Impaired lipid metabolism and, as a consequence, the diagnosis of hypercholesterolemia is determined by blood biochemistry. The following 4 indicators are examined:
- total cholesterol;
- low density cholesterol;
- high density cholesterol;
- triglycerides.
This comprehensive blood test is called a lipid profile. Most often, an increase in cholesterol levels that is not associated with heredity is detected during a preventive examination. In addition to laboratory blood tests, the diagnosis of hypercholesterolemia includes collecting the patient’s medical history and analyzing his complaints.
And the patient is also examined, during which external signs of increased cholesterol levels in the blood can be detected. These are xanthomas, xanthelasmas and lipid arch of the cornea. The patient's blood pressure is measured. In people with hypercholesterolemia it is most often elevated.
Treatment methods
To normalize blood cholesterol levels and eliminate hypercholesterolemia, medicinal and non-medicinal treatment methods are used. It is known that the concentration of cholesterol in the blood is often provoked by an unhealthy diet rich in animal fats.
Therefore, correcting the diet with a slight increase in this indicator will help cope with hypercholesterolemia without special medications. If cholesterol levels in the blood are consistently high, while progression of vascular changes is observed and negative symptoms are present, then drug therapy, and sometimes surgical treatment, is necessary.
Non-drug therapy includes the following areas:
- normalization of body weight;
- feasible physical activity;
- restrictions in the diet of animal fats;
- increasing the consumption of vitamins and dietary fiber;
- significant limitation or cessation of alcohol consumption;
- to give up smoking.
According to clinical recommendations, as part of drug treatment, special drugs are prescribed, the action of which is aimed at reducing the concentration of cholesterol in the blood through various mechanisms. One of the main groups of drugs for patients with high lipid levels are statins.
Their action is aimed at reducing the production of cholesterol in the liver, as well as reducing the intracellular content of lipoproteins. In addition, statins stimulate the destruction of fat-like substances and prevent vascular damage.
Drugs in this group are selected individually depending on the severity of the pathology. Self-administration of such drugs is unacceptable, as they have many side effects.
The next group of drugs prescribed for the treatment of hypercholesterolemia are bile acid sequestrants. When they are taken, bile acids containing cholesterol are removed into the intestines and subsequently exited from the body.
Fibrates reduce triglyceride concentrations and increase the content of healthy high-density cholesterol. Usually prescribed in conjunction with statins. The treatment regimen for hypercholesterolemia also includes drugs containing omega-3 polyunsaturated fatty acids.
For severe forms of hypercholesterolemia, extracorporeal treatment methods are used. These include cascade plasma filtration, immunosorption of lipoproteins, hemosorption, plasma sorption. The essence of these methods is to change the properties and composition of the patient’s blood outside the body using special devices.
It is advisable to treat hypercholesterolemia with folk remedies only if there is a slight deviation from the norm in the level of lipoproteins. It is believed that among alternative medicines, the most effective in reducing cholesterol are recipes based on garlic, lemon, and honey. But before starting such treatment, you should consult with your doctor.
Special medications can reduce high cholesterol levels in the blood
Complications of high blood cholesterol levels
The most natural consequence of hypercholesterolemia in clinical practice is called atherosclerosis. This condition is characterized by the formation of atherosclerotic (cholesterol) plaques, compacting the walls of the arteries and narrowing their lumen up to complete occlusion (blockage).
Atherosclerosis can affect the vessels of the brain, heart, kidneys, intestines, lower extremities, and even the aorta. This disease, in turn, provokes a number of other complications:
· Myocardial infarction;
· Coronary heart disease;
· Strokes and micro-strokes;
· Angina pectoris.
The therapeutic prognosis in the treatment of atherosclerosis associated with hypercholesterolemia depends on the balance of pro-atherogenic and anti-atherogenic lipids in the patient’s blood, the rate of development of destructive changes in the vessels, and the location of the affected artery. Complete and timely treatment, coupled with the elimination of modifiable provoking factors, prolongs the patient’s life expectancy and significantly improves its quality.
3. Symptoms and diagnosis
As stated above, hypercholesterolemia is not a disease, which means, in particular, the absence of its own symptoms. The clinical picture is always determined by a specific combination of causes and consequences (for example, obesity and cardiovascular pathology, smoking and hemodynamic disorders in the lower extremities, cerebral transient ischemic attacks against the background of chronic stress, and many others).
Hypercholesterolemia is diagnosed through laboratory tests using special tabular criteria.
About our clinic Chistye Prudy metro station Medintercom page!
Reasons for the development of hypercholesterolemia
Primary hypercholesterolemia develops solely as a result of genetic predisposition (hereditary receipt from parents of a destructive gene responsible for the synthesis of a substance).
Secondary hypercholesterolemia can be caused by concomitant diseases and conditions:
· Diabetes;
· Obstructive pathologies of the liver and gall bladder (including cholelithiasis);
· Hypothyroidism;
· Schematic use of medications (immunosuppressants, diuretics, beta blockers);
· Nutritional reasons (incorrect nutrition with a predominance of animal fats in the normal diet).
The latter factor can provoke both transient and permanent hypercholesterolemia.
The following modifiable and non-modifiable factors contribute to the development and progression of dyslipidemia:
· Smoking;
· Alcohol abuse;
· Physical inactivity;
· Binge eating;
· Stressful personality type;
· Obesity (mainly abdominal, i.e. in the abdomen area);
· Decompensated diabetes mellitus;
· Arterial hypertension (chronic hypertension);
· Genetic predisposition to early atherosclerosis;
· Myocardial infarction;
· Ischemic stroke;
· Male gender;
· Mature age (over 45 years old).
Ignoring symptoms and neglecting adequate therapy leads to the fact that constant hypercholesterolemia leads to severe complications and consequences.