Bilirubin is a pigment that gives bile its characteristic color. Its direct fraction dissolves in liquid and is normally excreted in bile. To assess the amount of this substance, blood biochemistry is performed. As a rule, this test is prescribed if an increase in total bilirubin has previously been detected. Studying the number of its fractions makes it possible to determine the reason for the increase in overall indicators. The examination program is drawn up by the doctor taking into account the clinical picture and the results of previously performed tests. The analysis is required during the diagnosis of a number of diseases (for example, jaundice).
Detailed description of the study
The liver is an organ in which complex metabolic processes occur. The functional activity of the liver is provided by hepatocyte cells, they are responsible for:
- Bilirubin exchange and bile formation;
- Regulation of carbohydrate metabolism;
- Regulation of fat metabolism;
- Formation of many proteins, including enzymes;
- Neutralization of toxic substances (medicines, alcohol, etc.).
Bilirubin is an orange-yellow pigment formed during the breakdown of heme (a component of hemoglobin). Every day, the human body synthesizes about 350 mg of indirect (free) bilirubin. Most of it is formed during the breakdown of red blood cells, a smaller part (about 20%) is formed from other heme proteins in the liver and bone marrow.
Free bilirubin is insoluble in water; it is transported in human blood plasma in combination with a protein - albumin. Next, the liver captures free bilirubin, and after a series of transformations it is converted into direct (associated with glucoronic acid) bilirubin, which is soluble in water.
Bound bilirubin in bile is sent to the gallbladder and released into the small intestine during food digestion. In the small intestine it is metabolized by bacteria to urobilinogen. Most of the urobilinogen is transformed into stercobilin, which turns the stool brown. A small amount of urobilinogen is reabsorbed by the liver and returns to the bile. A small part is excreted in the urine.
Normally, the level of indirect bilirubin in the blood is very low. If the concentration of bilirubin and its fractions increases, a person may develop yellowness of the skin and whites of the eyes. This condition is called jaundice.
Depending on the cause of bilirubin metabolism disorders, there are three types of jaundice:
- Hemolytic;
- Parenchymatous;
- Mechanical.
1) Hemolytic, or suprahepatic, jaundice is associated with increased release of bilirubin into the blood due to increased breakdown of red blood cells. The pigment formed during destruction is not captured by hepatocytes, but remains in the blood (having a toxic effect). A similar pathology can be observed in newborns when their Rh factor is incompatible with that of the mother (Rh conflict).
In rare cases, a congenital disorder of bilirubin metabolism known as Gilbert's syndrome occurs. This disorder is associated with reduced activity of the enzyme glucuronyl transferase, which converts indirect bilirubin into direct bilirubin. As a rule, it is determined by chance and has a favorable clinical course.
Hereditary diseases associated with defects in the functioning of enzymes responsible for bilirubin metabolism also include Dubin-Johnson syndrome and Rotor syndrome.
Increased release of indirect bilirubin into the blood accompanies hemolytic anemia. This condition is also associated with the premature breakdown of red blood cells and the inability to fully metabolize this pigment in liver cells due to its excess.
May be caused by internal defects in the red blood cells themselves (hereditary pathology) or:
- Taking certain medications (methyldopa, penicillin, quinine, etc.);
- Immunological disorders;
- Infections;
- Mechanical damage to blood vessels;
- Toxic effects (copper, lead).
2) Hepatic, or parenchymal, jaundice occurs due to lesions of the liver tissue. Such conditions are diagnosed with viral hepatitis, poisoning, sepsis, etc.
3) Mechanical, or subhepatic, (obstructive) jaundice occurs due to the presence of mechanical obstacles (stones, tumors) in the bile ducts, which impairs the outflow (excretion) of bile.
A bilirubin test may be used as part of an annual physical to evaluate liver health. It is also used to determine the causes of jaundice and helps the specialist determine the tactics of further therapy.
The study is also carried out in newborns with jaundice to determine its causes.
