Acute chest pain is a serious cause for concern. It may be the first symptom of a heart attack, so you should always seek medical help at the first sign of discomfort. However, such signs may also indicate intercostal neuralgia - nerve pain, which is less dangerous for the patient. At home, there are several ways to distinguish heart pain from neuralgia. They will allow you to always remain calm, identify life-threatening conditions in a timely manner and provide accurate information to the doctor about your well-being.
How does cardiac neuralgia manifest?
The clinical picture of the disease manifests itself in a paroxysmal form. Rolling pain in the heart area brings with it unpleasant sensations:
- burning;
- numbness;
- tingling.
Localization of symptoms can be not only in the chest area, but also in the area of the back, ribs, and shoulder blades.
The development of intercostal neuralgia is provoked by pathological conditions of the nervous system, infections, and weak immunity. The attacks vary in duration and usually begin in the evening or at night. With sharp turns, deep breathing, and coughing, the pain intensifies.
In addition to pain, intercostal cardiac neuralgia is accompanied by other symptoms associated with irritation and further compression of the nerve roots. Along with pain, isolated muscle contractions with twitching may be observed.
With neuralgia of the heart, increased sweating may occur. The color of the skin changes - it becomes pale or turns red. In the area of direct damage to the nerve fibers that cause neuralgia in the heart area, a burning sensation, tingling sensation appears, loss of sensitivity, and numbness are observed.
The patient may remain in an antalgic position. A person suffering from cardiac neuralgia bends the body in the healthy direction and strives to maintain this position. At the same time, the intercostal spaces are stretched, which reduces compression and irritation of the nerve endings, thereby reducing pain.
For treatment of this disorder, you can contact a therapist, neurologist or cardiologist. These specialists know exactly how to distinguish intercostal neuralgia from heart pain.
What is intercostal neuralgia?
Neuralgia of the intercostal nerves is pain of a different nature that occurs due to various etiological factors. It is more often observed in adult men and women over 30-35 years of age. Symptoms of neuralgia may appear suddenly on one or both sides of the chest, along one or more intercostal nerves. The disease has an ICD code - M.79.2.
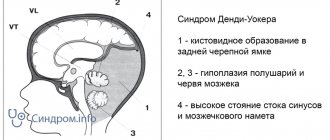
To understand what intercostal neuralgia is, you should understand the anatomical features of the thoracic nerves. There are 12 pairs in total. Each intercostal nerve contains motor, sensory and sympathetic fibers. It originates from the anterior roots of the spinal cord of the thoracic spine, passes along the lower edge of each rib, reaching the sternum. The parietal pleura covers the nerve fibers on top.
Thoracic nerves transmit impulses to the skin, the musculo-ligamentous apparatus of the chest and the anterior wall of the abdomen, partly the pleura and peritoneum, and the mammary glands. Sensitive fibers of neighboring nerve trunks actively interact with each other, creating cross innervation.
Differentiation of neuralgia and heart pain
It is important to know the difference between heart pain and neuralgia in order to provide or receive timely help.
Important differences in the manifestation of pathologies:
- pain syndrome. With neuralgia, any body movements, including inhalation and exhalation and normal walking, lead to increased pain. When there is pain in the heart, its intensity does not change depending on the depth of breathing;
- duration of the attack. Heart pain can be relieved in 15-20 minutes by taking medicine (validol, nitroglycerin). These drugs will not help with neuralgia;
- arterial pressure. Cardiovascular disorders lead to increased blood pressure during a painful attack and increased heart rate. Neuralgia does not cause changes in blood pressure;
- nature of pain. Coronarogenic pain in the heart is strong, pressing, with neuralgia it is burning and short-lived;
- localization. In case of heart problems, the pain is concentrated on the left or behind the sternum, neuralgia is accompanied by pain along the affected nerve;
- additional symptoms. Coronarogenic pain syndrome can be accompanied by cold sweat, pallor, and a feeling of shortness of breath. If the pain is of neurological origin, sweating, increased blood pressure, and limited mobility are possible;
- provoking factors. Heart pain can be associated with physical and emotional stress. Neuralgia is caused by sudden movements and uncomfortable posture;
- reaction to medications. Pain in the heart is relieved by treatment with nitroglycerin; neuralgia can be relieved by taking NSAIDs.
