Bilirubin metabolism disorders
Erythrocytes - red blood cells - contain a complex protein called hemoglobin. It is necessary for the transport of oxygen through human tissues. Having served its term, it enters the liver, spleen, bone marrow, where it is destroyed. Among the breakdown products is indirect bilirubin, which is pathogenic for the body. Therefore, under the influence of other components, it goes through the next stage of transformation, and is released along with liver bile and leaves the body naturally.
If bilirubin is not neutralized, or the process does not affect most of the substance, it turns into biliverdin, an oxidation product. Increased levels lead to jaundice. In some cases, the skin may become greenish. This is due to the high concentration of direct bilirubin in the blood, since in this form it oxidizes faster.
Causes of hyperbilirubinemia
- Accelerated breakdown and/or shortening of red blood cell life.
- Impaired production of substances necessary for the breakdown of bilirubin.
- Decreased absorption of bilirubin by liver cells.
- Decreased excretion of pigment from the liver into bile.
- Obstructed outflow of bile and its penetration into the blood.
There are many causes of bilirubin metabolism disorders, including cholelithiasis, liver diseases, including cirrhosis, tumors and chronic hepatitis. Hyperbilirubinemia can also be caused by parasites that reduce the body’s ability to excrete bilirubin, exposure to toxic substances, anemia, etc.
Depending on the stage of disruption of the conversion and output process, an increase in the level of one of the fractions is diagnosed in the blood. If total bilirubin is high, this indicates liver disease. An increase in indirect bilirubin means excessive destruction of red blood cells or impaired transport of bilirubin. High level of direct - problems with the outflow of bile.
General information
The renewal of red blood cells circulating in the blood is a physiological process. When they are destroyed, hemoglobin turns into indirect bilirubin. It is transported to the liver. Here the pigment combines with a sugar-containing substance. This compound is able to dissolve in liquid and is called direct bilirubin. It enters the intestines. Here the compound breaks down and a pigment is formed, which is excreted in the feces.
The direct fraction of the pigment is normally present in the blood only in small quantities. If bilirubin is not removed from the body in a timely manner, its concentration in the blood increases. The cause of this may be liver damage or blockage of the bile ducts. In the second case, bilirubin cannot enter the intestines and turn into brown pigment. Instead, it goes into the urine. Therefore, with this pathology, urine becomes dark, and feces, on the contrary, become lighter.
Hereditary disorders
Gilbert's syndrome
. A harmless form with a favorable course. The reason is a violation of the uptake and transport of bilirubin by liver cells. Unconjugated (unbound) bilirubin increases in the blood.
Rotor syndrome
. It is expressed in a violation of the uptake of bilirubin and, as a result, its removal from the body. It appears at an early age and does not lead to serious consequences.
Dubin-Johnson syndrome
. A rare form of conjugated hyperbilirubinemia. The transport system is disrupted, which causes difficulties in removing bound bilirubin. The syndrome does not lead to dangerous conditions, the prognosis is favorable.
Crigler-Najjar syndrome
. Severe form of unconjugated hyperbilirubinemia. The reason is the lack or complete absence of glucuronyl transferase, a substance necessary for the conjugation of bilirubin in the liver. Causes damage to the nervous system and can lead to premature death.
Timely diagnosis, pathogenetic therapy, proper nutrition, work and rest schedules can qualitatively improve the lives of most patients with hereditary hyperbilirubinemia.
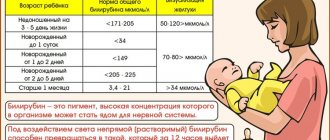
Normal bilirubin level in blood
The level of bilirubin depends on the age and condition of the person.
In newborns, the maximum level of bilirubin reaches the 3rd - 5th day of life, the so-called physiological jaundice. Sometimes it reaches 256 µmol/l. The level should normalize on its own by the 2nd week of life. If the level exceeds 256 µmol/l, immediate examination of the child is required. This condition can lead to brain damage.
No less dangerous is an increase in bilirubin levels during pregnancy. This can cause premature birth, anemia and fetal hypoxia.
