Reasons for the development of pathology
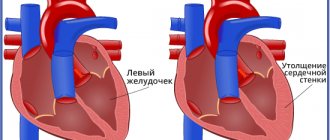
An enlarged heart in an adult is also called myocardial hypertrophy syndrome. Occurring against the background of an underlying cardiac disease, this condition can aggravate the overall clinical picture and worsen the prognosis of the underlying pathology. Enlargement of the right ventricle of the heart is less common than the left; in rare cases, there are changes in the size of both ventricles. According to statistics, against the background of concomitant cardiac pathologies, myocardial hypertrophy leads to mortality in 75-80% of cases. Therefore, timely detection and treatment of diseases of the cardiovascular system will be the key to a stable state of health.
The average heart weight in adult men is about 330 grams, in women - about 250 grams; to determine the external size of your own heart, just look at your clenched fist - the volume of the heart is about the same.
This pathology can be detected both in childhood and in adulthood. Athletes are susceptible to myocardial hypertrophy, since during active training the heart is subjected to an inappropriately increasing load, actively pumping blood. The heart muscles become overstrained, an enlargement of the ventricle or even two occurs, and a state of myocardial hypertrophy occurs.
With coronary heart disease, reduced blood flow to the organ occurs. The cells of the main muscle do not receive sufficient nutrition, as a result of which they begin to actively contract, and the process of their degeneration into connective tissue begins. It no longer has the ability to stretch or contract, so only the cavities of the heart can be enlarged.
This phenomenon is most pronounced during myocardial infarction - a certain part of the muscle tissue of the wall becomes inactive, which leads to the formation of a scar in this place.
The most common factors leading to an increase in myocardial size are excessive stress on the heart during heavy physical work, too much activity during sports, bad habits, as well as concomitant pathologies of the cardiovascular system. To summarize, the main reasons can be identified:
- heart defects (both congenital, hereditary, and acquired during life);
- physical labor and various strenuous sports that place excessive stress on the heart;
- ischemia;
- arterial hypertension;
- abuse of tobacco products and alcoholic beverages;
- excess body weight;
- sudden, unexpected stress on the heart muscle, against the background of an inactive, sedentary lifestyle.
This condition may have a hereditary etiology, that is, transmitted through generations from relatives suffering from cardiovascular diseases. In the presence of such an acquired “inherited” disease as aortic stenosis, arterial hypertension, mitral valve stenosis, a large heart is not such a rare occurrence. Enlargement of the ventricle, or both, occurs under excessive loads, when the organ triggers a compensation mechanism in order to protect itself. As a result, the size of the myocardium is increased.
Carditis, rheumatic carditis are diseases of the heart, which can also lead to the fact that it becomes enlarged against the background of flabbiness of the myocardial muscles, while the ventricles grow in size, and the heart dilates transversely. There have been cases when such a hypertrophied organ occupied both sides of the chest.
Myocarditis is a heart pathology that occurs as a consequence of a severe viral infection. When the disease worsens, the patient feels shortness of breath, becomes lethargic, a picture of general malaise appears, and the heart beats at an accelerated pace. There is an enlargement of the right ventricle of the heart against the background of acute heart failure. This condition also causes myocardial hypertrophy.
Septic endocarditis is considered a dangerous disease because it occurs against the background of infection of the inner surface of the heart by the microbial environment. As a result of infection, the valves, muscles, and left and right ventricles undergo significant changes. The patient suffers from fever, aching joints, increased body temperature (which is often confused with cold symptoms), and the myocardium increases in size.
About the structure of the cardiovascular system
The heart is a unique organ on which human life depends. It works without rest, has its own control center, which sends electrical impulses that stimulate muscle contractility.
The structure of the heart is widely known: it has two ventricles and two atria. By contracting, they ensure blood circulation through two vascular systems: the small and large blood circles. To more accurately explain the characteristics of different types of heart failure, it is necessary to mention the characteristics of blood flow.
The systemic circulation involves the flow of blood from the left ventricle into the aorta, oxygenation of all important organs and limbs and the return of venous blood to the right atrium. The pulmonary circulation is the flow of blood from the right ventricle to the lungs and the movement of oxygenated blood into the left atrium.
Symptoms of heart failure depend on which part of the heart is affected. This is reflected in disruption of the functioning of blood circulation.
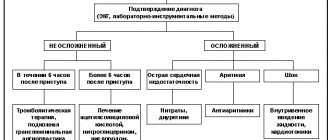
Heart failure, depending on the nature of its course, can be of two types. The chronic form develops over a long period of time and has several stages. Acute heart failure progresses rapidly. The duration of the process is from an hour to two days. This condition requires urgent hospitalization.
