Decoding the results is the competence of a pediatrician, therapist or specialist, since it is important not only to analyze the numbers, but also to compare deviations from the norms of different indicators, to compare the information obtained during examination and history taking. To have an overview and be prepared when you see your doctor, learn what blood elements are tested in the laboratory, how to interpret the results, and what abnormalities may mean.
Why is a leukocyte blood formula needed?
The leukocyte formula is the percentage of leukocytes in the blood serum (eosinophils, neutrophils, lymphocytes, basophils, monocytes).
This analysis allows you to determine the current state of the immune system, identify inflammatory processes in the patient’s body and determine the etiology of allergies. It is known that leukocytes protect the human body from dangerous microorganisms. One of the main tasks of leukocytes is the destruction of foreign particles. If an inflammatory process occurs in the patient’s body, it is immediately reflected in the leukocyte count.
Complete blood count (CBC/Diff - 5 fractions of leukocytes) - capillary blood in Moscow from day 1
from 290 ₽
Sign up
Clinical blood test (CBC/Diff - 5 leukocyte fractions) + ESR in Moscow from day 1
from 294 ₽
Sign up
Complete blood count (CBC/Diff - 5 fractions of leukocytes) in Moscow from 1 weekday
from 290 ₽
Sign up
When leukocyte counts change in the blood, it is necessary to determine in which direction the deviation occurs. This study will help you quickly find the problem and make a diagnosis. However, it should be taken into account that changes in blood parameters without in-depth diagnostics are not a characteristic and final sign for making a diagnosis.
What indicators does the blood test contain?
Donating blood for testing is necessary during planned hospitalization, to assess the effectiveness of the therapy, and during pregnancy. To make an accurate diagnosis and prescribe treatment, the doctor always prescribes a general blood test. Material for research is taken from a finger or from a vein. The second option is preferable, since venous blood more accurately shows the level of hemoglobin and red blood cells.
First of all, red blood cells, white blood cells and platelets are analyzed, as well as:
- Hemoglobin level.
- Erythrocyte indices.
- Hematocrit level.
- Reticulocyte count.
Additionally, the erythrocyte sedimentation rate (ESR), color and blood clotting period are determined.
An extended study involves indicating the leukocyte formula, including the count of eosinophils, lymphocytes, monocytes, band and segmented neutrophils.
When is the test prescribed?
A clinical blood test with a leukocyte formula is indicated for patients with various pathologies. It allows you to assess a person’s health status with a comprehensive and timely diagnosis of diseases, including those occurring in a latent form.
Indications for a clinical blood test with a leukocyte formula are:
- medical examination or routine medical examination;
- preparation for surgical treatment;
- infection or suspected infection;
- suspicion of inflammation or parasitic infestation in the patient’s body;
- allergic reactions;
- prescribing certain medications;
- monitoring the effectiveness of treatment.
Before donating capillary blood, it is recommended not to drink alcohol during the day, not to eat for 2-3 hours, not to smoke for 30 minutes and to avoid stress and excessive physical activity.
Clinical blood test is a laboratory study assessing the quantitative and qualitative characteristics of all classes of blood cells, including a cytological examination of a peripheral blood smear to calculate the percentage of leukocyte varieties and determine the erythrocyte sedimentation rate.
Synonyms Russian
Complete blood count (CBC), hemogram, CAC, complete blood count.
English synonyms
Complete Blood Count (CBC), Hemogram, CBC with White Blood Cell Differential Count, Peripheral Blood Smear, Blood Film Examination.
What biomaterial can be used for research?
Venous blood, capillary blood.
How to properly prepare for research?
- Eliminate alcohol from your diet for 24 hours before the test.
- Children under 1 year of age should not eat for 30-40 minutes before the test.
- Children aged 1 to 5 years should not eat for 2-3 hours before the test.
- Do not eat for 8 hours before the test; you can drink clean still water.
- Avoid physical and emotional stress for 30 minutes before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
A clinical blood test is performed to diagnose quantitative and qualitative changes in the formed elements - blood cells: red blood cells, leukocytes and platelets. Their changes may be caused by disturbances in the hematopoietic process, but most often they are reactive in nature - they reflect the reaction of hematopoiesis to other pathological conditions and diseases. Therefore, a clinical blood test is one of the most common routine tests and is used by doctors of various specialties; it plays a leading role in the primary diagnostic search.
Both venous and capillary blood can be used for the study, with venous blood being preferable. The collection is performed using a vacuum system, most often from the veins in the elbow. A special tube called a vacutainer already contains an anticoagulant (EDTA), which prevents blood clotting. The volume of blood drawn into the vacutainer must correspond to the mark on it - this way the required concentration of the anticoagulant is achieved, which prevents the formation of microclots and, as a result, incorrect calculation of the number of cellular elements and distortion of their morphological structure.
Currently, a clinical blood test is most often performed on a hematology analyzer - a high-tech device that can detect and automatically calculate more than 30 blood characteristics, including counting formed elements, including the main populations of leukocytes. The operating principle of hematology analyzers is based on the passage of a cell suspension through a sensitive element - a laser beam or electric current. Each cell refracts the laser or changes the resistance of the electric current; these changes are proportional to the size of the cell, which is what the analyzer is based on to distinguish them.