Analysis result
| Age | Reference values (in µmol/l) |
| The first day after birth | 24-149 |
| 1-3 years | 58-197 |
| 4-5 years | 26-205 |
| More than 5 years | 5-21 |
An increase in total bilirubin can lead to:
- Cholelithiasis
- Viral hepatitis
- Cirrhosis of the liver
- Choledocholithiasis
- Pernicious, hemolytic, or sickle cell anemia
- Autoimmune hemolysis
- Thalassemia
- Gilbert and Crigler–Nayjar syndromes
- Malaria
- Sepsis
- Transfusions of incompatible blood group
- Hemorrhages in tissue
- Hemorrhagic pulmonary infarction
- Myocardial infarction
- Alcoholic liver disease
Bilirubin levels increase during pregnancy, infectious mononucleosis, liver abscesses, toxic hepatitis, cirrhosis, massive tumors or metastases in the liver.
Symptoms
Abnormalities in the chemical reactions of bilirubin are detected by determining its level in the blood. If the concentration is higher than normal, but does not exceed 85 µmol/l, this is a mild form of hyperbilirubinemia, up to 170 µmol/l is moderate, and from 170 µmol/l is a severe form of the disease. External signs manifest themselves differently, depending on the cause of the increase in bilirubin concentration.
- Liver problems are expressed in the following symptoms:
- Discomfort and heaviness due to liver enlargement.
- Change in urine color (it becomes like dark beer), lightening of stool.
- Heaviness after eating, drinking alcohol, frequent belching.
- Periodically occurring dizziness, general weakness, apathy.
If the cause of the pathological condition is viral hepatitis, then elevated body temperature is added to the symptoms.
- Violation of bile outflow:
- Yellowness of the skin and sclera.
- Itchy skin.
- Intense pain in the right hypochondrium.
- Flatulence, constipation or diarrhea.
- Dark urine, light stool.
A common cause is gallstone disease. The list functions normally, neutralizes incoming bilirubin, but its removal from the body is difficult.
Prehepatic jaundice
- a condition caused by the rapid destruction of red blood cells. Expressed by the following symptoms:
- Anemia.
- Dark stools with normal urine color.
- Extensive hematomas that form without external causes.
- Skin itching, worse at rest and after warming up.
- Yellowish skin color.
Also, sometimes, regardless of the cause, symptoms such as bitterness in the mouth, changes in taste, weakness, impaired memory and intelligence may be observed.
Blood test indicator table
Decoding a biochemical blood test is a comparison of the results obtained with normal values. The analysis form contains a complete list of indicators determined by the biochemical laboratory and their reference values.
The norms for biochemical blood test indicators in adults are shown in the table:
| Analysis: | Men: | Women: |
| Total protein | 64-84 g/l. | 64-84 g/l. |
| Hemoglobin | 130-160 g/l | 120-150 g/l. |
| Haptoglobin | 150-2000 mg/l | 150-2000 mg/l |
| Glucose | 3.30-5.50 mmol/l. | 3.30-5.50 mmol/l. |
| Urea | 2.5-8.3 mmol/l. | 2.5-8.3 mmol/l. |
| Creatinine | 62-115 µmol/l | 53-97 µmol/l. |
| Cholesterol | 3.5-6.5 mmol/l. | 3.5-6.5 mmol/l. |
| Bilirubin | 5-20 µmol/l. | 5-20 µmol/l. |
| AlAT (ALT) | up to 45 units/l. | up to 31 units/l. |
| ASAT (AST) | up to 45 units/l. | up to 31 units/l. |
| Lipase | 0-190 units/l. | 0-190 units/l. |
| Alpha amylase | 28-100 units/l. | 28-100 units/l. |
| Pancreatic amylase | 0-50 units/l. | 0-50 units/l. |
Each of the criteria indicated in the table reflects the condition of one or more human organs. And a combination of some of them sometimes makes it possible to make an accurate diagnosis or direct the diagnostic process in the right direction.
Sometimes it is enough to establish a final diagnosis based on deviations from the norm of one or more parameters. But much more often, a full diagnosis requires other results of additional research methods and an assessment of the clinical picture of the disease.
