Prevalence of the disease
In the world, those diagnosed with chronic venous insufficiency in different countries range from 15 to 25%, depending on the development of medicine in the country. In Russia, symptoms of CVI are observed in every second person aged 20–50 years, of which up to 15% have an established diagnosis, and 4% suffer from a severe form of the disease with complications in the form of trophic ulcers.
Chronic venous insufficiency is caused by upright posture, as a result of excessive stress on the legs. The impetus for its development can be congenital and acquired pathological conditions, injuries and prolonged physical activity. CVI is not always accompanied by visible changes in the veins; in most cases (mild form) it is a feeling of heaviness in the legs, swelling in the evenings, increased fatigue, pain when forced to stand for long periods of time.
Diagnostics
Based on the examination results, the specialist prescribes treatment for blood vessels and veins. The doctor examines the patient, inquires about symptoms and complaints. If there is doubt about the diagnosis, the patient is referred to procedures such as:
- Obstruction of venous outflow of the brain in children
- Magnetic resonance imaging.
- Ultrasound examination of cerebral vessels.
- CT scan.
- Angiography of cerebral vessels.
These examinations help to establish the root cause of the disturbance in the venous outflow of blood in the brain area.
If, as a result of the examination, the patient is found to have abnormalities in the area of the jugular vein, this can cause pronounced symptoms that provoke discomfort, the development of other diseases, and the occurrence of pathologies of the brain and venous outflow. During diagnosis, the eyeball must be examined, as blood stagnation may occur there.
In most cases, the disease (venous drainage of the brain) is accompanied by venous expansion in the legs, so complex treatment is carried out. The patient is prescribed medications and various exercises.
Causes of CVI
Most often, venous insufficiency occurs with varicose veins, as well as against the background of such diseases and pathological conditions as:
- congenital pathology of the venous system;
- congenital aplasia and hypoaplasia of the deep veins;
- congenital arteriovenous fistulas;
- congenital osteohypertrophic nevus with varicose veins;
- suffered acute thrombosis of the main veins;
- Klippel-Trenaunay syndrome;
- previous phlebothrombosis.
In recent years, a new cause for the development of chronic venous insufficiency has emerged, which is increasingly being identified - phlebopathy. This name refers to the state of venous stagnation in the absence of clinical signs of pathology. In rare cases, CVI begins to develop after a trauma (bruise, rupture, deep burns or hypothermia).
Main symptoms
What are the symptoms of vascular malformation? Vascular malformations can cause a variety of symptoms depending on their location in the body: A common symptom of all malformations is pain. Venous and lymphatic defects can cause subcutaneous swelling, over which the mole may be located. Skin lesions may ooze lymph or cause bleeding. Lymphatic malformations are usually complicated by an infectious process, requiring treatment with antibacterial drugs. Venolymphatic malformations may be associated with a phenomenon called Klippel-Trenaunay syndrome.
Arteriovenous malformations (AVMs) can also cause pain. They are the most dangerous due to the rapid discharge of blood from the arteries into the veins. Depending on their location, they can also lead to bleeding (eg from the uterus, bladder). Pulmonary arteriovenous malformations are somewhat different in that they act as a shunt that drains blood from the right side of the heart to the left side of the heart without increasing the level of oxygen in the lungs. This leads to symptoms of low oxygen, shortness of breath, and fatigue. Such defects can bleed, resulting in hemoptysis or hemothorax (the appearance of blood in the chest). Additionally, this abnormality can allow blood clots to pass through the lungs and into other arteries in the person's body, thereby causing a stroke or brain abscess. This is an essential reason for immediate treatment of pulmonary arteriovenous malformations.
The mechanism of the onset and development of the disease
Under the influence of gravity, the blood in the vessels descends to the lower extremities, the body has to make efforts to lift it. Venous valves prevent blood from flowing downwards, which are actively helped in this by physical activity, muscle contraction and bending of the knees. The combination of these factors ensures normal blood flow.
Maintaining a constant resistance to gravity is possible due to physiological changes in the lumen of blood vessels when changing body position, the operation of the valve apparatus and the tone (elasticity) of the venous wall. If one of these component mechanisms is disrupted, pathological processes begin to affect the entire system as a whole. Loss of elasticity of the section of the vein below the valve, and its expansion leads to valvular incompetence, the inability to maintain blood flow for subsequent rise. Stagnation of fluid leads to increased pressure to move blood upward. But, over time, increased pressure increases the volume of the part of the vein that has lost its elasticity.