If there are deviations in the results of a study on a hematology analyzer, the laboratory diagnostics doctor performs a morphological study of the blood smear. Smear microscopy was included initially in this study. To visually count the formed elements, one or two drops of blood are dripped onto a glass slide, another glass is used to smear it into a thin layer in one motion and is fixed with special substances. The smears are then stained with dyes to make it easier to distinguish and visualize cells and are examined by a doctor under a microscope. Traditionally, the count is carried out per hundred cells and the resulting numbers are recorded as percentages. Knowing the total number of leukocytes, percentages can be converted into absolute values, which much more objectively reflect the state of the leukocyte population.
Parameters determined in the study
Red blood cells are the most numerous blood cells; their main function is the transport of oxygen, which they perform with the help of a special protein they contain - hemoglobin. The hematology analyzer determines the number of red blood cells, hemoglobin content, hematocrit and, based on this, calculates a number of characteristics - the so-called red blood cell indices.
Red blood cells (RBC, Red Blood Cell) are anucleate cells, formed in the bone marrow from reticulocytes, and have the shape of a biconcave disk, which allows them to achieve the maximum possible surface area for binding oxygen. Red blood cells have a diameter of 7-10 micrometers, they are elastic and can easily change shape to safely pass through the smallest vessels - capillaries. In a blood smear they appear as pale red round elements with a clearing in the center. The unit of measurement is 1012 per liter (trillion cells per liter).
Hemoglobin (HGB) is a protein, the main component of red blood cells, which has an affinity for oxygen, which ensures the transport function of red blood cells. Oxygenated hemoglobin gives red blood cells and blood in general their red color.
Hematocrit (HCT) – characterizes the ratio of the volume of red blood cells and plasma. This is a calculation parameter - the hematology analyzer calculates the volume of red blood cells from their number and the average cell volume (MCV).
Mean Corpuscular Volume (MCV, Mean Corpuscular Volume) – is calculated by the analyzer by dividing the sum of cell volumes by the number of red blood cells. It may have a normal value if both microcytosis and macrocytosis are present in the blood. In such situations, you should pay attention to the RDW parameter. The unit of measurement is femtoliter.
The average hemoglobin content in an erythrocyte (MCH, Mean Corpuscular Hemoglobin) – reflects the degree of saturation of the erythrocyte with hemoglobin. Calculated by dividing the hemoglobin concentration by the number of red blood cells.
The average hemoglobin concentration in an erythrocyte (MCHC, Mean Corpuscular Hemoglobin Concentration) also characterizes the saturation of an erythrocyte with hemoglobin. Calculated by dividing hemoglobin by hematocrit.
Distribution of erythrocytes by volume (RDW, Red Cell Distribution Width) - characterizes the degree of variability of erythrocyte volume - anisocytosis. If there is a population of red blood cells in the blood with an altered, but fairly uniform size, RDW values may remain normal. With pronounced differences in the volume of red blood cells, when MCV, which characterizes the average volume of all cells, is normal, RDW will be increased.
Platelets (PLT, Platelet) are blood cells involved in stopping bleeding by forming blood clots. They are not cells; they are fragments of the cytoplasm of bone marrow megakaryocytes. Diameter 2-4 microns.
Mean platelet volume (MPV, Mean Platelet Volume) – platelet volume decreases as cells age, so an increase in this parameter indicates a predominance of young platelets in the population.
Platelet distribution by volume (PDW, Platelet Distribution Width) – characterizes the variability of platelet sizes.
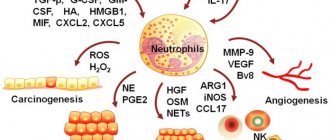
Leukocytes (WBC, White Blood Cell) are a heterogeneous population of nucleated blood cells, the main function of which is to protect the body from foreign agents. Leukocytes include cells of the granulocytic (eosinophils, basophils, neutrophils), monocyte and lymphoid (T- and B-lymphocytes) series. Modern analyzers can differentiate the main five types of leukocytes, but smear microscopy is still the most accurate method for assessing the leukocyte population, as it allows not only to determine the number of different leukocytes, but also to identify changes in their morphology, as well as detect atypical cells.
The percentage of different types of leukocytes in a blood smear is called the leukocyte formula . Staining of blood smears allows you to differentiate 5 types of leukocytes due to different staining of the nuclei and intracellular space (cytoplasm):
- Neutrophils are granulocytic leukocytes: their cytoplasm contains granules with specific active substances that allow them to perform their protective functions (capture and destroy foreign objects). Neutrophils also have a nucleus, according to the structure of which they are divided into band-nuclear and segmented (this is the final stage of maturation following the band-nucleus, at which the nucleus is divided by constrictions into 4-5 lobes). When stained, neutrophil granules turn purple, which, together with the peculiarity of the nucleus, allows them to be distinguished from other granulocytes.
- Eosinophils are granulocytes involved in allergic reactions and antiparasitic immunity. Their granules contain mediators of allergy and inflammation. Eosinophils have a two-segmented nucleus, and their granules are orange-pink in color.
- Basophils are granulocytes that take an active part in immediate allergic reactions. They have an S-shaped non-segmented nucleus, which is often not visible due to large granules of intense blue color containing allergy mediators.