Total protein
Total protein is the total concentration of proteins found in the blood. Proteins take part in all biochemical reactions of the body - they transport various substances, act as catalysts for reactions, and participate in immune defense.
Normal levels of protein in the blood are 64-84 g/l. If the protein is higher than this, the body may be susceptible to infection. In addition, the cause of increased protein may be arthritis, rheumatism, or the onset of cancer. With a low protein content in the blood, the likelihood of liver disease increases many times, as well as problems with the intestines and kidneys. The most difficult diagnosis for low protein is cancer.
Albumen
This protein is produced by the liver and is considered the main protein in the blood plasma. In general, experts distinguish albumins as a separate protein group, called protein fractions.
An increase in the concentration of albumin in the blood (hyperalbuminemia) may be associated with the following pathologies:
- dehydration, or dehydration (loss of fluid from the body through vomiting, diarrhea, profuse sweating);
- extensive burns.
A reduced albumin level is observed in smoking patients and in women during pregnancy and breastfeeding. In other people, a decrease in albumin may indicate various liver pathologies (for example, cirrhosis, hepatitis, or oncology), or intestinal inflammation of an infectious nature (sepsis). In addition, in case of heart failure or cancer, burns or fever, various injuries or drug overdose, the albumin in the blood will be lower than normal.
Glucose (sugar)
The most common indicator of carbohydrate metabolism is blood sugar. Its short-term increase occurs during emotional arousal, stress reactions, pain attacks, and after eating. The norm is 3.5-5.5 mmol/l (glucose tolerance test, sugar load test).
Sugar is elevated - diabetes, endocrine disorders, pancreatitis, pancreatic tumor, cerebral hemorrhage, chronic liver and kidney damage, myocardial infarction, cystic fibrosis.
Sugar is low - damage to the liver and pancreas, hypothyroidism, stomach or adrenal cancer, arsenic poisoning or certain medications, alcohol intoxication.
Uric acid
The main breakdown product of the main component of nucleic acids - purine bases. Since it is not used further in metabolic processes, it is excreted unchanged by the kidneys. The normal level in blood plasma is 0.16-0.44 mmol/l.
An increase in uric acid levels in the blood indicates:
- renal failure;
- leukemia, lymphoma;
- prolonged fasting;
- alcohol abuse;
- overdose of salicylates and diuretics.
A decrease in the level of uric acid in the blood can be observed during treatment with piperazine drugs, allopurinol, prebenecid, ACTH, sometimes with hepatitis, anemia.
Urea
It is a consequence of the breakdown of proteins. The permissible amount of this substance in a person’s blood changes with age. Often, the level of urea goes through the roof in patients who have pathologies in their kidneys: doctors prescribe a similar blood test to diagnose and predict the disease.
A decrease in the level of urea in the blood can be triggered by reasons that are physiological (pregnancy, fasting, excessive exercise), or pathological (celiac disease, cirrhosis of the liver, heavy metal poisoning).
Creatinine
This substance, like urea, is a product of protein metabolism and is also excreted by the kidneys. Creatinine is a product of metabolic processes occurring in skeletal muscles, and to a lesser extent in the brain. Accordingly, its level will depend on the condition of the kidneys and muscles.
Increased creatinine is observed in renal failure, severe injuries with muscle damage, increased thyroid function, and after the use of certain anti-inflammatory and antibacterial agents. Moderately high creatinine is found in athletes.
Alanine aminotransferase (ALT, AlAt)
This indicator, along with AST, is used in medical practice for laboratory diagnosis of liver damage. Alanine aminotransferase is synthesized intracellularly, and normally only a small part of this enzyme enters the blood. When the liver is damaged (hepatitis, cirrhosis) as a result of cytolysis (cell destruction), this enzyme enters the blood, which is detected by laboratory methods.
The level of this transaminase may also increase during myocardial infarction and other conditions. An increase in ALT that exceeds an increase in AST is characteristic of liver damage; if the AST indicator increases more than the ALT increases, then this, as a rule, indicates problems with myocardial (heart muscle) cells.