The classification of heart failure based on the localization of the pathology distinguishes several types:
- Left ventricular failure;
- Right ventricular failure
- Total form.
As the disease progresses, isolated variants lead to the formation of a general, total form of the lesion. Damage to the left ventricle causes disturbances in the systemic circulation. Pathology of the right ventricle - affects the lungs or pulmonary circulation.
Symptoms
Any manifestations of pathology may be absent for a long time, which is why this syndrome is considered very dangerous. The patient may not be aware that he has a large heart, as well as the reasons that caused this condition. Pathology can be detected on an X-ray, during a routine preventive examination, or in worst cases, during an autopsy after sudden death. Myocardial hypertrophy can be manifested by the following symptoms:
- Shortness of breath of unknown etiology, occurring both during physical exertion and at rest.
- Pain in the chest, similar to the symptoms of angina pectoris.
- Heart rhythm disturbances.
- Swelling of tissues, deterioration in the removal of fluid and salts from the body.
- Dizziness, fainting.
The listed symptoms should be the reason for a mandatory visit to a therapist, who, after a thorough examination and examination of the patient’s complaints, will send him to a cardiologist for examination.
Myocardial hypertrophy is diagnosed using ultrasound; it shows itself to be the most informative in terms of identifying cardiac pathologies.
If they are detected, it is recommended to conduct an ECG (recording of an electrocardiogram), and to clarify concomitant diseases, magnetic resonance imaging is recommended.
What to do with an enlarged heart?
The first thing that worries parents if an X-ray reveals an enlarged heart in a child is the measures that can be taken.
- First you need to pull yourself together and put aside panic. If the disease is detected by chance, and not by diagnosis based on specific complaints and symptoms, then the baby is clearly not suffering, the organ copes with its task normally.
- It is necessary to contact a cardiologist who will prescribe additional studies and diagnostics to confirm or refute the suspected diagnosis.
- Proceed with the intended treatment. The sooner this happens, the greater the chance of a favorable prognosis.
As for the treatment itself, it is prescribed individually, depending on the symptoms, the baby’s well-being, the severity and cause of the disease.
Consequences of the disease
In case of increased myocardial activity and its subsequent increase, it is necessary to be observed by an experienced cardiologist and undergo regular examination courses. An important part of drug therapy will be a review of your lifestyle. In particular, you need:
- Give up bad habits - alcohol and cigarette abuse.
- Get rid of obesity and extra pounds to reduce the load on the heart muscle.
- Reduce the amount of salted, smoked, cholesterol-rich foods you consume.
- Balance the diet, enrich it with microelements and substances to normalize heart function.
- Reduce inadequate stress on the heart.
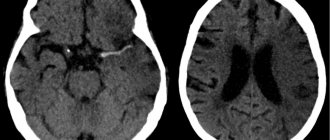
If measures are not taken to maintain the myocardium in a healthy state, this can lead to the development of stroke, heart attack, heart failure and even death.
People with alcohol addiction are at particular risk. Against the background of constant intoxication, the heart of a drinker sometimes reaches very large sizes. Restoration of myocardial size can only occur if alcohol is completely abstained.
Medicine offers modern drugs and treatment methods that, if used in a timely manner, will help reduce blood pressure, normalize blood flow to the myocardial muscle and return the heart to its original size. The main thing for successful treatment is to detect the pathology in time.
Who diagnoses the disease and how
As a rule, pathology is diagnosed randomly. An enlarged heart in a child is usually detected on x-ray. The resulting image clearly shows the increased size of the main vital organ.
Some changes can also be seen on a cardiogram or echocardiogram. At the same time, the little patients themselves do not experience any unpleasant sensations or discomfort. Such a diagnosis is made against the background of sports activity or other diseases.
If complaints arise and the doctor purposefully orders an X-ray diagnosis of an enlarged heart in a child, then the prognosis is usually unfavorable. This indicates a deterioration of the condition, a severe course of the disease, which in a complicated form can be fatal.
You can perform timely diagnostics at JSC “Medicine”. The clinic is located in the center of Moscow at the address: 2nd Tverskoy-Yamskaya Lane, 10. You can get to it from the metro stations: Mayakovskaya, Belorusskaya, Novoslobodskaya, Tverskaya, Chekhovskaya.
Modern methods of treatment
Treatment for pericarditis will depend on its underlying cause.