- Lymphocytes are cells with a large nucleus, practically devoid of cytoplasm. Their nucleus is colored intense purple-violet, and the cytoplasm is blue-blue. Lymphocytes participate in more complex immune reactions associated with the recognition of their own and foreign antigens.
- Monocytes are relatively large leukocytes containing an unsegmented bean-shaped nucleus and, unlike lymphocytes, a large amount of cytoplasm. When stained, the nucleus becomes purplish-red, and the cytoplasm is a cloudy bluish-gray. The main function of monocytes is phagocytosis, that is, the absorption and digestion of microorganisms, their own dying cells, etc.
The above types of leukocytes are found normally in a peripheral blood smear. In some diseases, cells that normally should not be in the smear may enter the blood from the bone marrow: for example, blasts are the morphological substrate of acute leukemia. In the conclusion to the study, the number and, if possible, morphological features of atypical cells must be indicated.
In addition to counting leukocytes, microscopy evaluates the morphological characteristics of red blood cells - their size, shape. These parameters are important in the diagnosis of various acquired and congenital anemias.
Erythrocyte sedimentation rate . The test is based on the ability of red blood cells to settle under the influence of gravity in blood that is deprived of the ability to clot. Normally, red blood cells settle slowly; this process is accelerated by agglutination - the sticking of red blood cells to each other, which leads to an increase in the mass of settling particles. Ordinary red blood cells have a negative charge on the membrane, which helps them repel each other. In infectious-inflammatory, autoimmune and some tumor (especially paraproteinemic hemoblastoses) diseases, the protein composition of the plasma changes towards an increase in the content of proteins (for example, immunoglobulins). All protein molecules reduce the membrane charge of red blood cells, promoting their gluing to each other and increasing the rate of sedimentation. The test is carried out for an hour, the height of the resulting sediment is measured in millimeters.
What is the research used for?
- To assess general health (routine medical examinations, screening examinations, etc.);
- For diagnostics at the first stage of a wide range of diseases that may manifest themselves as changes in the characteristics of peripheral blood;
- Monitoring of peripheral blood parameters in diseases accompanied by quantitative and qualitative changes;
- To monitor the toxicity of treatment if the methods used may affect the composition of peripheral blood (for example, chemotherapy, radiation therapy).
When is the study scheduled?
- During screening examinations;
- As a primary diagnosis for suspected diseases that may be accompanied by changes in the cellular composition of the blood;
- In the presence of hematopoietic diseases;
- To monitor the effectiveness and toxicity of treatment.
What do the results mean?
Reference values
Leukocytes
| Age | Reference values |
| Less than 1 year | 6 - 17.5 *10^9/l |
| 1-2 years | 6 - 17 *10^9/l |
| 2-4 years | 5.5 - 15.5 *10^9/l |
| 4-6 years | 5 - 14.5 *10^9/l |
| 6-10 years | 4.5 - 13.5 *10^9/l |
| 10-16 years | 4.5 - 13 *10^9/l |
| More than 16 years | 4 - 10 *10^9/l |
Red blood cells
| Age | Floor | Red blood cells, *10 ^12/ l |
| 3,9-5,9 | ||
| 14 days – 1 month. | 3,3-5,3 | |
| 1-4 months | 3,5-5,1 | |
| 4-6 months | 3,9-5,5 | |
| 6-9 months | 4-5,3 | |
| 9-12 months | 4,1-5,3 | |
| 1-3 years | 3,8-4,8 | |
| 3-6 years | 3,7-4,9 | |
| 6-9 years | 3,8-4,9 | |
| 9-12 years | 3,9-5,1 | |
| 12-15 years | male | 4,1-5,2 |
| female | 3,8-5 | |
| 15-18 years old | male | 4,2-5,6 |
| female | 3,9-5,1 | |
| 18-45 years old | male | 4,3-5,7 |
| female | 3,8-5,1 | |
| 45-65 years | male | 4,2-5,6 |
| female | 3,8-5,3 | |
| > 65 years old | male | 3,8-5,8 |
| female | 3,8-5,2 |
Hemoglobin
| Age | Floor | Hemoglobin, g / l |
| 134-198 | ||