Aspartate aminotransferase (AST, AST)
A cellular enzyme involved in amino acid metabolism. AST is found in the tissues of the heart, liver, kidneys, nervous tissue, skeletal muscles and other organs. An AST blood test may show an increase in AST in the blood if the body has a disease such as:
- myocardial infarction;
- viral, toxic, alcoholic hepatitis;
- angina pectoris;
- acute pancreatitis;
- liver cancer;
- acute rheumatic carditis;
- heavy physical activity;
- heart failure.
AST is elevated in skeletal muscle injuries, burns, heat stroke, and as a result of cardiac surgery.
Alkaline phosphatase
Many laboratories automatically include this enzyme in their biochemical analysis. From a practical point of view, only an increase in the activity of this enzyme in the blood may be of interest.
This is evidence of either intrahepatic stagnation of bile in the small bile ducts, which occurs with mechanical and parenchymal jaundice, or progressive osteoporosis or destruction of bone tissue (myeloma, aging of the body).
Cholesterol
A component of fat metabolism, it is involved in the construction of cell membranes, the synthesis of sex hormones and vitamin D. There is total cholesterol, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol.
Degrees of increased cholesterol in the blood:
- 5.2-6.5 mmol/l – mild degree of increase in the substance, a risk zone for atherosclerosis;
- 6.5-8.0 mmol/l – a moderate increase, which is corrected by diet;
- over 8.0 mmol/l – a high level requiring drug intervention.
An increase in cholesterol levels in the serum or blood plasma is an argument in favor of atherosclerosis, hypothyroidism (low activity of the thyroid gland), chronic hepatitis, decompensated diabetes mellitus, obstructive jaundice.
This indicator decreases when:
- malignant liver tumors;
- cirrhosis of the liver;
- rheumatoid arthritis;
- hyperfunction of the thyroid and parathyroid glands;
- starvation;
- malabsorption of substances;
- chronic obstructive pulmonary diseases.
Bilirubin
Bilirubin is a yellow-red pigment that is formed when hemoglobin breaks down in the spleen, liver and bone marrow. Its normal level in the blood of children and adults is 3.4–20.5 µmol/l.
If the table with the examination results contains an elevated level of bilirubin, then the doctor can diagnose one of the following diseases in adults:
- cholelithiasis;
- pancreatic tumors;
- inflammatory diseases of the biliary tract.
If bilirubin is below normal, then the patient may have one of the following diseases:
- acute viral hepatitis;
- bacterial liver damage (leptospirosis, brucellosis, etc.);
- toxic hepatitis;
- medicinal product;
- neoplasms in the liver and primary biliary cirrhosis;
- hemolytic anemia of various etiologies.
Bilirubin, formed as a result of the breakdown of hemoglobin (indirect), is released into the blood, where it binds to albumin and is transported to the liver. In liver cells, bilirubin combines with glucuronic acid. This bilirubin bound to glucuronic acid is called direct bilirubin.
Amylase
Breaks down carbohydrates from food and ensures their digestion. Contained in the salivary glands and pancreas. There is alpha-amylysis (diastase) and pancreatic amylase.
- alpha-amylase rate: 28-100 units/l.
- pancreatic amylase rate: 0-50 units/l.
A high amylase content in a biochemical blood test indicates: peritonitis, pancreatitis, diabetes mellitus, pancreatic cyst, stone, cholecystitis or renal failure.
Decreased alpha-amylase: thyrotoxicosis; myocardial infarction; complete necrosis of the pancreas; toxicosis of pregnant women.
Potassium
Another important intracellular electrolyte. Its normal content in the body ranges from 3.5 to 5.5 mmol per liter.
Reduced potassium content:
- excess hormones of the adrenal cortex (including taking dosage forms of cortisone);
- chronic fasting (failure to receive potassium from food);
- prolonged vomiting, diarrhea (loss with intestinal juice);
- renal dysfunction;
- cystic fibrosis.
Increased potassium content:
- dehydration;
- acute renal failure (impaired renal excretion); ,
- adrenal insufficiency.
- cell damage (hemolysis - destruction of blood cells, severe starvation, convulsions, severe injuries).