These signs are key in recognizing the nature of pain. But for an accurate diagnosis, additional examination is required. To identify the nature of the pathology, specialists from the IntegraMed CDC (formerly NDC) in St. Petersburg prescribe the following procedures:
- appointment with a cardiologist;
- appointment with a therapist;
- CT scan;
- Ultrasound;
- ECHO-cardiography;
- MRI of the spinal column.
Diagnosis of intercostal neuralgia
Make an appointment Shpigel Anna Yakovlevna Neurologist, massage therapist 33 years of experience. The specialist receives: - newborn children and schoolchildren - adults - athletes Reviews from patients Consultation from 3000 rubles.
Acute intercostal neuralgia is a reason to contact a competent, qualified neurologist. Since symptoms in adults with damage to the thoracic nerves can be disguised as other diseases, the patient must undergo a comprehensive examination to exclude possible pathology. The doctor must conduct a survey and examination.
The person’s posture is noteworthy when he leans towards the healthy side, so as not to provoke a painful attack. Palpation of the chest reveals pain. Trigger points are identified at the lower edge of the rib, where the affected nerve passes. If neuralgia affects several nerve branches, which often happens, this leads to a decrease or complete loss of sensitivity in the corresponding area of the body.
First of all, the doctor must distinguish the symptoms of intercostal neuralgia on the left from cardiovascular pathology. For this purpose, the patient undergoes an ECG. If indicated, a cardiologist is consulted. In order to correctly diagnose and treat intercostal neuralgia, the doctor also excludes diseases of the respiratory system, digestive tract, musculoskeletal system, infectious processes and other diseases. He may prescribe a number of additional tests (laboratory tests, x-ray of the lungs, ultrasound of the abdominal organs, MRI of the spine, etc.).
Thoracic neuralgia is an indication for electroneurography. This method allows you to determine the condition of nerve fibers by assessing their structure and functionality.
Chest neuralgia can be a manifestation of benign and malignant tumors. It is often the first symptom of a herniated disc and degenerative changes in the spine. Therefore, early identification of its causes is considered an important task for the neurologist and the patient.
The main characteristics of pain arising from cardiac pathologies
Heart disease is divided into several types of pathology: angina pectoris, myocardial infarction, pericarditis, myocarditis.
Each pathology is accompanied by specific signs, having an idea of which, a person can sound the alarm in time and seek help from a medical institution.
Angina pectoris
An attack of angina is an acute heart failure caused by vasospasm, resulting in insufficient oxygen reaching the heart. The heart begins to contract harder, causing unpleasant sensations such as:
- sudden pain like a prick;
- pain radiates to the upper limbs;
- appear: panic, anxiety, fear of death;
- lack of air, suffocation;
- increased sweating;
- pallor of the skin.
With angina pectoris, pain appears, similar to an injection.
The pain disappears in a short time, as unexpectedly as it appeared. Heart rhythm returns to normal.
The nature of the pain helps differentiate angina from thoracic osteochondrosis. Pain when nerve endings are pinched always occurs or disappears with body movement and does not go away after using heart medications (nitroglycerin). The pain that occurs with this cardiac pathology is provoked by stress, intense physical activity, sudden temperature changes, overeating and goes away after taking nitroglycerin.
The intensity of pain during angina pectoris does not increase with coughing or movement, but may reappear during exercise.
Myocardial infarction
Myocardial infarction occurs as a result of a blood clot formed in an artery, which clogs the lumen of the vessel. Blood circulation in this place stops, the integrity of the vessel is disrupted, which leads to bleeding and death of nearby tissues. All this is accompanied by the following symptoms:
- sharp, sudden pain that occurs in most cases at night;
- inability to move due to pressing pain behind the sternum;
- panic attacks, resulting in an increase in the level of adrenaline in the blood. Due to the release of adrenaline, the coronary vessels dilate, the pressure drops, and the person loses consciousness;
- severe weakness, feeling of cold, vomiting, thready pulse.