If bilirubin is elevated during pregnancy
The appearance of jaundice can occur during all stages of pregnancy. If the analysis reveals an excess of bilirubin, this may be associated with the following diseases:
- viral hepatitis in acute form;
- intrahepatic cholestasis;
- acute fatty liver degeneration.
It is viral hepatitis that is the main cause of jaundice in pregnant women - it accounts for up to 50% of identified cases. Symptoms of the disease are varied. The pathology begins to manifest itself with weakness, fever, joint pain, skin rashes, and changes in the color of urine and feces. In these cases, you should immediately consult a doctor, take a blood test and other tests.
The second most common cause of abnormal bilirubin levels in pregnant women is intrahepatic cholestasis (another name is hepatosis). It accounts for up to 25% of identified cases. The main symptoms are;
- frequent itching of the skin;
- moderate jaundice;
- darkening of urine;
- stool lightening;
- rarely – prolonged, repeated vomiting.
As a rule, the described signs progress during the 3rd trimester, less often they appear at earlier stages. When taking an analysis, it turns out that bilirubin exceeds the norm by 4-5 times.
Finally, jaundice may also be associated with acute fatty degeneration. This pathology is much less common - 1 in 13,000 births. It manifests itself as a complication, more often in primiparous women in the last stage of pregnancy. The exact cause of the pathology has not yet been established.
References
- Clinical guidelines “Drug-induced liver damage”, 2019. - 35 p.
- Pakhomova, R.A., Kochetova, L.V. Clinical manifestations of obstructive jaundice and liver failure, depending on the severity of obstructive jaundice of benign origin.” — Modern problems of science and education, 2021. — No. 6. — P.47.
- Sullivan, J., Rockey., D. Diagnosis and evaluation of hyperbilirubinemia. — Current opinion in gastroenterology, 2021. — Vol. 33(3). — P. 164-170.
Direct bilirubin: norm and pathology
Reference values
are the same for patients of both sexes and all ages. A separate norm has been established only for newborns. Normal indicators should be in the range of 0-8.6 µmol/liter. When interpreting the results, the patient’s medical history and data from other tests are taken into account.
Increasing performance
may indicate a violation of the outflow of bile for various reasons, genetic pathologies, liver pathologies. It must be taken into account that the cause of an increase in bilirubin levels can be prolonged fasting, eating large amounts of fatty foods, or taking many medications (for example, antibacterial and antifungal agents, antidepressants).
How to normalize bilirubin metabolism
It is important to keep the level of the substance normal, but traditional methods are useless here. It is necessary to identify the cause of the pathology and undergo treatment with drugs, strictly following the doctor’s instructions. In case of liver disease, a man will have to go to hospital and adhere to a strict diet. If the concentration disorder is caused by blockage of the bile ducts with stones, they resort to surgery.
Although hereditary pathologies are not amenable to drug therapy, the man’s condition is maintained with periodic red blood cell transfusions. In case of severe genetic diseases, excision of the spleen is recommended.
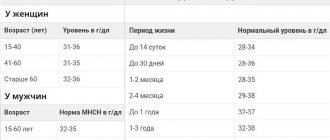
Normal values
When comparing BIL in men and bilirubin in women, the norm may be slightly different even for patients of the same age. This is due to the peculiarities of physiology and hormonal regulation in representatives of different sexes.
In men
A detailed examination plan should be drawn up by a doctor.
So, let’s find out what the normal total bilirubin should be in men by age: the table below will help you figure it out.
Table 1: Total bilirubin in men - normal:
| Age | Indicator, µmol/l |
| Newborns (1 day) | 23,1 |
| Day 2 | 54,2 |
| 3-4 day | 90,1 |
| 5-6 day | 72,0 |
| 7-9 day | 53,0 |
| 10-30 day | 3,10 |
| 1 month-14 years | 3,4-13,7 |
| 15-20 years | 3,7-8,1 |
| 21-30 years old | 3,8-19 |
| 31-40 years old | 3,8-18,5 |
| 41-50 years | 3,9-18,7 |
| 51-60 years | 3,8-18,5 |
| Over 60 years old | 3,7-18,5 |
Looking at the table, you will notice that BIL-T levels remain relatively stable throughout life. We will not take into account the period of newbornhood and the first month of life - here the sharp increase in the concentration of bile pigment is due to the physiological destruction of fetal hemoglobin and the transition of the baby’s body to a new “operating mode”.
