Experts from the World Health Organization believe that a stroke is a rapidly developing total or focal impairment of brain function that lasts more than 24 hours or leads to death. Stroke in women occurs between the ages of 18 and 65. The disease affects the patient’s quality of life and can lead to disability or death. The main reason is that women present with strokes a few days after the onset of the disease, when doctors have to deal with the consequences of the disease, and not with the disease. Neurologists at the Yusupov Hospital quickly diagnose stroke using modern examination methods:
- computer and magnetic resonance imaging;
- Dopplerography of cerebral vessels;
- video electroecephalogram;
- electromyography.
Such methods allow you to quickly determine the signs of stroke in women and apply appropriate treatment.
Symptoms of stroke in women are most often atypical. The patient may accidentally confuse the first sign with a simple malaise or another disease. Signs of a stroke in a woman have the following characteristics:
- age. In women, stroke develops mainly between the ages of 18 and 65;
- type of disease. Most often, women develop a hemorrhagic stroke due to a rupture of a cerebral artery against the background of high blood pressure. This is facilitated by emotional shock, sudden changes in hormonal levels, increased sensitivity to stress;
- hormonal background. Pregnancy, childbirth, taking contraceptives leads to changes in blood clotting and increases the susceptibility to stroke by 20-22%;
- course of the disease. Women are more likely than men to develop stroke complications and have a higher mortality rate. The disease is characterized by a severe course; warning signs of a stroke in a woman occur suddenly;
- ignoring the disease. The first symptoms of a stroke in women do not cause alarm.
Often, the precursors of stroke in women are vegetative-vascular dysfunction and transient cerebrovascular accidents.
What is a stroke
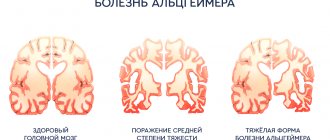
The essence of a stroke is the cessation of blood supply and functioning of a part of the brain as a result of damage to a vessel.
The larger the affected area, the more severe the stroke. Necrosis of a portion of the brain substance is called an infarction [3]. There is a high risk of death in the first few hours, and then in the period up to 28 days after a vascular accident. The annual mortality rate from stroke in the Russian Federation is 374 cases per 100,000 [10]. In 2018, 35% of patients died in the acute period of stroke; by the end of the first year, this figure increases by 15%, and in general, in the first 5 years, the mortality rate of strokes is 44% [11]. The mortality rate from stroke was 92.9 per 100,000 population, and the hospital mortality rate was 19.1% [5].
Long-term disability is most likely for patients who have suffered a stroke. The prevalence of primary disability due to stroke in 2018 was 3.2 per 10 thousand population [2]. Of these, 31% need constant care, 20% have severe mobility limitations, and only 8% return to work [3]. The prevalence of recurrent strokes in 2014 was 0.79%, of which ischemic
strokes account for 87.5% [9].
Brain stem
With ischemia, life- and health-threatening manifestations develop. Like stopping breathing, cardiac activity. This is the only case when a pre-stroke in a woman can lead to death even without the death of cerebral tissue.
Additionally, it is possible to develop elevated body temperature. Thermoregulation is disrupted, the readings fluctuate, from 35 to 38 degrees Celsius or more.
The sign is also considered threatening and requires urgent correction in a hospital setting. The patient is constantly monitored for timely resuscitation.
Causes of stroke
Depending on the cause of cerebrovascular accident, ischemic and hemorrhagic strokes are distinguished.
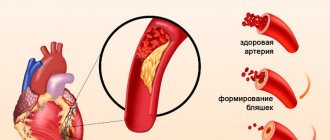
Ischemic stroke occurs as a result of blockage of cerebral vessels by a blood clot, when gradually less and less blood flows to an area of the brain. Hemorrhagic stroke develops as a result of rupture of a vessel and hemorrhage in the brain tissue, as a result of which the blood supply to its area abruptly stops. Hemorrhage can be into the subarachnoid space (SAS) or directly into the cerebral substance (ICH). The ratio of ischemic and hemorrhagic strokes is 4-5:1 [4].
Pathologically, a stroke can be cardioembolic, lacunar, atherothrombotic, or another, including unknown, etiology (TOAST classification) [10].
Predisposing factors:
- men from 45 to 59 years old;
- age 70 years and older (for both sexes) [4];
- arterial hypertension;
- atrial fibrillation;
- atherosclerosis of cerebral vessels;
- coagulopathy, thrombophilia, anemia;
- arteriovenous malformations;
- osteochondrosis with damage to the vertebral artery;
- brain tumors;
- dyslipoproteinemia;
- obesity;
- diabetes;
- intermittent claudication;
- mechanical prostheses of heart valves and blood vessels;
- IHD, myocardial infarction less than 6 months before the stroke;
- other cardiac diseases;
- smoking, alcoholism;
- family history of stroke;
- sedentary lifestyle;
- stress [1, 3].