Venous reflux (reverse flow of blood from top to bottom) can join the pathological process. The liquid begins to stagnate and put pressure on the walls of the vessel. As a result, blood plasma leaks into the surrounding tissue, causing swelling. The situation develops similarly with initial valvular insufficiency.
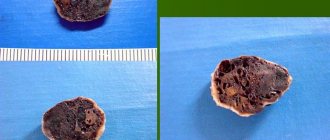
Simultaneously with circulatory failure, the lymphatic system is also overloaded. Trophic disorders contribute to the formation of trophic ulcers. Trophic ulcers are long-term non-healing wounds (6 months or more) affecting the skin and tissues. They form on the lower leg, are surrounded by an area of inflammation, and have a high risk of infection.
How to improve venous drainage of the brain
To improve venous outflow from the brain when it is dysfunctional, medications (Actovegin, Detralex), neck exercises, massage, diet with limited salt and sufficient intake of dietary fiber, medicinal plants, leeches, and physiotherapy are used. It is important to monitor working conditions.
Treatment with drugs
To treat circulatory disorders in the veins of the brain, drugs from the following groups are used:
Exercises
For dysfunctional venous congestion, a set of exercises for the neck is useful ; it can be done even at your desk:
- lowering your shoulders down, try to reach the top of your head towards the ceiling, relax and repeat 10 times;
- tilting the head to the shoulder, while trying not to bend the neck, but stretching it as far as possible to the side (10 times to the right and left);
- pushing the chin forward (snake head) and pulling the back of the head back with a delay of 10 counts in each final position;
- turning the head to the sides with the shoulders lowered as much as possible (10 repetitions each);
- pull your shoulders towards your ears, and then with a sharp movement throw them down 10 times.
Expert opinion Alena ArikoExpert in the field of cardiology With venous dysfunction of the brain, headstand exercises, heavy lifting, and hanging on rings are contraindicated. All movements should be smooth, without jerking.
- Hemorrhagic cerebral stroke: what it is, symptoms and consequences
Massage
Massage of the cervical-collar area is considered effective to improve venous outflow. It is better if it is carried out by a specialist, but to relieve headaches and heaviness in the head, several techniques can be done independently:
- use your fingers to move in the direction from the forehead to the neck with intense pressure on the skin 3 times, as if moving it back;
- perform stroking from the back of the head to the shoulders (from the center to the sides) 5 times;
- stretch and knead the back of the neck from top to bottom (3 times) and from the center to the sides (3 times);
- tap with the tips of 4 fingers from the crown to the back of the head and along the shoulders;
- repeat the first movement, but without effort.
Nutrition
It is necessary to exclude from the diet foods that retain fluid in the body:
- pickles,
- marinades,
- smoking,
- sausages,
- hot sauces,
- fried foods.
Table salt is limited to 5 g per day. This means that you need to cook without it, and add salt to the already prepared dish. It is useful to replace the table with pink Himalayan. To improve blood flow, the diet should include:
- proteins – low-fat dairy, meat and fish products;
- vegetables with coarse fiber - cabbage, pumpkin, beets, fresh salads;
- black bread, bran;
- fruits, berries;
- dried fruits – prunes, dried apricots;
- drinking water – no more than 1.5 liters, it should be drunk in small portions.
If you are prone to constipation, kefir or fresh yogurt is recommended before bed; it is better to prepare them at home using pharmacy starters.
To enhance the laxative effect, an hour before taking, you can add a mixture of a teaspoon of bran and 4 prunes (they are pre-steamed with boiling water for 30 minutes).
Traditional methods
To treat venous dysfunction in the brain, a collection of herbs is used:
- crushed chestnut fruits 50 g,
- raspberry leaf 20 g,
- peony flowers 20 g,
- horsetail herb 10 g.
A tablespoon of the mixture is poured into a glass of boiling water and cooked in a water bath for 30 minutes, and then left for 1.5 hours. After straining, take 50 ml half an hour before meals 4 times a day for 45 days. After a 15-day break, the course can be repeated.
Hirudotherapy
For cyanotic skin and severe venous stagnation, hirudotherapy is used - leeches are placed on the occipital and retroauricular area. Prescribe 5-7 sessions 2 times a week. The secretion of the salivary glands of leeches contains hirudin, which:
- reduces blood viscosity;
- improves nutrition of brain cells;
- reduces swelling;
- accelerates the movement of blood through veins and arteries;
- relieves pain.