| 14 days – 1 month. | 107-171 | |
| 1-2 months | 94-130 | |
| 2-4 months | 103-141 | |
| 4-6 months | 111-141 | |
| 6-9 months | 114-140 | |
| 9-12 months | 113-141 | |
| 1-5 years | 110-140 | |
| 5-10 years | 115-145 | |
| 10-12 years | 120-150 | |
| 12-15 years | male | 120-160 |
| female | 115-150 | |
| 15-18 years old | male | 117-166 |
| female | 117-153 | |
| 18-45 years old | male | 132-173 |
| female | 117-155 | |
| 45-65 years | male | 131-172 |
| female | 117-160 | |
| > 65 years old | male | 126-174 |
| female | 117-161 |
Hematocrit
| Age | Floor | Hematocrit, % |
| 41-65 | ||
| 14 days – 1 month. | 33-55 | |
| 1-2 months | 28-42 | |
| 2-4 months | 32-44 | |
| 4-6 months | 31-41 | |
| 6-9 months | 32-40 | |
| 9-12 months | 33-41 | |
| 1-3 years | 32-40 | |
| 3-6 years | 32-42 | |
| 6-9 years | 33-41 | |
| 9-12 years | 34-43 | |
| 12-15 years | male | 35-45 |
| female | 34-44 | |
| 15-18 years old | male | 37-48 |
| female | 34-44 | |
| 18-45 years old | male | 39-49 |
| female | 35-45 | |
| 45-65 years | male | 39-50 |
| female | 35-47 | |
| > 65 years old | male | 37-51 |
| female | 35-47 |
Mean erythrocyte volume (MCV)
| Floor | Age | Reference values |
| Less than 1 year | 71 – 112 fl | |
| 1-5 years | 73 – 85 fl | |
| 5-10 years | 75 – 87 fl | |
| 10-12 years | 76 – 94 fl | |
| Female | 12-15 years | 73 – 95 fl |
| 15-18 years old | 78 – 98 fl | |
| 18-45 years old | 81 – 100 fl | |
| 45-65 years | 81 – 101 fl | |
| More than 65 years | 81 – 102 fl | |
| Male | 12-15 years | 77 – 94 fl |
| 15-18 years old | 79 – 95 fl | |
| 18-45 years old | 80 – 99 fl | |
| 45-65 years | 81 – 101 fl | |
| More than 65 years | 81 – 102 fl |
Average hemoglobin content in erythrocytes (MCH)
| Age | Floor | Reference values |
| 30 - 37 pg | ||
| 14 days - 1 month. | 29 - 36 pg | |
| 1 - 2 months | 27 - 34 pg | |
| 2 - 4 months | 25 - 32 pg | |
| 4 - 6 months | 24 - 30 pg | |
| 6 - 9 months | 25 - 30 pg | |
| 9 - 12 months | 24 - 30 pg | |
| 1 – 3 years | 22 - 30 pg | |
| 36 years | 25 - 31 pg | |
| 6 – 9 years | 25 - 31 pg | |
| 9-15 years | 26 - 32 pg | |
| 15-18 years old | 26 - 34 pg | |
| 18-45 years old | 27 - 34 pg | |
| 45-65 years | 27 - 34 pg | |
| > 65 years old | female | 27 - 35 pg |
| > 65 years old | male | 27 - 34 pg |
Mean erythrocyte hemoglobin concentration (MCHC)
| Age | Reference values |
| Less than 1 year | 290 – 370 g/l |
| 1-3 years | 280 – 380 g/l |
| 3-12 years | 280 – 360 g/l |
| 12-19 years old | 330 - 340 g/l |
| More than 19 years | 300 – 380 g/l |
Platelets
| Age | Reference values |
| Less than 10 days | 99 - 421 *10^9/l |
| 10 days – 1 month | 150 – 400 *10^9/l |
| 1-6 months | 180 – 400 *10^9/l |
| 6 months – 1 year | 160 - 390 *10^9/l |
| 1-5 years | 150 – 400 *10^9/l |
| 5-10 years | 180 - 450 *10^9/l |
| 10-15 years | 150 – 450 *10^9/l |
| More than 15 years | 150 – 400 *10^9/l |
RDW-SD (red blood cell volume distribution, standard deviation): 37 - 54.
RDW-CV (red blood cell volume distribution, coefficient of variation)
| Age | RDW-CV, % |
| 14,9 — 18,7 | |
| > 6 months | 11,6 — 14,8 |
Platelet distribution by volume (PDW): 10 - 20 fL.
Mean platelet volume (MPV): 9.4 - 12.4 fL.
Large platelet count ratio (P-LCR): 13 – 43%.
Neutrophils (NE)
| Up to 4 years | 1.5 - 8.5 *10^9/l |
| 4-8 years | 1.5 - 8 *10^9/l |
| 8-16 years | 1.8 - 8 *10^9/l |
| More than 16 years | 1.8 - 7.7 *10^9/l |
Lymphocytes (LY)
| Up to 1 year | 2 - 11 *10^9/l |
| 1-2 years | 3 - 9.5 *10^9/l |
| 2-4 years | 2 - 8 *10^9/l |
| 4-6 years | 1.5 - 7 *10^9/l |
| 6-8 years | 1.5 - 6.8 *10^9/l |
| 8-10 years | 1.5 - 6.5 *10^9/l |
| 10-16 years | 1.2 - 5.2 *10^9/l |
| More than 16 years | 1 - 4.8 *10^9/l |
Monocytes (MO)
| Up to 1 year | 0.05 - 1.1 *10^9/l |
| 1-2 years | 0.05 - 0.6 *10^9/l |
| 2-4 years | 0.05 - 0.5 *10^9/l |
| 4-16 years | 0.05 - 0.4 *10^9/l |
| More than 16 years | 0.05 - 0.82 *10^9/l |
Eosinophils (EO)
| Up to 1 year | 0.05 - 0.4 *10^9/l |
| 1-6 years | 0.02 - 0.3 *10^9/l |
| More than 6 years | 0.02 - 0.5 *10^9/l |
Basophils (BA): 0 - 0.08 *10^9/l.