In general, representatives of different ages have approximately the same total bilirubin: the norm in men over 50 years of age is practically no different from that of thirty-year-olds. The physiological values of D-BIL and ID-BIL can be found in the diagrams below.
Reference values for D-BIL in men
ID-BIL norms
Among women
First, let's compare total bilirubin - the norm for women by age - the table is presented below.
Table 2: Total bilirubin: normal for women by age:
| Age | Indicator, µmol/l |
| Newborns (1 day) | Less than 35 |
| Day 2 | 25-150 |
| 3-5 day | 25-205 |
| 5-6 day | 125 |
| 7-9 day | 45 |
| 10-30 day | 3,10 |
| 1 month-14 years | 5-14,7 |
| 15-20 years | 5-19 |
| 21-30 years old | 3,8-19 |
| 31-40 years old | 3,9-17,6 |
| 41-50 years | 3,7-17,4 |
| 51-60 years | 3,7-17,9 |
| Over 60 years old | 3,0-18 |
Here we also see that newborns and infant girls have very high bilirubin: for women the norm is relatively stable. Now let's look at bound bilirubin - the norm for women of different ages is indicated in the form of a diagram.
D-BIL in women
We will also compare ID-BIL indicators.
ID-BIL in women
Important! The authorities indicated in the sections above are only generally accepted, and you should not rely entirely on them. The fact is that each laboratory uses its own equipment and its own reagents. Therefore, when comparing the obtained analysis results with the reference ones, always pay attention to the “norm” column on the form.
Questions for the doctor
Additional examination
Hello! Recently, my dad (he is 64 years old) was invited for a preventive examination at the clinic. Now the nurse called and said the bilirubin level was high. I myself noticed that his skin and eyes were somehow yellowish. But he himself has no particular complaints.
Tell me what additional examination should dad undergo in order to determine the reason for the poor analysis? After all, is bilirubin 60 in an adult man abnormal?
Expert opinion
Romanova Natalya, surgeon
Good day! Indeed, a BIL-T value exceeding 18.5 μmol/L is considered pathologically elevated. To find out the causes of the disease, I recommend that your dad take:
- Laboratory tests:
- UAC;
- OAM;
- additionally determination of fractions D-BIL, ID-BIL;
- scatological research;
- Instrumental tests:
- Ultrasound of the liver and gastrointestinal tract;
- according to indications - radiography.
The instructions written above are just the standard minimum; you may need something more. After receiving the results, be sure to show them to your doctor to draw up an adequate plan for diagnosing and treating the disease. Be healthy!
How to prepare for the test: diagnostic features
Bilirubin in men is determined by a biochemical blood test. For planned biochemical studies it is necessary to prepare:
- A few days before blood sampling, avoid alcohol, fried foods, and spicy foods.
- In the morning before the test, do not eat, drink juices, carbonated drinks, coffee or tea.
- Do not smoke before blood collection.
On the day of the analysis, it is forbidden to have breakfast. Donate blood on an empty stomach.
Sometimes, if the condition worsens, urgent analysis is necessary. During an emergency examination, small errors in readings are acceptable and no special preparation is required.
Signs of changes in bilirubin in the blood
The disease is indicated not only by the result of a blood test, but also by external signs. With an increase in the amount of bilirubin in plasma, the following is noted:
- Yellow skin tone. A similar symptom is sometimes provoked by an increased concentration of vitamin A, pathologies of the pancreas or thyroid gland. With hyperbilirubinemia, the sclera of the eyes necessarily turn yellow - this sign allows you to more accurately determine the disease.
- Bitter taste in the mouth.
- Periodic nausea and vomiting.
- Feeling of heaviness in the area of the right hypochondrium.
- The stool is discolored.
- The pigment accumulates in the urine, so its color resembles dark beer.