Functions and meaning
Lipids play an important role in the human body. They are found in all cells and tissues and participate in many metabolic processes.
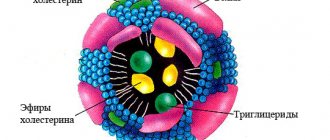
lipoprotein structure
- Lipoproteins are the main transport form of lipids in the body
. Since lipids are insoluble compounds, they cannot independently fulfill their purpose. Lipids bind in the blood to proteins - apoproteins, become soluble and form a new substance called lipoprotein or lipoprotein. These two names are equivalent, abbreviated as LP.
Lipoproteins occupy a key position in the transport and metabolism of lipids. Chylomicrons transport fats that enter the body with food, VLDL deliver endogenous triglycerides to the site of disposal, cholesterol enters cells with the help of LDL, HDL has anti-atherogenic properties.
- Lipoproteins increase the permeability of cell membranes.
- LPs, the protein part of which is represented by globulins, stimulate the immune system, activate the blood coagulation system and deliver iron to the tissues.
What are lipoproteins?
Fat is produced by liver cells, but it needs protein to become a vehicle.
With a sufficient amount of protein in a lipoprotein molecule (over 50.0%), this molecule has a high density and serves as a building element of the cell membrane in the body.
The lipoprotein membrane contains:
- Protein molecules, cholesterol fat molecule, as well as phospholipid molecules,
- The lipoprotein is hydrophilic, therefore it has the properties of binding to the plasma of the blood composition.
The inner core of the lipoprotein has the following molecular composition:
- Ester of a fatty compound (cholesterol),
- Triglyceride molecules,
- Fat-containing acid,
- Vitamin A.
If lipoproteins have a stable standard concentration, then they support the synthesis of fat molecules and components of apoprotein particles (protein in high molecular weight lipoprotein).
Lipoprotein
Classification
Blood plasma lipids are classified by density
(using the ultracentrifugation method). The more lipids a drug molecule contains, the lower their density. There are VLDL, LDL, HDL, and chylomicrons. This is the most accurate of all existing drug classifications, which was developed and proven using a precise and rather painstaking method - ultracentrifugation.
The size of the LP is also heterogeneous.
The largest molecules are chylomicrons, and then in decreasing size - VLDL, LPSP, LDL, HDL.
Electrophoretic classification
LP is very popular among clinicians. Using electrophoresis, the following classes of lipid were identified: chylomicrons, pre-beta lipoproteins, beta lipoproteins, alpha lipoproteins. This method is based on the introduction of an active substance into a liquid medium using a galvanic current.
Fractionation
LPs are carried out to determine their concentration in the blood plasma. VLDL and LDL are precipitated with heparin, and HDL remains in the supernatant.
Reduced index
Alipoproteinemia is a pathology that is caused by genetic inherited disorders in the immune system.
This disease belongs to the section of autoimmune disorders of the body, when the body perceives lipoproteins as its enemies and fights them at the cellular level of the immune system.
Alipoproteinemia manifests itself with the following symptoms:
- Weakness of the whole body
- Inflammation in the tonsils,
- Decreased reflexes.
The pathology of hypolipoproteinemia is asymptomatic.
Weakness of the whole body
Kinds
Currently, the following types of lipoproteins are distinguished:
HDL (high density lipoprotein)
HDL transports cholesterol from body tissues to the liver.
HDL contains phospholipids, which keep cholesterol in suspension and prevent it from leaving the bloodstream. HDL is synthesized in the liver and provides reverse transport of cholesterol from surrounding tissues to the liver for disposal.
- An increase in HDL in the blood is observed in obesity, fatty hepatosis and biliary cirrhosis of the liver, and alcohol intoxication.
- A decrease in HDL occurs in hereditary Tangier disease, caused by the accumulation of cholesterol in tissues. In most other cases, a decrease in the concentration of HDL in the blood is a sign of atherosclerotic vascular damage.
The HDL level differs between men and women. In males, the LP value of this class ranges from 0.78 to 1.81 mmol/l, the norm in women for HDL is from 0.78 to 2.20, depending on age.
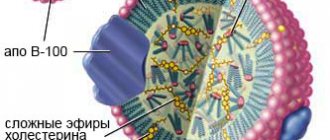
LDL (low density lipoprotein)
LDLs are carriers of endogenous cholesterol, triglycerides and phospholipids from the liver to tissues.
This class of drugs contains up to 45% cholesterol and is its transport form in the blood. LDL is formed in the blood as a result of the action of the enzyme lipoprotein lipase on VLDL. When there is an excess of it, atherosclerotic plaques appear on the walls of blood vessels.