Physiotherapy
To treat dysfunction of the venous outflow in the brain, the following is used:
- phonophoresis (ultrasonic injection) of Troxevasin ointment on the collar area;
- galvanic collar;
- laser and magnetic therapy;
- hydrogen sulfide, carbon dioxide baths.
The high effectiveness of sanatorium-resort treatment has been proven, since physical and climatic conditions are used simultaneously.
Risk factors for CVI
A number of factors significantly increase the risk of developing chronic venous insufficiency, these include:
- Genetic predisposition, including pathologies of connective tissue and weakness of the vascular wall.
- Taking hormone-containing drugs, including hormonal contraceptives.
- Low physical activity, sedentary lifestyle, constant heavy lifting, excess weight.
- Chronic constipation.
CVI is more often diagnosed in women, since the formation of venous insufficiency is influenced by a high concentration of estrogens (female steroid sex hormones). The period of pregnancy and childbirth and the use of hormonal contraceptives have a negative impact. With age, the likelihood of developing the disease increases in both sexes due to prolonged exposure to adverse factors.
Classification of CVI
- 1st degree:
is expressed in a feeling of heaviness, aching pain, passing, minor swelling and night cramps.
- 2nd degree:
persistent swelling, hyperpigmentation (darkening of the skin of the affected limb), lipodermatosclerosis (dystrophic changes in fatty tissue), dry and weeping eczema (serous inflammation of the dermis).
- 3rd degree:
To the above signs of stage 2, trophic ulcers, current or already healed, are added.
- There is also 0 degree
when the patient does not observe changes, there are no complaints, however, the pathological processes have already started. The treatment method for patients with zero degree CVI differs from the treatment of patients at other stages.
In international practice, chronic venous insufficiency is divided into 6 degrees according to clinical manifestations, including zero (CEAP system). The disease also has an etiological classification based on its causes:
- EC is a congenital pathology.
- ES is an acquired form as a result of thrombosis, varicose veins, or trauma.
- EP is an unclear cause of venous insufficiency.
There is also an anatomical classification based on location, taking into account pathophysiology, disability scale and a number of other factors.
Origin of vascular malformations
Malformations occur in the prenatal period. Geneticists are conducting a lot of research to study this phenomenon, but have not yet come to a definite concept. Therefore, the question of the causes of malformations remains not fully understood.
Congenital angiodysplasia (Parks-Weber-Rubashov syndrome) is characterized by the presence of pathological anastomosis (fistulas) between arteries and veins.
Arteriovenous anastomoses are often multiple and have a variety of sizes and shapes. Depending on the diameter, a distinction is made between macrofistulas, visible to the naked eye, and microfistulas, which are detected only by microscopic examination of the tissues of the limb.
The causes of the development of Parkes-Weber-Rubashov syndrome have not been definitively established. A number of authors consider it to be the result of mutations in the RASA1 gene, which encodes the p120-RasGAP protein, which is involved in the transmission of chemical signals from the extracellular space to the cell nucleus. However, exactly how these changes lead to specific vascular abnormalities in individuals with Parkes-Weber-Rubashov syndrome has not been established.
Pathological anastomosis are most often located in the area of the femoral, branches of the popliteal artery, as well as along the tibial arteries. Intensive discharge of arterial blood through arteriovenous fistulas leads to an increase in blood pressure in the veins.
Due to the increased functional load, the histological structure of the venous wall changes. There is a thickening of its muscular membrane and the formation of an internal elastic membrane (“arterialization” of the vein).
In the presence of fistulas, a significant part of the arterial blood enters the venous bed, bypassing the capillary network, so severe oxygen starvation occurs in the tissues and metabolic processes are disrupted. Due to venous hypertension, the load on the heart increases, which gradually leads to expansion of its boundaries and cardiac decompensation.
Symptoms of chronic venous insufficiency
At an early stage, chronic venous insufficiency has a broad clinical picture, expressed in one symptom, followed by a chaotic addition of other manifestations. As a rule, they appear or intensify after long periods of sitting or standing, as well as during periods of increased physical activity:
- heaviness in the legs;
- fatigue, buzzing;
- aching pain;
- transient swelling;
- numbness, temporary loss of sensation;
- cramps that occur at night.
If you regularly experience at least one of these symptoms, you should consult a doctor. Subsequently, with the development of pathology, pigmentation of the skin of the lower leg will occur, the skin will lose elasticity and become dry.