The condition when potassium is elevated is called hyperkalemia, and when it is low, hypokalemia.
Sodium
Sodium does not directly participate in metabolism. It is completely abundant in the extracellular fluid. Its main function is to maintain osmotic pressure and pH. Sodium excretion occurs in the urine and is controlled by the adrenal hormone aldosterone.
Sodium reduction:
- decreased concentration due to increased fluid volume (diabetes mellitus, chronic heart disease)
- failure, liver cirrhosis, nephrotic syndrome, edema).
- loss of an element (abuse of diuretics, kidney pathology, adrenal insufficiency).
Increased sodium content:
- increased function of the adrenal cortex;
- excess salt intake;
- loss of extracellular fluid (profuse sweat, severe vomiting and diarrhea, increased urination in diabetes insipidus);
- violation of the central regulation of water-salt metabolism (pathology of the hypothalamus, coma).
An increase in a microelement is called hypernatremia, and a decrease is called hyponatremia.
Diagnostics
Doctors are faced with the task of reducing bilirubin levels to normal limits, and this can only be done by knowing the reason for its increase. Therefore, after a blood test to determine the concentration of bilirubin, the following tests are also performed:
- on the level of alkaline phosphatase;
- alanine aminotransferase activity;
- presence of glucuronyl transferase and other studies.
An ultrasound of the liver is also prescribed to determine its condition. Laboratory tests include: general blood and urine analysis, level of total coproporphyrin in daily urine, phenobarbital test, bromsulfalein test, test for markers of hepatitis viruses.
The purpose of diagnosis is not only to determine the level of bilirubin, but also its form. For example, an increase in direct bilirubin occurs when bile flow is impaired (dyskinesia). The concentration of indirect bilirubin increases due to liver problems and excessive destruction of red blood cells. Having established the form of bilirubin, it is necessary to differentiate the specific disease (pathology).
Increased direct bilirubin
The direct enzyme begins to accumulate in the blood due to a disruption in the process of bile outflow. Instead of going into the stomach, it enters the bloodstream. This condition occurs with hepatitis of bacterial and viral etiology, chronic, autoimmune, and drug-induced hepatitis. It can occur with cholelithiasis, cirrhosis, oncological changes in the liver, cancer of the gallbladder or pancreas. Be a consequence of congenital Rotor syndrome (a milder form of a defect in bilirubin excretion) or Dubin-Johnson syndrome (a more severe form).
Increased direct bilirubin - reasons
The increase in the level of direct bilirubin is based on a violation of the outflow of bile. As a rule, this occurs due to the development of the following pathologies:
- Gallstone disease (GSD);
- Hepatitis: viral, bacterial, drug-induced, autoimmune, toxic, medicinal;
- Cancer of the liver, pancreas or gallbladder;
- Biliary cirrhosis;
- Rotor and Dubin-Johnson syndromes.
Why is my liver enlarged? An enlarged liver may be associated with diseases of other organs. We tell you what pathologies cause changes in the size of the body's main detoxifier.
Increased indirect bilirubin
The reason is the rapid breakdown of red blood cells. It can occur as a complication of sepsis, acute intestinal infection, congenital, toxic, acquired autoimmune anemia.
An increase in the indirect form of bilirubin also occurs with Gilbert's syndrome. This is a benign, chronic disease caused by disruption of the intracellular transport of bilirubin. Among the causes of hyperbilirubinemia, Crigler-Najjar syndrome is a disruption of the process of combining bilirubin with glucuronic acid, formed during the oxidation of D-glucose.
The Lucy-Driscol symptom is unusual. It occurs exclusively in infants due to breastfeeding. Breast milk contains an enzyme that disrupts the conjugation of bilirubin. With the transition to artificial feeding, the disease goes away. However, indirect bilirubin is very dangerous, so the occurrence of jaundice after 3-5 days of life requires urgent medical examination.
Diagnosing infants
If in adults jaundice means the presence of diseases, then in children hyperbilirubinemia can be physiological or pathological. In the first case, it is noted by the 4th day of life, in Asian children by the 7th, it goes away on its own, without reaching critical levels of bilirubin.