Normally, the amount of LDL is 1.3-3.5 mmol/l.
- The level of LDL in the blood increases with hyperlipidemia, hypothyroidism, and nephrotic syndrome.
- A reduced level of LDL is observed with inflammation of the pancreas, hepatic-renal pathology, acute infectious processes, and pregnancy.
infographics (click to enlarge) – cholesterol and LP, role in the body and norms
VLDL (very low density lipoprotein)
VLDL is formed in the liver. They transport endogenous lipids, synthesized in the liver from carbohydrates, to tissues.
These are the largest LPs, second in size only to chylomicrons. They are more than half triglycerides and contain small amounts of cholesterol. When there is an excess of VLDL, the blood becomes cloudy and takes on a milky tint.
VLDL is a source of “bad” cholesterol, from which plaques form on the vascular endothelium. Gradually, the plaques increase, and thrombosis occurs with the risk of acute ischemia. VLDL is elevated in patients with diabetes and kidney disease.
Chylomicrons
Chylomicrons are absent in the blood of a healthy person and appear only in cases of lipid metabolism disorders
. Chylomicrons are synthesized in the epithelial cells of the small intestinal mucosa. They deliver exogenous fat from the intestine to peripheral tissues and the liver. Most of the transported fats are triglycerides, as well as phospholipids and cholesterol. In the liver, under the influence of enzymes, triglycerides break down and fatty acids are formed, some of which are transported to muscles and adipose tissue, and the other part is bound to blood albumin.
what do major lipoproteins look like?
LDL and VLDL are highly atherogenic
– containing a lot of cholesterol. They penetrate the artery wall and accumulate there. When metabolism is disrupted, LDL and cholesterol levels rise sharply.
HDL are the safest against atherosclerosis
. Lipoproteins of this class remove cholesterol from cells and promote its entry into the liver. From there, it enters the intestines along with bile and leaves the body.
Representatives of all other classes of drugs deliver cholesterol into cells. Cholesterol is a lipoprotein that is part of the cell wall. It is involved in the formation of sex hormones, the process of bile formation, and the synthesis of vitamin D, necessary for the absorption of calcium. Endogenous cholesterol is synthesized in liver tissue, adrenal cells, intestinal walls and even in the skin. Exogenous cholesterol enters the body along with animal products.
Removing cholesterol from the body
The classic route of cholesterol elimination is cholesterol transport from the periphery to the liver (HDL), uptake by liver cells (SR-BI), excretion into bile and excretion through the intestine, where most of the cholesterol is returned to the blood [10].
The main function of HDL is the reverse transport of cholesterol to the liver. Plasma HDL is the result of a complex of different metabolic events. The composition of HDL varies greatly in density, physicochemical properties and biological activity. These are spherical or disc-shaped formations. Disc-shaped HDL is mainly composed of apoprotein AI with an embedded layer of phospholipids and free cholesterol. Spherical HDL is larger and additionally contains a hydrophobic core of cholesteryl esters and small amounts of triglycerides.
In metabolic syndrome, the exchange of triglycerides and cholesterol esters between HDL and triglyceride-rich lipoproteins is activated. As a result, the content of triglycerides in HDL increases, and cholesterol decreases (i.e., cholesterol is not excreted from the body) [11]. The absence of HDL in humans occurs in Tangier disease, the main clinical manifestations of which are enlarged orange tonsils, corneal arch, infiltration of bone marrow and mucosal layer of the intestine [3].
To briefly summarize, it is not cholesterol itself that is scary, which is a necessary component that ensures the normal structure of cell membranes and the transport of lipids in the blood, but in addition it is a raw material for the production of steroid hormones. Metabolic disorders manifest themselves when the balance of LDL and HDL is disturbed, which reflects a disruption of the lipoprotein transport system, including liver function, bile formation and the participation of macrophages. Therefore, any liver diseases, as well as autoimmune processes, can cause the development of atherosclerosis, even with a vegetarian diet. If we return to the original experiments of N.A. Anichkov on feeding rabbits with food rich in cholesterol, we will see that cholesterol is not found in the natural diet of rabbits and therefore, like a poison, disrupts the functioning of the liver, causes severe inflammation of blood vessels and, as a result, the formation of plaques.
Restoring this balance artificially (for example, at the molecular level using nanoparticles) will someday become the main method of treating atherosclerosis (see “Nanoparticles for “bad” cholesterol!” [13]). - Ed.