During myocardial infarction, sharp, sudden pain appears.
Life-threatening pain is the main symptom that distinguishes a heart attack from osteochondrosis.
Heart attack pain generally does not arise out of nowhere, but is the result of atherosclerosis, coronary heart disease.
Pericarditis
Pericarditis occurs when the serous membrane of the heart becomes inflamed. Inflammation disrupts the contractile function of the heart, causing unpleasant symptoms:
- pain of increasing nature;
- hyperthermia;
- respiratory dysfunction;
- nausea and vomiting;
- When listening to the heart, a murmur is heard.
Inflammation of the lining of the heart during pericarditis
The main difference between cardiac pain during pericarditis and chondrosis is increasing pain, the intensity of which increases for several days.
- What you can’t do and what you can do at home if your heart hurts
Myocarditis
Myocarditis is an inflammation of the heart muscle, accompanied by the following symptoms:
- slow heartbeat;
- low blood pressure;
- sensations of pain behind the sternum, pressing in nature;
- breathing problems, shortness of breath;
- pale skin with a bluish tint;
- swelling.
Inflammation of the heart muscle with cardiac myocarditis
Symptoms of pain of a pressing nature are a distinctive feature from pain with osteochondrosis.
Prevention
Prevention is a simple and affordable way to reduce the risk of intercostal neuralgia in adulthood. It includes moderate physical activity, selected in accordance with the general well-being of the patients. Loads should be dosed and regular, preferably daily.
It is important to monitor your posture. If you are predisposed to disorders, perform a set of exercises aimed at strengthening the muscle corset. To maintain immunity, you should avoid excessive stress and stress, eat well, and avoid hypothermia.
Causes
The causes of intercostal neuralgia may be associated with inflammation of the peripheral nerves. As a rule, it develops as a result of hypothermia or an infectious process of another localization. For example, intercostal neuralgia often occurs as a result of herpetic infection or herpes zoster.
Intercostal neuralgia develops as a result of degenerative changes in the thoracic spine. Diseases that lead to the destruction and reduction of the height of the intervertebral discs provoke compression of the nerves. Bone growths form on the vertebrae, which also irritate the nerves.
Other possible reasons include:
- Physical overexertion. Staying in an uncomfortable position for a long time, sleeping on a hard or too soft mattress, intense exercise, as well as chronic vertebrogenic syndrome can lead to compression of the nerves.
- Injuries. Nerve damage can be caused by broken ribs, bruises, and injuries to the chest and spine.
- Cardiovascular diseases. A number of pathologies lead to hypoxia of the nerve trunks - atherosclerosis, arterial hypertension, rheumatism and anemia.
- Endocrine disorders. Intercostal neuralgia is often diagnosed in women during menopause, patients with thyrotoxicosis, diseases of the adrenal glands, and also after long-term use of hormonal drugs.
This is not a complete list of diseases and pathological conditions that are accompanied by intercostal neuralgia. The risks of developing the syndrome increase with gastric and duodenal ulcers, diabetes mellitus, tumor diseases, gastritis and colitis.
Which cardiovascular drugs are gastro or hepatotoxic?
Gastrotoxicity of a drug is an undesirable drug reaction, expressed in damage to the organs of the digestive system and associated with the peculiarities of the mechanism of drug metabolism, as well as the dose and duration of their use. When they talk about hepatotoxicity, they mean the predominant damaging effect of the drug on the liver. However, there are drugs that negatively affect both the gastrointestinal mucosa and liver cells.
Drugs prescribed by a cardiologist that can cause toxic damage to the gastrointestinal tract include antiarrhythmic, antihypertensive, hypolipidemic (to reduce the level of cholesterol, triglycerides, low-density lipoproteins associated with the risk of developing vascular atherosclerosis) drugs, as well as aspirin, used to prevent thrombosis. The main task of a cardiologist when selecting therapy is to take into account the existing gastrointestinal disease and select a drug that has less gastro- and hepatotoxicity. In turn, the gastroenterologist observing the patient can additionally select drugs to protect the gastrointestinal tract.