How to avoid getting sick?
Neurologists admit that it is better to prevent a stroke than to treat it. Restoring lost functions of the human brain is extremely difficult. How to avoid a stroke?
- Monitor your blood pressure. Since the most common cause of apoplexy is high blood pressure, doctors urge to fight it. It is important to monitor him and take all necessary medications.
- Quit alcohol and smoking. By quitting smoking, even the most heavy smokers reduce the risk of cerebral hemorrhage by 4 times.
- Eat a balanced diet and avoid foods rich in cholesterol.
- Fight excess weight.
- Increase physical activity.
- Monitor your emotional health.
- Do not overdo it with the uncontrolled use of hormonal drugs, both contraceptives and during menopause.
If it was not possible to avoid a dangerous disease, then only intensive therapy in the next 2-3 hours can increase the chances of a favorable outcome.
Signs of an incipient stroke
The onset of a hemorrhagic stroke is characterized by the following symptoms:
- severe headache;
- increased blood pressure;
- vomit;
- dizziness;
- loss of consciousness;
- weakness in the limbs;
- visual impairment;
- seizures [1].
The onset of ischemic stroke is gradual; within an hour, some of the following symptoms appear:
- facial asymmetry, numbness;
- difficulty speaking – incoherent, impaired understanding;
- double vision, visual disturbances;
- headache;
- numbness, limited mobility in the limbs, often on one side;
- dizziness, imbalance, staggering, staggering gait;
- confusion with disorientation, subsequently there may be loss of consciousness [3].
If one or more of these signs appear, you should:
- Sit the patient down, providing access to fresh air.
- Call emergency medical help immediately.
- If the patient is conscious and able to chew and swallow, give him one aspirin tablet.
The patient must be hospitalized in a neurological or neurosurgical department, where stroke treatment will be carried out. The sooner the patient is in the hospital, the more effective the therapy.
Symptoms of a stroke
Stroke leads to various brain injuries, depending on the location of the lesion and the pathological type of cerebrovascular accident:
- disturbances of movement in the limbs: from restrictions (paresis) to complete paralysis. When the lesion is localized on the right, the left limbs suffer; with a left-sided lesion, right hemiparesis is formed; in some cases, movements in all limbs may stop (tetraparesis or double hemiparesis);
- sensory disturbances on one or both sides;
- speech disorders (dysarthria - poor articulation; aphasia - inability to pronounce and understand words, write and read);
- ataxia (impaired coordination of movements, “overshooting”, unsteadiness, imbalance, tremor);
- visual impairment: from blindness to double vision and gaze paresis;
- hearing impairment and dizziness;
- violation of mental functions (consciousness, thinking, attention, memory, will, behavior);
- paresis of the soft palate and pharynx, swallowing disorders;
- disorders of urination and defecation;
- depression of respiration and vascular tone;
- increased intracranial pressure;
- patients complain of headaches, vomiting, hiccups, yawning, shoulder pain;
- consciousness is gradually depressed to the point of coma [1, 3].
Causes of death may include cerebral edema, pneumonia, heart failure, and recurrent stroke. In severe cases, “locked-in syndrome” may develop: the patient is conscious, but cannot move, swallow or speak [3].
Occipital lobe
The functions of this part of the nervous system include color recognition and normal vision. Processing incoming visual information and converting it into understandable images.
- Complete blindness. Temporary or so-called transient. The disorder has no connection directly with the retina or the visual tract up to the brain.
- Inability to estimate the distance to an object. Understand its dimensions. Metamorphopsia occurs. Small objects appear larger than the patient herself and vice versa. The small room seems like a huge hall.
This is a direct indication of the neurogenic origin of the disorder, because the eye is not able to independently process information. This is just a source, an input for images; the processes of transformation and analysis take place in the cerebral cortex.
- Induced color blindness. Inability to recognize colors.
- Scotomas. Loss of areas of the visual field. They look like black spots that block your view. In the paracentral areas and along the periphery, usually from the side of the temples.
- The simplest visual disturbances. Photopsias. Flashes of light, bright dots, lines. Rings, geometric shapes. There is no objective source of irritation. The central nervous system is excited spontaneously. Restoring blood flow leads to compensation of the condition.