As it progresses (stages 2 and 3), symptoms such as:
- persistent swelling;
- increased pain during exercise;
- formation of ulcers and eczema;
- phlebeurysm.
Lack of blood circulation negatively affects not only the affected area, but also the entire body as a whole. Dizziness and fainting, high mental and physical fatigue may occur. Signs of heart failure are also noted: heart rhythm disturbances, pale skin, shortness of breath.
Treatment methods
Depending on the speed of the disease and the patient’s well-being, the following treatment methods may be prescribed:
- Medicines;
- physiotherapy;
- massage of the collar area and back;
- physical therapy (physical therapy);
- acupuncture;
- special diet.
Treatment is carried out using one of the listed methods, or in combination.
Drug therapy
Drug therapy is based on the patient taking venotonic drugs. They help improve blood circulation. The doctor prescribes drugs such as: Detralex, Tanakan, Vinpocetine, Asniton, Phezam. Diuretics may also be prescribed to relieve swelling in the face and neck.
ATTENTION! The drugs are selected individually and strictly as prescribed by the doctor.
Physiotherapy
In addition to taking medications, physical therapy can help you feel better. A general practitioner or neurologist may prescribe:
- Electrophoresis;
- Valerian masks;
- Magnetotherapy;
- Laser therapy;
- Electrical stimulation.
The effectiveness of physiotherapy has been tested for decades, and compared to medicinal treatments, it is a more “gentle” method.
- What to do and how to recognize impaired venous outflow with cervical osteochondrosis?
Medication and physical therapy can be prescribed in combination.
Massage
Massage of the collar zone is prescribed to a patient with venous stagnation quite often. Massage is prescribed only in the absence of acute inflammation , otherwise this procedure can become extremely painful and harm the patient’s health.
Massage helps improve blood circulation, relieve muscle tension, and eliminate pain. It is advisable that the procedure be performed by an experienced massage therapist or chiropractor. The massage course lasts no more than 10 days.
Self-massage is also possible, 2-3 times a day: light stroking in the direction from the base of the neck to the head. Circular movements are also made from bottom to top to improve blood flow.
Exercise therapy: effective exercises
Therapeutic exercise is prescribed to a patient if there is a violation of the outflow in the brain, if there are no other contraindications and acute pain symptoms are relieved with the help of medications. Exercise therapy is aimed at strengthening the neck muscles and is initially performed in a sitting position to avoid dizziness and fainting.
Effective exercises to improve blood flow include:
- Smooth circular rotations of the head;
- tilts back and forth, left and right;
- turns the head and neck left and right.
REFERENCE. A course of exercise therapy can be taken at a specialized medical center, where a physical therapy doctor will select the necessary set of exercises, because to improve well-being it is necessary to strengthen the entire body as a whole.
Treatment of vertebrogenic causes
Vertebrogenic headache (cervicocranialgia) is associated with the presence of SCH. The muscles of the neck and back are subject to tension and therefore pain occurs.
The causes of vertebrogenic headaches can be severe physical exertion, injuries to the back muscles, and as a result, protrusions, prolapses or hernias in the intervertebral discs.
- Venous discirculation of the brain
The main symptom of vertebrogenic headaches is a noticeable limitation of movements of the head or neck, as well as pain that occurs when palpating areas of the neck.
Treatment is achieved with medications, and after acute symptoms are relieved using the above methods of restorative treatment.
Self-medication for cervicocranialgia is unacceptable!
The course of therapy is prescribed by a neurologist or vertebrologist.
IMPORTANT INFORMATION! Massage for cervicocranialgia can lead to a deterioration in well-being and is prescribed only at the rehabilitation stage.
Diagnosis and treatment of CVI
At an appointment with a phlebologist at the Ambulatory Surgery Center, the patient is diagnosed based on the medical history, the patient’s complaints, and the results of the study. The main method of instrumental examination is duplex ultrasound scanning. In our clinic, functional diagnostic doctors during the study not only confirm the presence of CVI, but also help surgeons determine the extent of damage to the venous system and the choice of tactics for further action. In some cases, the attending physician may prescribe a duplex angioscan or X-ray contrast study (phlebography).
Treatment of chronic venous insufficiency is a set of measures, the purpose of which is to restore the functionality of the venous and lymphatic systems, eliminate the pathologies that arise from them and prevent relapses. The method of therapy is selected individually for each patient, taking into account the degree of pathological changes, medical history, age and concomitant diseases.