Treatment
Treatment is selected taking into account the root cause of the pathological process, as well as the current condition of the patient.
To relieve acute pain during an attack of intercostal neuralgia, painkillers are used. If the pain is very severe, they give injections - injections with solutions of lidocaine and novocaine.
In the acute stage of the pathological process, the patient is prescribed bed rest and rest. Drugs and methods are selected aimed at normalizing the functioning of the nervous and muscular systems:
- B vitamins;
- analgesics;
- muscle relaxants;
- sedatives;
- NSAIDs.
If there is severe swelling of the tissues, diuretics are prescribed to the patient.
If the pathological process is caused by a herpes infection, antiviral and antihistamines are prescribed. If it is not possible to check for infection, they are prescribed for preventive purposes.
The rehabilitation period can last several weeks or even months. How long it lasts depends on the patient's condition. The doctor selects a set of measures aimed at restoring the nervous system:
- exercise therapy;
- massotherapy;
- osteopathy;
- drug therapy.
In the period between exacerbations, mud therapy, as well as radon, sodium chloride, and sulfide baths can be used. Manual therapy, kinesiotaping and acupuncture are used to relax the fascia of the chest and back, improve the functioning of nerve fibers and overall well-being.
How exactly to treat intercostal neuralgia is determined by a neurologist. Self-medication for this disease is unacceptable.
Heart diseases with similar symptoms
I want to say that there are many cardiac and vascular pathologies that are accompanied by similar symptoms. I propose to consider the most common abnormalities, this will help to understand whether the heart or neuralgia is the cause of the pain.
Angina pectoris
Pain in this case occurs in the area of the heart muscle (but do not forget that there are atypical attacks). It has a diffuse nature, a person is not able to indicate the exact location. Its strength and description are variable: it can be pressing, piercing, cutting, baking. It radiates to the left arm, under the shoulder blade, neck, lower jaw. It does not depend on the position of the body, but can be provoked by physical overload, nervous stress, as well as sudden hypothermia or overheating.
At this moment, there is a fear of death, shortness of breath with difficulty in inhaling. The attack can be one-time, occurring 1-2 times a day or more often. Its duration ranges from 3-5 to 20 minutes. Almost the same signs are characteristic of myocardial infarction. But unlike angina, the attack usually lasts a long time. The patient takes a certain position in bed - sitting with his legs down or lying on several pillows. You can read more about angina pectoris and how to deal with it in the article at the link.
Myocarditis
Inflammatory diseases are accompanied by moderate pain, which is monotonous. Occurs in 90% of all patients. They describe it as aching or pressing. In the acute period, signs of inflammation are observed (fever, body aches), shortness of breath with impaired inhalation or exhalation. The history often reveals a recent infectious disease. There is no clear dependence on physical activity.
Often myocarditis simulates angina pectoris, especially in older people, when pain and lack of air come to the fore, and the rest of the symptoms are smoothed out or do not appear.
Perikadite
The pain of pericarditis gradually increases, but when effusion appears, it can significantly decrease or go away completely. It stings, cuts, radiates to the neck, back, shoulder, to the right side, and lasts for a long time. Some relief occurs in a sitting position with anterior tilt.
In acute dry inflammation, an attempt to make a deep entrance increases the pain, so with this disease a person breathes quickly and shallowly. During auscultation, in this case, I clearly heard the pleural friction noise. The heart most often hurts with this type of pericarditis in the apex area.
A complete collection of information about pericarditis and its treatment methods is here.
Aortic aneurysm
The symptoms of this acute condition are largely reminiscent of myocardial infarction. A sharp increase in blood pressure, stress or physical activity can be a provocation. The pain is tearing, bursting, localized in the retrosternal region, radiating to the neck, lower jaw, right side of the chest, and sometimes runs along the spine. Has a wavy character. In some cases, it spreads to the projection area of the abdominal aorta and even to the legs.
At the same time, sharp pressure surges appear; when the pressure drops, a collapsible state may occur. There is an asymmetry of the pulse on the left and right arms. As blood begins to accumulate under the inner lining of the aorta, symptoms of anemia (pallor and blueness of the skin, dizziness) quickly develop.