Dyslipoproteinemia is a diagnosis for disorders of lipoprotein metabolism
Dyslipoproteinemia develops when two processes are disrupted in the human body: the formation of lipoproteins and the rate of their elimination from the blood. An imbalance in the ratio of LP in the blood is not a pathology, but a factor in the development of a chronic disease,
in which the arterial walls become denser, their lumen narrows and the blood supply to the internal organs is disrupted.
When cholesterol levels in the blood increase and HDL levels decrease, atherosclerosis develops, leading to the development of deadly diseases.
Etiology
Primary
dyslipoproteinemia is genetically determined.
Causes of secondary
dyslipoproteinemias are:
- Physical inactivity,
- Diabetes,
- Alcoholism,
- Kidney dysfunction
- Hypothyroidism,
- Hepatic-renal failure,
- Long-term use of certain medications.
The concept of dislipoproteinemia includes 3 processes - hyperlipoproteinemia, hypolipoproteinemia, alipoproteinemia. Dyslipoproteinemia is quite common: every second inhabitant of the planet experiences similar changes in the blood.
Hyperlipoproteinemia is an increased level of lipoproteins in the blood due to exogenous and endogenous causes.
The secondary form of hyperlipoproteinemia develops against the background of the underlying pathology. In autoimmune diseases, drugs are perceived by the body as antigens to which antibodies are produced. As a result, antigen-antibody complexes are formed, which are more atherogenic than the drugs themselves.
- Type 1 hyperlipoproteinemia is characterized by the formation of xanthomas - dense nodules containing cholesterol and located above the surface of the tendons, the development of hepatosplenomegaly, and pancreatitis. Patients complain of a deterioration in their general condition, a rise in temperature, loss of appetite, and paroxysmal abdominal pain, which intensifies after eating fatty foods.
Xanthomas (left) and xanthelasmas (center and right) are external manifestations of dyslipoproteinemia
- In type 2, xanthomas are formed in the area of the tendons of the feet and xanthelasmas in the periorbital zone.
- Type 3 – symptoms of cardiac dysfunction, the appearance of pigmentation on the skin of the palm, soft inflamed ulcers over the elbows and knees, as well as signs of damage to the blood vessels of the legs.
- With type 4, the liver enlarges, coronary heart disease and obesity develop.
Alipoproteinemia is a genetically determined disease
with an autosomal dominant type of inheritance. The disease is manifested by enlarged tonsils with an orange coating, hepatosplenomegaly, lymphadenitis, muscle weakness, decreased reflexes, and hyposensitivity.
Hypolipoproteinemia –
low levels of LP in the blood,
often asymptomatic. The causes of the disease are:
- Heredity,
- Poor nutrition
- Passive lifestyle,
- Alcoholism,
- Pathology of the digestive system,
- Endocrinopathy.
Dyslipoproteinemias are: organ or regulatory,
toxigenic, basal - study of the level of LP on an empty stomach, induced - study of the level of LP after eating, drugs or exercise.
Transportation disruption
With disturbances in the ability to transport lipids, as well as with deviations in lipid metabolism, the potential of the human body decreases, the body’s ability to quickly transmit impulses along the nerve endings of the system decreases.
If lipid metabolism is disrupted at the stage of formation of lipid molecules, this is a pathology of hypoproteinemia, but if metabolism is disrupted at the stage of utilization, then this is a pathology of hyperproteinemia.
When lipid metabolism is disturbed, the diagnosis of dyslipoproteinemia is most often made. This pathology develops when there is a deviation in the synthesis of lipoproteins, as well as in deviations in the process of removing them from the body.
This disorder of lipid metabolism causes pathologies in the bloodstream system:
- The arterial membranes narrow,
- The elasticity of the arterial membranes is lost,
- Plaques form on the inner sides of the arterial membranes,
- The passage of blood in the vessels and its speed are disrupted.
Dyslipoproteinemia is a pathology that is at the origins of the development of atherosclerosis.
The concept of the diagnosis of dyslipoproteinemia consists of such processes of its development, where each stage can be a separate pathology with characteristic symptoms:
- Hypolipoproteinemia,
- Hyperlipoproteinemia,
- Alipoproteinemia.
Dyslipoproteinemia
Diagnostics
It is known that excess cholesterol is very harmful for the human body. But a lack of this substance can lead to dysfunction of organs and systems. The problem lies in hereditary predisposition, as well as in lifestyle and dietary habits.