Conservative treatment
A course of treatment is prescribed, lasting on average 2 - 3 months, then after a certain period it is resumed. The course usually includes:
- medicines (phlebotrobic drugs);
- local use of antiseptic ointments;
- corticosteroid drugs;
- elastic compression (bandages and compression hosiery);
- treatment of associated secondary infections;
- elevated position of the legs when lying down.
In some cases, antibiotics and diuretics are prescribed to reduce swelling. The greatest role in the routine treatment of CVI is played by elastic compression, including hardware, pneumatic, and leg elevation. Compression is indicated for all patients, even those with ulcers. In this case, I use elastic bandaging, and then wear special stockings. They should create a distal pressure of 20–30 mm Hg. for patients of the first stage, 30–40 mm Hg. – second and up to 60 mm Hg. at the third.
The effectiveness of therapy directly depends on the active participation of the patient. He needs to strictly follow the doctor’s recommendations and build his life in such a way that conditions that aggravate the course of the disease are not created.
Surgery
Surgery is performed only in 10% of patients with:
- severe concomitant diseases;
- trophic disorders;
- transformed tributaries of the great (small) saphenous veins;
- relapse of varicose veins and in other similar cases.
For this purpose, a minimally invasive surgery technique is chosen - miniphlebectomy.
. The operation is performed under local anesthesia. Through small punctures, the vascular surgeon gains access to the affected areas of the veins to perform ligation (vessel ligation), vein removal, and valve reconstruction. The tasks of a vascular surgeon include eliminating pathological blood discharge and truncation of varicose veins. After the operation, an hour later, the patient can go home; a hospital stay is not required.
Problems of venous insufficiency in infants
Institute of Correctional Pedagogy RAO, Moscow. The clinical method of neurological examination in combination with diagnostic methods ensures the correct diagnosis. The clinical picture of various forms of vascular diseases of the brain is largely determined by dysfunction of the venous circulation, and often the course and outcome of the disease depend specifically on venous disorders, so their identification is of theoretical and practical importance. The venous system of the head is anatomically complex; the extracranial venous network, diploic veins, sinuses and veins of the dura mater, which have many anastomoses, take part in its formation.
Among perinatal pathologies, hypertensive-hydrocephalic syndrome occupies one of the first places. Symptoms of increased intracranial pressure and expansion of the cerebrospinal fluid spaces of the brain reflect ischemic - hypoxic, traumatic brain damage in the intra- and perinatal period / B.V. Lebedev, L.M. Kuzenkova, O.I. Maslova, 1990/.
Manifestations of intracranial hypertension in infancy are often hidden, which is explained by the presence of well-developed adaptation mechanisms in children. Intracranial pressure is determined not so much by the form of hydrocephalus as by the stage of development of the disease /P. Wiecka, Chr. Tsekov, 1982/. Patients often develop a violation of venous outflow. Liquor, intraventricular hypertension is not an obligatory component of intracranial hypertension syndrome. The cerebrospinal fluid pressure continuously changes depending on the degree of preservation of the adaptation mechanisms of the brain due to an imbalance between the individual components of the intracranial fluid volume.
The term “benign” intracranial hypertension (pseudotumor cerebri) is used in modern literature to designate a syndrome of increased intracranial pressure in the absence of a massive cerebral process. Children complain of headaches / no history of head injuries or inflammatory diseases of the nervous system /, blurred vision, and oculomotor disorders. Analgesics do not relieve pain. A positive effect of dehydration therapy was noted /E.M. Burtsev, E.V. Maletskaya, 1997/.
Echoencephalography /ECHOEG/ is a method for diagnosing intracranial lesions using ultrasound. The use of ECHOEG has no contraindications, provides high accuracy, and has a number of differential diagnostic capabilities (including the detection of hypertensive-hydrocephalic syndrome). Over the past three years /1996-1998/ at the Consultative and Diagnostic Center of the IKP RAO and the city children's clinic N34 in Moscow / chief physician L.K. Drozdova / we examined 63 infants aged from 2 months to 2 years /27 girls and 36 boys/.
Most patients were diagnosed with “hypertensive-hydrocephalic syndrome”, “intracranial hypertension”, “neurotic reactions”. Mothers often experienced pathologies during pregnancy: threat of miscarriage, toxicosis in the second half of pregnancy. Labor was quick or protracted, with many having a caesarean section. Premature babies (7-8 months) were more often boys. From the complaints of parents: poor / short / sleep of infants, hyperactivity, crying, neurotic reactions, enlarged head size, delays in physical and mental development (underdevelopment of speech by 2 years).