Pulmonary embolism
Pulmonary embolism is accompanied by sharp and severe pain, which is localized in the center of the sternum, as well as to the left or right of it. It can last from a few minutes to 3-5 hours and is associated with respiratory movements of the chest. At the same time, a lack of air comes to the fore, a sharp decrease in pressure, up to collapse. Clinical manifestations depend on the location of the thrombus and its size. When the lumen of a large vessel is blocked, cyanosis appears in the upper part of the body, arrhythmia with an increase in pulsation frequency. When small arteries are blocked, the skin develops blue, shortness of breath, the pain is most often moderate, cough and sputum streaked with blood are observed.
Case from practice
A 56-year-old woman came to see me with complaints of chest pain that radiated to her arm.
She noticed her first attacks 1.5 years ago, with a history of large-focal infarction of the anterior wall. Palpation reveals increased sensations in the area of the 6-7 thoracic vertebrae. Some relief is noted after lying on a flat, hard surface. After taking an ECG and conducting additional drug tests, cardiac pathology was excluded. The patient was referred for consultation to a neurologist. An MRI reveals an intervertebral hernia. Treatment is rest during an exacerbation, NSAIDs, massage, electrophoresis with novocaine, traction. After completing the full course, my condition is satisfactory.
Stressors: Holmes and Ray model
“What will happen to him! Look how he holds up!” - this can be said about any unfamiliar person, and then you are surprised to find out that he is trying his best and has already suffered 2 heart attacks. Based on the time of action, psychogenic factors of CVD are divided into mental trauma and psychotraumatic situations. Injuries occur suddenly, a person is at the mercy of emotions and often does not have time to adapt (acute stress). Psychotraumatic situations exist for a long time, sometimes for years. At some stage, a person can adapt to them, but over time, compensatory mechanisms are exhausted. The disease develops.
How can you assess the strength of the negative influence and the body’s resource? According to the importance of the operating factor, life situations are assigned different numbers of points. In 1970, American psychiatrists T. Holmes and R. Ray analyzed people's reactions to significant events, ranked them and compiled a scale of stressors. The list includes not only obvious disasters, but also a large number of “ordinary” events and situations. The ten most important situations are listed below in descending order:
- death of a spouse or other closest person;
- divorce of spouses;
- separation of spouses (in marriage);
- imprisonment;
- death of one close family member;
- illness (injury);
- marriage;
- dismissal;
- reconciliation of spouses;
- termination of work upon retirement.
Fewer points are “given” for changing jobs, vacations, pregnancy, fines for minor offenses, and changing habits. In the Holmes and Ray scale there are only 43 event points that can pull the rug out from under your feet.
To assess the resource and likelihood of developing a nervous or psychosomatic disorder, the authors of the theory recommended noting the events that a person experienced during the year and summing up the points. A high score on the Holmes and Ray scale indicates that the subject has exhausted his resources and needs immediate help.
Associated pain
Patients often make an appointment with a urologist and gynecologist due to pain in the lower abdomen. This is how osteochondrosis of the lumbosacral spine manifests itself. Formed osteophytes infringe on the spinal roots, causing disruption of innervation. Therefore, when patients ask whether osteochondrosis can cause pain in the lower abdomen, vertebrologists answer in the affirmative. The progression of the pathology is indicated by the absence in the clinical picture of characteristic signs of urogenital diseases - bleeding, the appearance of cheesy discharge, cutting and burning during urination. But difficulties with emptying the bladder and intestines due to disrupted innervation cannot be ruled out. With exacerbation of osteochondrosis, other specific symptoms may occur:
- pain in the mammary glands, requiring differential diagnosis to exclude benign or malignant tumors;
- pain in the hypochondrium, epigastric region, reminiscent of an attack of gastritis, cholecystitis, pancreatitis, hepatic colic, hepatitis.
There have even been cases of toothache occurring during relapses of cervical osteochondrosis. Also, a person’s condition can be complicated by increased blood pressure, headaches, and dizziness. The psycho-emotional state is often destabilized - sleep is disrupted, anxiety and fatigue arise.