Neutrophils, % (NE%)
| Up to 1 year | 16 — 45 % |
| 1-2 years | 28 — 48 % |
| 2-4 years | 32 — 55 % |
| 4-6 years | 32 — 58 % |
| 6-8 years | 38 — 60 % |
| 8-10 years | 41 — 60 % |
| 10-16 years | 43 — 60 % |
| More than 16 years | 47 — 72 % |
Lymphocytes,% (LY%)
| Up to 1 year | 45 — 75 % |
| 1-2 years | 37 — 60 % |
| 2-4 years | 33 — 55 % |
| 4-6 years | 33 — 50 % |
| 6-8 years | 30 — 50 % |
| 8-10 years | 30 — 46 % |
| 10-16 years | 30 — 45 % |
| More than 16 years | 19 — 37 % |
Monocytes, % (MO%)
| Up to 1 year | 4 — 10 % |
| 1-2 years | 3 — 10 % |
| More than 2 years | 3 — 12 % |
Eosinophils,% (EO%)
| Up to 1 year | 1 — 6 % |
| 1-2 years | 1 — 7 % |
| 2-4 years | 1 — 6 % |
| More than 4 years | 1 — 5 % |
Basophils,% (BA%): 0 - 1.2%.
Erythrocyte sedimentation rate (photometry)
| Male | Up to 15 years | 2 - 20 mm/h. |
| 15-50 years | 2 - 15 mm/h. | |
| More than 50 years | 2 - 20 mm/h. | |
| Female | Up to 15 years | 2 - 20 mm/h. |
| 15-50 years | 2 - 20 mm/h. | |
| More than 50 years | 2 - 30 mm/h. |
A clinical blood test includes a relatively large number of parameters that must be interpreted in combination. Most often, based on the results of the hemogram, the range of studies necessary to clarify the causes of the changes identified in it is determined.
Changes in erythrocyte parameters. A decrease in the level of hemoglobin and erythrocytes are laboratory manifestations of anemia, and changes in erythrocyte indices characterize its pathogenetic variant and help clarify the causes. Increased levels of red blood cells and hemoglobin may indicate a myeloproliferative disorder (polycythemia vera), but also occurs as a compensatory reaction in active smokers, people with respiratory diseases and heart defects.
Changes in platelets. An increase in platelet count may be a manifestation of essential thrombocythemia (a hematological disease characterized by excess production of platelets in the bone marrow), but also occurs as a compensatory reaction after massive bleeding. A decrease in platelet count is observed with an enlarged spleen, immune thrombocytopenia, as well as aplastic anemia, where it will be combined with a decrease in red blood cells and leukocytes.
Changes in leukocytes. Leukocytosis is considered a manifestation of infectious and inflammatory diseases, and the appearance in the blood smear of a large number of young forms of neutrophils - band and even metamyelocytes (this is called a shift of the leukocyte formula to the left) is characteristic. But too high an increase in the level of leukocytes may be a consequence of an oncohematological disease - acute or chronic leukemia. In this case, morphologically changed cells are found in the blood smear, as well as immature forms of leukocytes (blasts), which normally should not enter the peripheral blood. Leukopenia can accompany severe infectious diseases and in this case characterize the depletion of the leukocyte lineage, and be a consequence of inhibition of bone marrow hematopoiesis, for example, against the background of tumor metastases in the bone marrow.
Erythrocyte sedimentation rate. It is a nonspecific parameter indicating changes in the protein composition of plasma. Most often this is caused by infectious-inflammatory, autoimmune and oncological diseases.
What are leukocytes?
Leukocytes are cells that are found in very large quantities in the blood and in almost all tissues. Their main function is protective and immune. However, they would not be able to fully perform these functions if they were not divided into several varieties within their group, each of which plays its own special role.
There are five main types of leukocytes in the blood. They are determined in tests in the form of a leukocyte formula, so the level of leukocytes in the blood is assessed not only as a whole. The content of these cells is also always calculated. These include:
- neutrophils;
- lymphocytes;
- monocytes;
- eosinophils;
- basophils.
They have different functions, but they work together, influence each other, transmit information between themselves and more. High or low white blood cells belonging to a certain type in the blood indicate various diseases, so determining their number is very important in medical practice.
Normal for pregnant women
| Trimester | White blood cell count (*109) |
| first | 4–9 |
| second | 4–10 |
| third | 14–12 |
Normal for women
| Age | White blood cell count (*109) |
| up to 16 years old | 4,5–12,5 |
| up to 20 years | 4,2–10,5 |
| from 21 years old | 4–9,0 |
Normal for men
| Man's age | White blood cell count (*109) |
| 12–18 years old | 3,5–8 |
| 18–25 years old | 4–9 |
| 25–40 years | 4–8 |
| Over 40 years old | 3–9 |
Normal in children
| Age | White blood cell count (*109) |
| newborn | 10–30 |
| from the fifth day of life | 9–15 |
| from the tenth day of life to one month | 8,5–14 |
| from month to year | 8–12 |
| from one to five years | 7–11 |
| from 5 to 15 years | 6–10 |
| over 15 years old | 5–9 |
Platelets
The main task of platelets is to participate in stopping bleeding. They form the primary plug in the area of vessel damage and participate in the formation of a blood clot. In forms, automatic analyzers are designated by the abbreviation PLT , which comes from the English word platelets (literally, “saucers”) for their peculiar shape.
A decrease in the number of platelets can be accompanied by bleeding and is a consequence of diseases and conditions such as malaria, thrombocytopenic purpura, malignant neoplasms, disseminated intravascular coagulation syndrome and some others.