Diagnosis of dyslipoproteinemia is based on medical history, patient complaints, clinical signs - the presence of xanthoma, xanthelasma, lipoid arch of the cornea.
The main diagnostic method for dyslipoproteinemia is a blood lipid test. The atherogenicity coefficient and the main indicators of the lipid profile - triglycerides, total cholesterol, HDL, LDL - are determined.
A lipidogram is a laboratory diagnostic method that identifies lipid metabolism disorders that lead to the development of heart and vascular diseases. A lipidogram allows the doctor to assess the patient’s condition, determine the risk of developing atherosclerosis of the coronary, cerebral, renal and hepatic vessels, as well as diseases of the internal organs. Blood is donated to the laboratory strictly on an empty stomach, at least 12 hours after the last meal. One day before the test, avoid drinking alcohol, and an hour before the test, avoid smoking. On the eve of the analysis, it is advisable to avoid stress and emotional overstrain.
The enzymatic method for studying venous blood is the main one for determining lipids. The device records samples pre-stained with special reagents. This diagnostic method allows you to conduct mass examinations and obtain accurate results.
It is necessary to take tests to determine the lipid spectrum for preventive purposes, starting from youth, once every 5 years. Persons over 40 years of age should do this annually.
Blood tests are carried out in almost every district clinic. Patients suffering from hypertension, obesity, heart, liver and kidney diseases are prescribed a biochemical blood test and a lipid profile. Family history, existing risk factors, monitoring the effectiveness of treatment are indications for prescribing a lipid profile.
The results of the study may be unreliable after eating food the day before, smoking, stress, acute infection, pregnancy, or taking certain medications.
Diagnosis and treatment of pathology is carried out by an endocrinologist, cardiologist, therapist, general practitioner, and family doctor.
Lipidogram and biochemical blood test
In order to find out the level of b lipoproteins in the body, you should donate blood for a biochemical analysis, which displays the amount of cholesterol in the blood. In addition to biochemistry, the patient is required to receive a referral for a lipid profile, which recognizes the cholesterol fractions that are in the human circulatory system.
A lipid profile is prescribed as a last resort when there is a suspicion of elevated cholesterol levels, which can be good or bad. If there is a sharp decrease in the concentration of high-density lipoproteins, it is worth undergoing additional examinations in order to exclude the development of atherosclerosis.
To assess the risk of developing coronary heart disease and determine treatment tactics, an analysis of high-grade lipoproteins with an indicator of total cholesterol should be performed.
Risk level for developing cardiovascular diseases
| Index | Norm | Low | Moderate | High |
| Total cholesterol | 3,3-5,2 | Less than 4.8 | 4,8-6,0 | More than 6.0 |
| LDL (low density lipoprotein) | 0-3,9 | Less than 3.0 | 3,0-4,0 | More than 4.0 |
| HDL (high density lipoprotein) | 0,7-2,0 | More than 1.2 | 1,0-1,2 | Less than 1.0 |
| Triglycerides | 0,45-1,86 | Less than 1.7 | 1,7-2,2 | More than 2.2 |
The level of beta lipoproteins in the blood should be kept under control. If the readings are elevated, you should consult a doctor who will prescribe treatment. To determine the risk of developing coronary heart disease, it is important to correctly calculate the atherogenic coefficient using the formula K = total cholesterol - HDL / HDL. It is worth considering that HDL has antiatherogenic properties.
Norm of atherogenic coefficient in units:
- in newborns – no more than 1;
- in men whose age is between 20-30 years;
- in women whose age does not exceed 30 years – up to 2.2;
- in an adult 40-60 years old – up to 3.5.
The atherogenicity index in individuals who suffer from coronary heart disease will reach 4-6.
What factors are taken into account when deciphering the analysis?
The results of the studies should be studied by the attending physician. It is worth remembering that in people who have had heart attacks or strokes, the norm of low-density lipoproteins will be slightly lower. In addition, the presence of:
- systematically increased blood pressure;
- cigarette smoking habits;
- atherosclerosis;
- chronic diseases that develop as a result of absolute or relative deficiency of the pancreatic hormone insulin;
- impaired blood supply to the brain.
The blood collection process is quick and painless
High cholesterol or hypercholesterolemia leads to the formation of atherosclerotic plaques.
When is it necessary to get tested?
The main indication for taking a cholesterol test is the age category of the patient. In older people, cholesterol tends to accumulate in excessive amounts. It is better to start controlling your own health from the age of 20-30. Blood sampling for biochemistry to detect elevated levels of lipoproteins should be carried out every 12 months.
