Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
Heart rhythm disorders (arrhythmias) are conditions in which the heart beats irregularly, too fast, or too slow. With frequent heart contractions - above 100 beats per minute in adults, this condition is called tachycardia, with rare - less than 60 beats per minute, it is called bradycardia. Some types of arrhythmia have no symptoms. If the arrhythmia is symptomatic, then the main complaints are palpitations or a feeling of a pause between heartbeats. Sometimes patients may complain of dizziness, fainting, shortness of breath or chest pain. Most types of arrhythmia are not a serious threat to the patient, but complications such as stroke or heart failure can often occur, and sometimes the arrhythmia can lead to cardiac arrest.
The Innovative Vascular Center employs experienced cardiologists who will help determine exactly why cardiac arrhythmia occurs and prescribe the correct treatment. In addition to drug therapy, our clinic implants artificial pacemakers (pacemakers) of any configuration. Timely and correct treatment allows our patients to avoid many complications, which means prolonging life and improving its quality.
Slow heartbeat - bradycardia
Bradycardia is a condition where the heart beats so slowly that it cannot pump enough blood to meet the body's needs. If bradycardia is left untreated, it can lead to extreme fatigue, dizziness, or fainting because not enough blood is supplied to the brain. This condition can be corrected by using an electronic pacemaker, which makes the heart beat normally.
Bradycardia occurs for various reasons:
- Sick sinus syndrome
The appearance of sinus bradycardia as a result of a “malfunction” in the sinus node (the natural pacemaker of the heart) occurs when discharges for contractions occur too infrequently. A weak sinus node can develop with age or be a consequence of illness. Some medications may also cause or worsen bradycardia. This arrhythmia may be temporary or permanent. It can be treated with medications or an electronic pacemaker.
- Blockage of the heart pathways
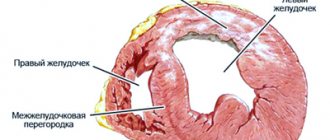
Heart block is a slowing or interruption of the electrical signal to the lower chambers of the heart (ventricles) that cause the heart muscle to contract. The heart's electrical conduction system typically sends signals from the upper chambers of the heart (atria) to the lower chambers (ventricles), which causes coordinated contractions of the heart muscle. Complete blockade of the atrioventricular node can manifest as a sudden loss of consciousness, since the ventricles contract very rarely without stimulus from the sinus node. An artificial pacemaker can eliminate this problem and normalize heart function.
Arrhythmia in children
Arrhythmias in children can appear at any age, but are more common during the neonatal period, at 4-5, 7-8 years and in adolescents [3].
In many cases, arrhythmias are asymptomatic and are detected during routine examinations. The higher prevalence of arrhythmias in children of pubertal age is associated with hormonal age-related changes. In this case, children complain of palpitations during exercise or at rest, weakness, fatigue, headaches, insomnia, periodic chest pain and increased blood pressure. Heart failure develops quickly, especially in children of the first year of life, and can lead to sudden cardiac death syndrome. Other causes of arrhythmia in childhood:
- damage to the nervous system in the perinatal period;
- congenital dysregulation (immaturity) of autonomic regulation of cardiac activity;
- childhood infections or previous congenital infections;
- endocrinological diseases;
- dehydration with prolonged vomiting, diarrhea, sweating;
- hypo- and hyperthermia;
- congenital and acquired heart defects and conduction tract anomalies.
Complicated pregnancy and childbirth, fetal malnutrition, prematurity, intrauterine infections contribute to arrhythmias in children, and, as a rule, in children with a history of arrhythmias, various cardiac diseases are detected in close relatives.
Rapid heartbeat - tachycardia
- Supraventricular tachycardia
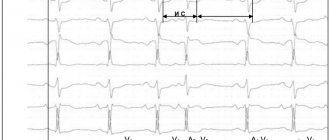
This is a rapid heartbeat in the atria (upper chambers of the heart) or in the atrioventricular (atrioventricular) node, the electrical connection between the atria and ventricles. The first signs of atrial fibrillation are usually detected on an ECG. Atrial fibrillation can be permanent or paroxysmal (periodic) in form, which determines the approach to treatment. Sinus tachycardia is a rapid heartbeat with the formation of regular complexes on the ECG. Sinus arrhythmia is usually associated with an emotional background, elevated temperature, endocrine diseases of the thyroid gland, as well as a predominance of the sympathetic autonomic nervous system.
- Atrial flutter
For atrial flutter to occur, an additional or early electrical impulse must move around the atrium in a circular path rather than along its normal path. This electrical signal causes the atria to contract very quickly, which is usually not life-threatening, but can cause chest pain, dizziness, or other more serious problems. Many chronic heart diseases lead to the development of flutter and atrial fibrillation - its variety.
- Atrial fibrillation
Coronary heart disease often leads to arrhythmia. This common form of tachycardia is more common in women and occurs when there is excess electrical activity in the atria that is extremely disorganized. The manifestation of this electrical activity is very frequent and chaotic contractions of the atria. The atria lose their contractile function, which leads to stagnation of blood in them and can contribute to the formation of clots. Blood clots are the main cause of complications and danger of atrial fibrillation, since they can break away from the atria and enter the general bloodstream. Such a blood clot can cause a blockage of any artery in the body (embolism), leading to a stroke or gangrene of the limbs.