A high platelet count can cause excessive blood clotting and often has no apparent cause. In this case, the condition is designated as essential thrombocythemia. In addition, thrombocytosis can be caused by iron deficiency anemia, hemolysis, some infectious and autoimmune diseases, and bone marrow damage.
This is where the work with platelets in a classic blood test ends; however, automatic analyzers even in this case offer additional diagnostic capabilities in the form of the following indicators:
- MPV —mean platelet volume. An indicator reflecting the size of cells, which directly depends on their age. An increased MPV may indicate hematological diseases, damage to the spleen, thyrotoxicosis, and progression of atherosclerosis. A decrease in the rate is observed in some genetic diseases, myocardial infarction, childhood infections, cancer chemotherapy and a number of other conditions.
- PCT is the ratio of the total volume of platelets to blood plasma (thrombocrit). It is not a specific indicator, it varies widely physiologically, but it allows one to assess the risk of bleeding and thrombosis.
- PDW —platelet distribution by volume. The indicator has no independent meaning and is assessed in conjunction with other indices.
Leukocyte formula:
| Index | × 10x9/l | ratio, % | |
| Neutrophils | segmented | 2,1–5,4 | 43–71 |
| stab | 0,4–0,3 | 1–5 | |
| Basophils | up to 0.063 | up to 1 | |
| Eosinophils | 0,02–0,3 | 0,5–5 | |
| Lymphocytes | 1,1–3,1 | 17–38 | |
| Monocytes | 0,08–0,5 | 3–12 | |
How to maintain normal neutrophil levels
To have normal levels of segmented neutrophils, you should take care to support your immunity and not waste it. Particular importance should be given to a woman’s environment during pregnancy.
- Vitamins from fruits and vegetables have a positive effect; food should be moderately high in calories and varied.
- According to indications, you should get vaccinated against influenza and other diseases, without waiting for the beginning of the period of increased incidence.
- To the usual hygiene rules of washing hands with soap, you should add rinsing your nose with clean water. Cleansing the mucous membrane and villi improves their protective function.
Hardening procedures can relieve the body of many problems.
Neutrophils
Neutrophils come from red bone marrow, they are formed from a single stem cell, which is the ancestor of all blood cells. However, stem cells do not immediately turn into neutrophils. Between these two forms there are several stages, several intermediate forms.
There are 6 types of neutrophils:
- myeloblasts;
- promyelocytes;
- myelocytes;
- metamyelocytes;
- band neutrophils;
- segmented neutrophils.
Most of all is in the blood of the latter. They are present in an amount of 40–75% of the total number of leukocytes. The number of rod-shaped neutrophils is significantly smaller, they can be 1–6%. The number of young cells does not reach 1%.
Definition and Purposes of Purpose
CBC (complete blood count) is a laboratory diagnostic method for assessing the condition of the body and searching for the source of pathology. This test can be prescribed by a doctor of any specialty. In what cases is OAC prescribed:
- For prevention during medical examinations. The composition of the blood is relatively constant and rarely goes beyond the normal range in a healthy person. And some diseases may not affect your well-being for a long time, and then a preventive test will become a reason for subsequent examination.
- When the first symptoms of illness appear. Analysis in this case can make it possible to determine the nature of the disease, the degree of intensity of inflammation or an allergic reaction.
- OAC may be re-prescribed to monitor the course of the disease over time. Also to assess the effectiveness of the therapy.
Monocytes
Monocytes are cells of the immune system that are among the first to respond to the penetration of aggressors into the body. If the forces of local immunity could not contain the attack of bacteria, fungi or viruses, then it is monocytes that are the first to rush to protect health.
Monocytes are formed in the red bone marrow and released into the blood. There they begin to actively function, but this does not last long, only 2-3 days. Then, using their ability to move, they move beyond the vessels through special small pores between the cells and penetrate into the tissue. There, monocytes slightly change their structure and turn into macrophages - more effective phagocytes.
Functions of white cells
Lymphocytes. T lymphocytes destroy foreign microorganisms and cancer cells. B lymphocytes are responsible for producing antibodies.
Monocytes. They participate in phagocytosis, directly neutralizing foreign bodies, as well as the immune response and tissue regeneration.
Eosinophils. Capable of active movement and phagocytosis. They actively participate in the formation of inflammatory and allergic reactions, capturing and releasing histamine.
Basophils. They ensure the migration of other types of leukocytes into tissues to the site of inflammation and take part in allergic reactions.
Neutrophils. The main purpose is phagocytic protection, that is, the absorption of foreign bodies. In addition, they release bactericidal substances.
Eosinophils
Eosinophils are a small number of white blood cells that are found in human blood and tissues. They are an indispensable element that provides immunity.
Like other white blood cells, they are formed from bone marrow, and their progenitor is a single stem cell. The norm is 1–4%.
In total, eosinophils live about 12 days, but do not spend all of this time in the bloodstream. After 3-4 days of ripening, they enter the bloodstream and remain there for only 6-12 hours. Then they pass into the tissues and accumulate in especially large quantities in the lungs, under the mucous membrane of the digestive tract, and in the skin.
When the number of eosinophils increases, the condition is called eosinophilia, and the reverse change is called eosinopenia. As a rule, bright changes are symptoms of diseases, but some physiological fluctuations in their number are possible within normal limits. For example, an increase and decrease in eosinophils can be observed depending on the time of day; at night they are usually most in the blood.