If it is a bacterial infection, antibiotics may be prescribed. In most cases, according to the American Heart Association, pericarditis is mild and goes away on its own - you just need to rest. But the doctor may prescribe non-steroidal anti-inflammatory drugs (Ibuprofen, Aspirin). If there are other medical risks, the patient may be hospitalized. In this case, therapy will be aimed at reducing pain, inflammation and minimizing the risk of relapse. As a rule, Colchicine is prescribed in this case.
Corticosteroids are also effective in reducing the symptoms of pericarditis, however, studies have shown that early use of these drugs may have an increased risk of recurrence of the disease and should be avoided except in extreme cases where the disease is refractory to conventional treatment.
Surgery may be considered for recurrent pericarditis that does not respond to other treatments, in which case the pericardium is removed.
Causes of pericarditis in adults
The cause of most pericarditis is unknown, but 80 to 90% of cases are thought to be associated with infections (viruses, bacteria, fungi, and parasites).
In addition, pericarditis can be caused by:
- cardiovascular problems (previous heart attack or surgery);
- injuries;
- radiation therapy;
- autoimmune diseases such as lupus;
- some medications, which is rare;
- metabolic disorders such as gout;
- renal failure;
- some genetic diseases, such as familial Mediterranean fever;
- cancer;
- some medications.
The mechanism of pathology formation
Chronic cardiovascular failure develops slowly due to the body's compensatory mechanisms.
At the compensatory stage of the myocardium, the heart muscle begins to hypertrophy. The vessels expand, causing their walls to become more fragile and permeable over time. Hormones are produced that change the composition of the blood, which becomes more liquid, its volume increases due to increased work of the bone marrow and an increase in the amount of water due to retention.
Compensatory possibilities dry up, and the decompensatory stage begins, which is characterized by a weakening of the functions of the entire cardiovascular system.
As the muscle mass of the myocardium grows, its small vessels lag behind in development, as a result, the heart muscle lacks oxygen and nutrients. Pathological changes occur: the proliferation of connective and sclerotic tissue. The heart becomes unable to pump the increasing volume of blood. Extensive oxygen starvation begins, which covers all organs.
Along with this, the walls of blood vessels become more fragile and permeable. Lymph leaks from the vessels. Swelling begins. These phenomena are especially dangerous in the lungs. They quickly fill with liquid and stretch. A person is tormented by a severe cough, and the discharge of sputum does not provide relief.
Diagnostics
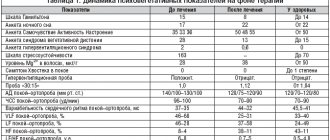
When collecting anamnesis, the doctor pays special attention to the presence of complaints of shortness of breath and fatigue. Collects information about the existence of other diseases. If heart failure is suspected, the patient is referred for instrumental studies and laboratory tests.
The Cardiology Center of the Federal Medical and Clinical Center of the Federal Medical and Biological Agency carries out a full range of diagnostic measures:
- ECG in 12 leads;
- ECHO-KG;
- Holter monitoring;
- ECG with dosed physical activity;
- transesophageal ECHO-CG;
- ABPM (24-hour blood pressure monitoring);
- Ultrasound of the abdominal organs;
- general blood analysis;
- biochemical blood test (lipid spectrum, blood glucose, liver and kidney function indicators);
- thyroid hormones;
- coagulogram (a test to determine blood clotting);
- general urine analysis;
- spirometry (respiratory function test);
What is pericarditis
Pericarditis is an inflammation of the pericardium, the thin, two-layered sac that surrounds the heart.
There is a small amount of liquid between the layers to prevent friction during beating. When the layers become inflamed, this can lead to disruption of the full functioning of the heart, the formation of adhesions in the cavity, fluid accumulation and chest pain. The pericardium also helps keep the heart inside the chest. Pericarditis usually occurs suddenly and lasts from several days to several weeks.
Anyone can get pericarditis. In most cases, it goes away on its own. However, 15 to 30% of people get it more than once—this is called recurrent pericarditis.
There are several forms of pericarditis:
- acute - it can occur on its own or as a symptom of an underlying disease;
- recurrent - can be periodic or constant, the first recurrence usually occurs within 18 - 20 months from the initial illness;
- chronic - in this case, relapse occurs immediately after treatment;
- delayed (Dressler syndrome) - it develops several weeks after heart surgery or a heart attack;
- constrictive - the pericardium scars or sticks to the heart so the heart muscle cannot expand (this form is rare and can develop in people with chronic pericarditis or after heart surgery);
- effusion-constrictive pericarditis - in this case, effusion (fluid) accumulates in the pericardium and a narrowing of the heart occurs.
One third of people with pericardial effusion develop cardiac tamponade, which requires emergency medical attention.