- Paroxysmal supraventricular tachycardia (PSVT)
With PSVT, heart rate increases from 140 to 250 beats per minute (the norm is 60-90 beats per minute). Why does this condition happen, cause trouble, but rarely life-threatening? The causes of this type of cardiac arrhythmia are associated with congenital additional electrical pathways between the atria and ventricles. Idiopathic supraventricular tachycardia is treated by destroying additional electrical pathways using radiofrequency ablation. Tachycardia is felt as an increased heartbeat and is very worrying for patients.
- Wolff-Parkinson-White syndrome (WPW)
In people with Wolff-Parkinson-White syndrome (WWS), extra, abnormal electrical pathways in the heart lead to periods of very fast heartbeat (tachycardia). Most people with WPW syndrome can lead normal lives. Many have no symptoms and no episodes of tachycardia. In some people, WPW syndrome can cause a rapid heartbeat (paroxysmal supraventricular tachycardia), when the heart rate rises to 240 beats per minute (normal is 60 to 80 beats per minute). Other symptoms include palpitations, shortness of breath, fainting, and angina (chest pain) with exercise. The first symptoms of this form of cardiac arrhythmia do not always require treatment, but a thorough examination by a cardiologist is necessary.
- Ventricular tachycardia
Ventricular tachycardia occurs when the ventricles (lower chambers of the heart) contract too quickly, making this arrhythmia life-threatening. This condition can be very serious as the ventricles are responsible for pumping blood to the rest of the body. If the tachycardia becomes so severe that the ventricles cannot pump blood effectively, it can be life-threatening. Tachycardia can be treated with medications. Other procedures include implantation of a defibrillator, catheter radiofrequency ablation, or surgical removal of the heart's accessory pathways. Ventricular extrasystole is a cardiac arrhythmia, which manifests itself as a sudden strong interruption in the functioning of the heart. It is clearly visible on the ECG and interrupts the normal heart rhythm. Bigemeny is one extrasystole every normal cardiac cycle. Trigemeny - extrasystole after two normal cycles. This poor prognostic sign is of great importance and requires immediate attention to a cardiologist.
- Ventricular fibrillation
Erratic and inefficient contractions of the ventricles occur when the electrical signal that normally causes the heart to beat breaks up and travels along random paths around the ventricles instead of following its normal route. The result is a series of rapid but ineffective contractions of the ventricles, leading to loss of consciousness as a result of a sharp drop in blood pressure. This means that without emergency treatment, fibrillation becomes fatal, as it turns off the pumping function of the heart and stops blood circulation. Fibrillation can be stopped with an electric shock or a blow to the heart using a defibrillator. The discharge allows you to “reset” the electrical activity of the heart and return to normal rhythm. Ventricular fibrillation occurs with myocardial infarction, severe chronic heart disease, hemorrhagic shock, and intracardiac procedures.
Symptoms of arrhythmia
- Feeling of interruptions and sinking heart.
- Palpitations, “fluttering” in the fingertips.
- Pain in the heart area.
- Dyspnea.
- Edema.
- Increased fatigue.
- Fear.
- Presyncope and fainting.
- Sleep disorders.
Children may have a delay in the rate of psychomotor development, tearfulness, and chest deformation.
Children experience vomiting, anxiety, shortness of breath, refusal to eat, and cold sweat. In some cases, arrhythmias are signs of life-threatening conditions:
- arrhythmic collapse or shock;
- heart failure;
- myocardial ischemia (acute coronary syndrome);
- sudden cardiac death.
Forecast
Cardiac arrhythmias are dangerous because they can lead to sudden cardiac arrest due to complete blockade of conduction. In severe arrhythmia, there is a high risk of ventricular fibrillation, which can be fatal. Atrial fibrillation leads to the formation of blood clots in the atria and their transfer to other organs with the development of stroke and gangrene of the extremities. The probability of an unfavorable outcome in patients with arrhythmias depends on the form of rhythm disturbance and is more than 20% per year. You should not rely on folk remedies - arrhythmia is very dangerous and requires correction by a professional cardiologist.
Diagnostics
Of course, the central role in the diagnosis of arrhythmias is played by electrocardiogram analysis, single ECG recording or 24-hour (Holter) monitoring.
An ECG with stress and functional studies are performed. Sometimes a revil-implantable device is installed that continuously records the ECG for several months. Additionally, an electroencephalogram, genetic testing, MRI or CT scan of the heart, and echocardiography are performed. Laboratory methods for diagnosing arrhythmias in order to identify electrolyte disturbances and signs of inflammation deserve special attention. Blood, urine, nail or hair tests are taken to determine the levels of magnesium, potassium, sodium, and chlorine. Blood tests are more revealing.