Red blood cells
Erythrocytes, or red blood cells, ensure the delivery of oxygen to all cells of the body. In English-language literature, red blood cells are called “red blood cells,” which is where the international abbreviation RBC .
To transport oxygen, these cells contain hemoglobin, which can combine with it through chemical reactions. The analyzer displays the following indicators regarding these processes:
- RBC is the number of red blood cells per liter of blood. An increase in this indicator in humans can be observed with various neoplasms, hormonal disorders, but much more often it is the result of blood thickening due to dehydration, burns, taking diuretics and some other reasons. A decrease in RBC is observed with blood loss, anemia, disorders of their formation or increased destruction. A slight decrease in the number of red blood cells during pregnancy is normal.
- HGB - total hemoglobin content. The indicator grows following an increase in RBC and decreases for the same reasons. A decrease in HGB is also observed during hemodilution—blood dilution, for example, against the background of intensive intravenous administration of a large volume of solutions. Hemoglobin levels in women are usually lower than in men due to physiological blood loss during menstruation.
- HCT - hematocrit. This is a value that reflects the ratio of all blood cells to its liquid part - plasma. Since 99% of these cells are red blood cells, the indicator is used to estimate their volume.
Red blood cell indices
In addition, the so-called erythrocyte indices are assessed:
- MCV - average erythrocyte volume. Before the introduction of new analyzers, an accurate assessment was not carried out, and the result was designated as microcytosis, normocytosis or macrocytosis - depending on the size of the cells. An increased level of MCV may indicate a deficiency of vitamin B12, folic acid, hemolytic anemia, a decreased level may indicate iron deficiency and sideroblastic anemia.
- MCH is the concentration of hemoglobin in one red blood cell. In older analyzers, for this purpose, the color indicator was assessed, which is 0.03 of the MCH.
- MCHC is the average hemoglobin concentration in the erythrocyte mass, which reflects the degree of saturation of RBC with hemoglobin. It is the most stable indicator and can serve as an indicator of a correctly performed analysis.
All of the above indicators are closely related to each other and are assessed as a whole. For example, bleeding is accompanied by the loss of a large number of red blood cells. Accordingly, the total hemoglobin content also decreases, but MCH may remain normal. With a disease such as iron deficiency anemia, a slight deficiency of red blood cells occurs with a decrease in hemoglobin and various changes in erythrocyte indices. It makes no sense to list all possible changes in the body related to the content of red blood cells, and the doctor deciphers the result based on knowledge of those processes in the body in various diseases.
A separate indicator associated with red blood cells is their sedimentation rate - ESR (in modern analyzers - ESR) . This is a completely non-specific indicator, an increase in which indicates some problems in the body that the doctor needs to look for. In some cases, for example during pregnancy, an increase in ESR is physiological and is considered normal.
Leukocyte blood count: interpretation of results
Increasing performance
An increase in neutrophils in the blood occurs during infectious diseases and during some specific patient conditions. For example, in acute infectious diseases, candidiasis, rheumatism, tumor processes, lead or mercury poisoning, during diabetes. Also, an increase in the number of neutrophils can be influenced by conditions not associated with diseases, for example: severe physical exertion, stressful situations, overheating or hypothermia.
An increase in the number of lymphocytes indicates the presence of an infectious disease, blood pathology, lead or arsenic poisoning. Some medications can affect the increase in lymphocytes.
A previous infectious disease affects the increase in monocytes. Monocytes increase in autoimmune diseases, in the presence of cancer, and during carbon and phosphorus poisoning.
An increase in eosinophils occurs in response to allergic reactions, when taking certain antibiotics, medications for tuberculosis and convulsive conditions. Parasitic infections, diseases of the skin and respiratory system, and the acute course of an infectious disease can also change the indicators.
Basophils in the blood increase during influenza, chickenpox, tuberculosis, allergic reactions, ulcerative colitis due to increased sensitivity to any food, and an increase may also indicate the presence of cancerous tumors in the body.
Decrease in indicators
If the number of neutrophils decreases, the doctor may suspect that the patient has an infectious disease, hypersensitivity to drugs, anemia and anaphylactic shock.
Lymphocytes decrease in conditions of immunodeficiency, acute inflammatory processes in the body, renal failure and systemic lupus erythematosus.
A decrease in monocytes occurs during oncohematological diseases, purulent infections and aplastic anemia, the use of certain drugs and in a state of severe shock.
The decrease in eosinophils is affected by severe purulent infection and heavy metal poisoning.
Pregnancy, severe stress and the period of ovulation can be a natural cause of a decrease in basophils. Pathological causes include infectious diseases and Cushing's syndrome.
Leukogram shift
Modern automatic blood analyzers quickly and accurately calculate the complete leukocyte formula, which greatly facilitates diagnosis
When the leukogram is deciphered, nuclear shifts are taken into account. These are changes in the ratio of mature and immature neutrophils. In the blood formula, the different forms of neutrophils are listed in order from young to mature (from left to right).
There are three types of shifts: left, left with rejuvenation, and right.
With a left shift, myelocytes and metamyelocytes are present in the blood. This change occurs through the following processes:
- acute inflammation: pyelonephritis, prostatitis, orchitis;
- purulent infections;
- acidosis;
- bleeding is acute;
- poisoning with toxins;
- high physical activity.