The pathology may be a consequence of liver dysfunction, high concentrations of beta-glucuronidase in breast milk, or occur with a low-calorie diet or dehydration. Both the baby himself and his mother are subject to examination.
Anamnesis and external signs are studied. It is important to rule out or diagnose kernicterus as soon as possible. Warning signs include: jaundice on the first day of life and after 2 weeks, increased total bilirubin and the rate of its rise, respiratory distress, the presence of bruises or hemorrhagic rash. The child's bilirubin level and blood, urine and cerebrospinal fluid cultures are measured. It is necessary to exclude the presence of TORCH infections in the mother.
Diagnostics and tests
To determine what is causing the increase in bilirubin, you need to undergo examination by a specialist. After a visual examination (checking the color of the skin, whites of the eyes, plaque on the tongue) and palpation of the abdominal cavity, the doctor prescribes laboratory diagnostics:
- BAC for the content of direct or indirect bilirubin;
- Aspartate aminotransferase and alanine aminotransferase assay;
- Ultrasound examination of the liver.
Blood sampling may be prescribed for a detailed clinical analysis.
Correct therapy can be prescribed only with an accurate diagnosis. In some cases, the help of an infectious disease specialist and gastroenterologist is required.
Treatment
Therapy for hyperbilirubinemia depends on the causes that caused it, i.e., treatment is etiotropic, aimed at the underlying disease.
Disruption of the biliary tract. Stones and obstructing tumors are removed. In some situations, stenting of the bile ducts is carried out - a frame is installed that preserves the lumen.
Hemolysis of red blood cells. Phototherapy and infusion therapy are prescribed to prevent or correct pathological losses. The infusion solutions contain glucose and albumin. These treatments help convert toxic bilirubin into a form that can be excreted from the body.
Kernicterus (bilirubin encephalopathy) in newborns
Pathology occurs in the first week of life. At first it is expressed by the following symptoms: suppression of the sucking reflex, vomiting, lethargy, monotonous cry. If not the signs are mild, if there is a risk of being discharged from the maternity ward without medical assistance. Typically, the disease manifests itself on the 4th day of life and requires an urgent exchange blood transfusion. This prevents the development of irreversible consequences.
After several weeks of development of the pathological condition, symptoms such as stiff neck, “stiff” limbs, convulsive posture with arching of the back, bulging of the large fontanel, hand tremors, convulsions, and a sharp cerebral cry appear.
Since the disease picture develops slowly over several days to weeks, during this time irreversible consequences in the central nervous system often occur. The disease finally manifests itself by 3–5 months of life, leading to paralysis, cerebral palsy, deafness, and mental retardation. To prevent the development of pathology, it is necessary to monitor bilirubin levels. If necessary, reduce the number of breastfeeding procedures. Perform phototherapy or exchange transfusion.
If total bilirubin is increased in men
Exceeding the norm in men may indicate the development of such pathologies:
- Prehepatic (hemolytic) jaundice is often observed in newborn boys if their blood is incompatible with the mother’s blood according to the Rh factor or group. It may also be associated with congenital or acquired anemia.
- Hepatic jaundice (parenchymal) - liver damage against the background of viral hepatitis of various natures, toxic and autoimmune lesions.
- Subhepatic jaundice is associated with impaired movement of bile, pancreatic tumors, metastases and other causes.
Advantages of JSC "SZTsDM"
You can check the levels of all forms of bilirubin, as well as find out the cause of the violation of bilirubin metabolism in one of the laboratories of JSC SZTsDM. This is the largest center conducting all types of laboratory tests, where you can also make an appointment with specialized specialists.
The Northwestern Center for Evidence-Based Medicine is chosen because it has a network of its own laboratories with the latest equipment, as well as:
- qualified medical and friendly employees work;
- high accuracy and quick availability of results are guaranteed;
- collection of materials can be carried out at home and in the terminal, where comfortable conditions for anonymity have been created;
- You can collect the results in several ways.
Another distinctive advantage is the convenient location of laboratories within transport accessibility.
You can get detailed information by calling: 8 (800) 234-42-00.