In addition, additional indications for conducting a biochemical blood test include the presence of a hereditary factor (in the case where close relatives of the patient suffer from high cholesterol, we can talk about hereditary susceptibility to these ailments), excess body weight, heart disease, diabetes, high blood pressure .
How to donate blood correctly
Blood sampling from a vein must be done in a special laboratory. It is very important to take the test on an empty stomach (it is advisable not to eat 12-14 hours before the planned hour of the test). During this period of time, you should drink clean water, thanks to which you can get the most accurate cholesterol readings.
Experts have developed a number of rules that must be followed if there is a need to donate blood for biochemistry. 48 hours before blood sampling, you should avoid physical activity and avoid all kinds of stressful situations. If the patient’s profession involves heavy physical labor, it is recommended to take a week’s break from work and only then go to the medical laboratory.
A recent history of acute respiratory viral infection or influenza should be a reason to postpone testing for 40-50 days. It is worth remembering that while carrying a child, cholesterol levels drop sharply, and after the birth of the baby, real readings can be achieved only 60-90 days after birth.
When using medications, it is important to inform your doctor about this so that he can understand whether any drug has an effect on the biochemistry result. To achieve the most accurate result, it is important to eat right the entire week before blood collection. You will have to completely give up fatty foods during this period of time.
Cholesterol does not dissolve in water, so low-density lipoproteins and special protein compounds are used to transport it
Treatment
Diet therapy plays a huge role in the treatment of dyslipoproteinemia.
Patients are advised to limit the consumption of animal fats or replace them with synthetic ones, and eat up to 5 times a day in small portions. The diet must be enriched with vitamins and dietary fiber. You should avoid fatty and fried foods, replace meat with sea fish, and eat plenty of vegetables and fruits. General restorative therapy and sufficient physical activity improve the general condition of patients.
Figure: useful and harmful “diets” from the point of view of drug balance
Lipid-lowering therapy and antihyperlipoproteinemic drugs are intended to correct dyslipoproteinemia. They are aimed at reducing cholesterol and LDL levels in the blood, as well as increasing HDL levels.
Among the drugs for the treatment of hyperlipoproteinemia, patients are prescribed:
- Statins - Lovastatin, Fluvastatin, Mevacor, Zocor, Lipitor. This group of drugs reduces the production of cholesterol by the liver, reduces the amount of intracellular cholesterol, destroys lipids and has an anti-inflammatory effect.
- Sequestrants reduce cholesterol synthesis and remove it from the body - Cholestyramine, Colestipol, Cholestipol, Cholestan.
- Fibrates reduce triglyceride levels and increase HDL levels - Fenofibrate, Ciprofibrate.
- B vitamins.
Hyperlipoproteinemia requires treatment with lipid-lowering drugs “Cholesteramine”, “Nicotinic acid”, “Miscleron”, “Clofibrate”.
Treatment of the secondary form of dyslipoproteinemia consists of eliminating the underlying disease.
Patients with diabetes are advised to change their lifestyle, regularly take antihyperglycemic drugs, as well as statins and fibrates. In severe cases, insulin therapy is required. In case of hypothyroidism, it is necessary to normalize the function of the thyroid gland. For this purpose, patients undergo hormone replacement therapy.
Patients suffering from dyslipoproteinemia are recommended after the main treatment:
- Normalize body weight,
- Dose physical activity
- Limit or eliminate alcohol consumption,
- If possible, avoid stress and conflict situations,
- Stop smoking.
Treatment of elevated beta lipoprotein levels
When prescribing therapy, the doctor must take into account the individual characteristics of the body. It is not advisable to use medications when the level of lipoproteins is at the permissible limit or slightly exceeds it.
In this case, the following will help restore health:
- Proper nutrition, excluding dishes containing significant amounts of animal fat. You will have to exclude the consumption of fatty meat, cheese, chips, fried potatoes, pizza, ice cream, sausage and various confectionery products. The listed products must be replaced with horse meat, rabbit, turkey, tilapia and plenty of fresh vegetables and fruits.
- Peanuts and almonds, oats and barley, and legumes help lower cholesterol.
- Systematic sports activities. Slow evening walks in the fresh air are very useful.
- Drink 2-2.5 liters of clean water per day.
- Complete elimination of bad habits. Alcohol-containing drinks and smoking contribute to increased cholesterol.
By following all the doctor’s recommendations, you can quickly restore your health. If there is an increase in lipoproteins, medications that contain a statin and help block the production of compounds by the liver may be prescribed. Treatment will also be required in cases where the levels are low.