With a left shift with rejuvenation, forms such as myelocytes, metamyelocytes, promyelocytes, myeloblasts, and erythroblasts can be found in the blood. This is observed in conditions such as:
- leukemia (chronic, acute);
- erythroleukemia;
- metastases;
- myelofibrosis;
- coma.
Video about the types and functions of leukocytes:
With a decrease in the number of band (immature) neutrophils and an increase in the level of segmented (mature forms containing 5-6 segments), they speak of a right shift. With such a change in the leukogram, we can talk about the following pathologies and conditions:
- liver and kidney diseases;
- megaloblastic anemia;
- consequences of blood transfusion;
- radiation sickness;
- vitamin B12 deficiency, folate deficiency anemia.
The degree of shift is assessed using a special index, which is determined by the ratio of the total number of all young neutrophils (myelocytes, metamyelocytes, promyelocytes, band neutrophils) to mature segmented ones. The norms for healthy adults are in the range of 0.05-0.1.
What does a shift in the leukocyte formula to the left and to the right mean?
Neutrophils form the body's antibacterial and antifungal defenses, and when a certain microbe enters the body, the number of neutrophils increases. In this case, not only their total number changes, but also the number of individual forms of these cells.
Chain of neutrophils arranged according to maturation:
Young - rod-nuclear - segmented.
A shift of the formula to the left is an increase in the number of young cells, and a shift to the right is an increase in the number of old cells.
Reasons for the shift in leukocyte formula
In medical practice, a shift to the left occurs more often. This is affected by the presence of an acute bacterial or fungal infection in the body. The bone marrow is mobilized to protect the body and begins to intensively produce neutrophils. They begin to fight the infection and die in the process. Young cells are produced to replace mature cells. At a certain point, the number of young cells exceeds the number of mature ones.
An increase in segmented neutrophils leads to a shift in the leukocyte count to the right. This occurs not only against the background of an increase, but even more often with a decrease in the number of leukocytes. This is facilitated by long-term chronic infections, in which bone marrow reserves are depleted and young cell forms cease to form. Poisoning, radiation, chemotherapy and radiotherapy, which also suppress the bone marrow, can cause the correct shift.
To prevent changes in the number of leukocytes and changes in the leukocyte formula, you need to monitor your health. To maintain your immune system, you should exercise, maintain a work-rest schedule, eat right, and avoid stressful situations. Also, do not forget about undergoing a routine examination with a therapist.
How to determine
The leukocyte formula is calculated by a laboratory assistant by viewing the blood under a microscope (leukogram count per hundred cells).
In addition, a hematology automatic analyzer is used. In case of deviations from the norm, a microscopic examination of the smear is additionally carried out, while the morphology of the cells is described and the leukogram is clarified.
The use of automatic equipment allows you to obtain the most accurate result: more than 2000 cells can be analyzed, while under a microscope - a maximum of 200. When examined using an analyzer, the result is more objective.
Automatic counting also has a drawback: the inability to divide neutrophils into segmented and band neutrophils. But in the case of a large number of young forms, the equipment records a shift to the left.
Why basophils may be elevated
Basophilia is diagnosed when the number of cells exceeds 0.2*109 /l. The use of drugs with estrogen hormones, as well as the use of thyreostatic drugs, can distort the picture. An increase in the rate is observed at the beginning of the menstrual cycle in women.
Basophils are increased:
- for chronic diseases of the gastrointestinal tract: inflammation of the gastric mucosa, enterocolitis, ulcerative inflammation of the large intestine, ulcerative lesions of the stomach and duodenum;
- at the stage of weakening of acute symptoms of an infectious disease;
- for blood diseases: acute form of leukemia, chronic myeloid leukemia, anemia, polycythemia, hemophilia, lymphogranulomatosis;
- for allergies and diabetes;
- with a decrease in the hormonal activity of the thyroid gland - hypothyroidism;
- oncology of the lymphatic system, blood cancer, lung cancer;
- due to prolonged exposure to low doses of radiation.
The main reasons for the increase in the indicator are a violation of immune defense and active invasion of the pathogen. In an adult, basophils may be elevated after removal of the spleen.
A child's concentration may increase:
- due to taking medications that cause allergies;
- due to a hidden inflammatory process;
- due to a recent vaccination or mosquito bite that gives rise to allergies;
- due to the introduction of foreign proteins.
To exclude pathology, a repeat analysis is recommended a week after the cessation of the above reasons. If the indicators are high again, a comprehensive examination is prescribed to identify the exact cause.
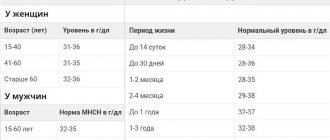
Normal indicators
The blood test form contains two indicators: relative, which shows the proportion of cells in the total number of leukocytes (BA%) and absolute, showing the number of basophils (BA#).
Each laboratory indicates its own normal ranges on the form, since indicators differ among clinics due to the specific equipment used for laboratory tests.
The number of basophils does not depend on gender, age, or time of day. Normally, the relative indicator is: 0-1%, absolute: 0-0.09*109/l. The absolute value gives a more complete picture of health. Sometimes it may be necessary to manually determine cell counts under a microscope.
The interpretation of the tests is carried out by the doctor as a whole, so based on only one indicator it is impossible to establish an accurate diagnosis.