You can perform a complex laboratory test "Cardiorisk", including determination of troponin levels, NT-pro BNP; C-reactive protein, homocysteine, triglycerides, lipoprotein, creatine kinase, LDH, cholesterol, low and high density lipoproteins, D-dimer.
To monitor the effectiveness of treatment, a study of the level of drugs amiodarone, lidocaine, procainamide in the blood is prescribed using high-performance liquid chromatography.
Bibliography
- Guzovskaya, E.V. Pathophysiology of the heart: textbook/ / E.V. Guzovskaya, S.F. Nepomnyashchy; GBOU VPO IGMU of the Ministry of Health of Russia - Irkutsk, IGMU - 48 p.
- Zatonskaya, E.V. Epidemiology of arrhythmias (review of literature data)/ E.V. Zatonskaya, G.V. Matyushin, N.G. Gogolashvili, N.N. Novgorodtseva - Text: direct // Siberian Medical Review, 2021.- No. 3.- P.5-16.
- Sozonov, A.V. The role of a single-channel electrocardiogram at home in the diagnosis of heart rhythm disorders in children / A.V. Sozonov, Yu.A. Trunova, O.S. Pokusaeva-text: direct // Russian Journal of Cardiology, 2021.-No. 24 (add.) – P. 18-19.
- Hingorani P., Natekar M., Deshmukh S., Karnad DR, Kothari S., Narula D., Lokhandwala Y. Morphological abnormalities in baseline ECGs in healthy normal volunteers participating in phase I studies // Indian. J. Med. Res. - 2012. - Vol. 135. - P. 322-330.
Author:
Pugonina Tatyana Alekseevna, Therapist
What's the forecast?
The prognosis for life with atrial fibrillation is determined primarily by the causes of the disease. For example, for survivors of acute myocardial infarction and significant cardiosclerosis, the short-term prognosis for life can be favorable, but for health in the medium term unfavorable, since in a short period of time the patient develops chronic heart failure, which worsens the quality of life and shortens it duration.
However, with regular use of medications prescribed by a doctor, the prognosis for life and health undoubtedly improves. And patients with a permanent form of MA registered at a young age, with proper compensation, live with it for up to 20-40 years.
Treatment of arrhythmia
Treatment can be conservative or surgical.
In severe cases, surgical interventions are performed to install an artificial pacemaker, cardioverter-defibrillators, radiofrequency and cryoablation (destruction of the focus generating pathological impulses with electricity or deep freezing). In emergency cases, intravenous administration of antiarrhythmic drugs is prescribed. First aid for arrhythmia in children is to provide fresh air, clear the airways and ensure rest. In the first minutes, you can apply an ice pack to the child’s face, tilt his head down for a couple of minutes, and press on the root of the tongue. Drug therapy is used as prescribed by the doctor. The choice of drug depends on the type of arrhythmia and the individual characteristics of the patient. Tablets for arrhythmia are prescribed by a cardiologist or therapist; you cannot take them yourself. Besoprolol, amiodarone, nadolol, atenolol or other β-blockers are prescribed.
Prevention of rhythm disturbances
- Treatment of somatic diseases and regular medical examination for these conditions (coronary heart disease, hypertension)
- Proper balanced nutrition (products rich in vitamins and microelements);
- Light physical activity (morning exercises, walking in the fresh air, swimming), exercise therapy according to a specially designed scheme
- Correct work and rest schedule
- Categorical refusal to smoke, drink alcohol, coffee, strong tea
- Weight control (obesity prevention)
- Psycho-emotional peace
When do interruptions of functional origin occur?
The functional nature of extrasystoles is spoken of when a person does not have significant heart damage, and the main cause of interruptions is a temporary change in the electrolyte composition of the heart.
Most often in this situation, extrasystoles occur in the following cases:
- Emotionally labile persons with signs of neurocirculatory dystonia
- Severe mental or physical stress
- Smoking
- Coffee abuse
- Alcohol abuse
- Use of narcotic drugs
- Energy
They may also occur against the background of the following diseases and conditions:
- Stomach ulcer
- Cholelithiasis
- Hiatal hernia
- After a large meal
- In a dream
- Hormonal disorders (for example, thyroid dysfunction in the form of hyper/hypothyroidism)
- Cervical osteochondrosis
- When taking certain medications
When do interruptions in the functioning of the heart of organic origin occur?
As for extrasystoles of organic origin, this is the result of pathological changes in the heart itself in the form of the following diseases:
- IHD, such as previous myocardial infarction
- myocardial dystrophy
- cardiosclerosis
- various channelopathies (long QT syndrome, Brugada syndrome)
- the presence of congenital additional pathways (for example, WPW syndrome)
- dilated cardiomyopathy
- atrial enlargement
- myocarditis
- acquired and/or congenital heart defects (for example, atrial septal defect or aortic valve stenosis)
- pericarditis and other heart diseases
The reason for this extrasystole is the presence of a focus, for example, scar tissue, which has an unfavorable prognostic value.
The causes of paroxysmal (episodic) heart rate accelerations are approximately the same. With all the components, supraventricular rhythm disturbances are safer, in contrast to ventricular ones.