EchoEG was performed using an EES-12 echoencephalograph. The degree of intracranial hypertension was determined by determining the width of the third ventricle, the severity of the number and amplitude of lateral echo signals, and M-ECA pulsations. Additional pathological signs are shifts in lateral echo signals. As the lateral ventricles expand, echoes from the medial walls shift medially, and echoes from the lateral walls shift laterally. The cerebral cape index was calculated. IMP=a/b, where a is the distance from the M-echo to the final complex; b — distance from the echo of the lateral ventricle to the terminal complex. Indexes > 2.3 / L.R. are considered pathological. Zenkov, M.A. Ronkin, 1991/.
I group of infants from 2 months. up to 12 months / n=23; 16 boys and 6 girls/.
In ECHOEG there are significant displacements/shifts of +0.5 mm. were not taken into account/no midline brain structures were identified: Md=58.4 mm; Ms=58.4 mm. /from 50 to 66 mm./. All of them had a split echo, which is typical for children. The width of the third ventricle of all children corresponded to the age norm /5 mm/, except for two boys in whom the width was increased by 1 mm. /6 mm./.
In the majority of infants /70%/ lateral echo signals were pronounced in number and amplitude, in the rest - moderately pronounced. Pulsations of echo signals in a third of patients were pronounced, over 50% (in two - over 60%), in the rest - up to 50% (normal limit). UTI was significantly increased in 80% of those examined and averaged: UTIs=3.1+0.1; IMPd=3.0+0.1 / from 2.9 to 4.0; worse left. For the rest, UTI = 2.7 + 0.1 / from 2.6 to 2.8/, with the norm <2.3. In three children (diagnosed with “neurotic reactions”), ECHOEG was a variant of the age norm: lateral echo signals were moderate in number and amplitude, M-echo pulsations up to 40%, IMP = 2.3, width of the third ventricle = 5 mm. Group II of infants from 1 to 2 years old/n=41; 21 boys and 20 girls.
ECHOEG did not reveal any significant displacements of the midline brain structures: Md=66.3 mm; Ms=66.3 mm /from 62 to 72 mm/. Everyone's echo was split. The width of the third ventricle in a third of patients was increased by 1 mm. compared to the norm and amounted to 6 mm. In the remaining children this value was normal /5 mm/.
In the majority of infants /80%/ lateral echo signals were pronounced in number and amplitude, in the rest - moderately pronounced. The pulsations of echo signals in most patients were up to 50% /normal limit/, in one - over 50%; two have over 60%. UTI was significantly increased in 75% of those examined and averaged: UTIs=3.0+0.1; IMPd=2.9 / from 2.8 to 3.2; worse left. For the rest, IMP = 2.6 + 0.1 / from 2.5 to 2.7/.
In four examined children (diagnosed with “neurotic reactions”), ECHOEG was a variant of the age norm.
Thus, the majority of the examined children /up to 80%/ according to echocardiography had intracranial hypertension. Approximately 10% of the examined infants had an echocardiogram within the age norm and 10% had mild signs of intracranial hypertension.
Dehydration therapy gave positive dynamics, especially immediately after the course of treatment. However, after 3-6 months, signs of intracranial hypertension often appeared.
From the age of three, some children (especially during repeated examinations) underwent ECHOEG and REG (rheoencephalogram). Obstruction of venous outflow is manifested on REG by the convexity of the descending part of the wave (catacrote). The incisura and additional waves give a “jagged” appearance – “cockscomb” combs. Signs of obstruction of venous outflow were often detected against the background of not sufficient (preserved) but decreased pulse blood filling of the cerebral vessels. V.V. Shtok, M.A. Ronkin, V.L. Anzimirov (1996) define these changes as types of venous insufficiency of the second and third degrees. An increase in the number and amplitude of lateral echo signals was recorded on ECHOEG.
Thus:
- The ECHOEG and REG methods are quite informative for assessing the liquor-venous circulation in infants.
- The study showed that boys tolerate prenatal, natal and postnatal pathologies worse, “mature” more slowly, and are more often exposed to injuries compared to girls.
- Dehydration therapy (except for acute conditions) should be used in gentle doses, taking into account the individual characteristics of infants.