Consequences of a stroke
There are transient ischemic attack (less than a day), minor stroke (from 1 day to 3 weeks) and stroke with persistent residual effects. The consequences of a stroke are expressed mainly in motor and sensory disorders, the formation of muscle contractures (pronounced constant restriction of movements in the joints), speech and swallowing disorders. General symptoms may also remain, including confusion, disturbances in thinking, will, and emotional regulation. Complications can develop: from epilepsy to bedsores, encephalopathy and anxiety-depressive syndrome [1, 3].
Limbic system
{banner_banstat9}
The key symptom of damage to subcortical structures (in particular the cerebellum) is a violation of orientation in space.
The patient loses understanding of the spatial structure and her position in it. A painful manifestation. If during dizziness the sense of place is formally preserved, in this case it is also lost.
At the same time, there may be a loss of the ability to learn, absorb new information and use it.
Pre-stroke, transient ischemia of the limbic system is rare: 3-5% of the total number of cases.
Diagnosis of strokes
First of all, it is necessary to conduct a detailed neurological examination. Instrumental diagnostic studies and laboratory tests are also prescribed. In case of a stroke, in the first hours, an MRI or CT scan of the brain is performed, if necessary, CT or MR angiography, color Doppler mapping of blood flow, ECG or Holter monitoring, echocardiography as indicated, monitoring of blood pressure, saturation, assessment of the risk of developing bedsores, assessment of swallowing function [ 1, 3, 6].
Tests for stroke
- Complete clinical blood test, including erythrocyte sedimentation rate (ESR).
- Biochemical blood test with determination of C-reactive protein and homocysteine, glucose level, platelet count, activated partial thromboplastin time, INR.
- Interleukin 10.
- Extended coagulogram.
- Determination of acid-base status.
- General urine analysis.
To prepare for neurosurgical intervention, a blood test is additionally performed for hepatitis, syphilis, HIV, blood group and Rh factor determination.
Stroke treatment
Treatment of stroke is regulated by relevant clinical guidelines and the Procedure for providing medical care to patients with acute cerebrovascular accident. In the first hours, thrombolytic therapy is carried out and subsequently - prevention of thrombus formation. For hemorrhagic stroke, neurosurgery may be performed. They normalize blood pressure, water-electrolyte balance, glucose levels in peripheral blood and urine, support the basic vital functions of the body and prevent complications. Drug therapy is also aimed at improving the affected functions of the nervous system [1, 3, 6].
Stroke rehabilitation
Stroke is a disease in which rehabilitation and care are of the utmost importance.
Recovery from a stroke begins in intensive care, from the moment vital functions are stabilized. A multidisciplinary rehabilitation team works with the patient, which includes a rehabilitation doctor, physical therapist or exercise therapy instructor, speech therapist, massage nurse, physiotherapist and physical therapy nurse, psychologist, occupational therapist, guard and rehabilitation nurse. Diagnosis is carried out using special scales that reflect the degree of dysfunction and limitations in the patient’s activity, the influence of environmental factors on the rehabilitation potential. The rehabilitation process continues throughout the entire period of hospitalization. At the second stage, patients with serious disabilities who are unable to move independently are sent to rehabilitation departments or specialized hospitals. Those who can walk independently or with support are rehabilitated in outpatient centers based in clinics and sanatoriums.
The rehabilitation process should not be interrupted, so classes must be continued at home. Of course, there are no high-tech robotic complexes or physiotherapeutic equipment at home, but exercise therapy, massage, and work with a psychologist, speech therapist and occupational therapist are possible. For this purpose, telemedicine technologies are used and visits to rehabilitation specialists are organized.
The individual rehabilitation program includes not only a referral for rehabilitation treatment, but also technical means of rehabilitation. However, usually relatives also have to devote significant physical and financial resources to achieve the best effect [7].
Temporal lobe
The work of this area ensures normal memory, internal speech and mental activity, and hearing in general.
- Epileptic seizures. As is the case with those with lesions of the frontal lobes, they develop suddenly. But they last less time. Otherwise, it is not possible to notice the difference without instrumental techniques. The difference is in the localization of the pathological impulse.
- Lack of hearing. The so-called cortical deafness. The patient completely loses the ability to navigate sounds. This is a temporary phenomenon; treatment as such does not make sense.
- Lack of speech perception. Formally, there is a noise stimulus, but it is impossible to evaluate the logic of the statements, the meaning of them, and even recognize the words.
- Verbal hallucinations of the mental type. So-called pseudohallucinations in outdated terminology. The proverbial voices in my head. Associated with disruption of Wernicke's area.
It is responsible for the production of inner speech. As a result of the anomaly, the signal moves to Broca's center.
He, in turn, identifies external stimuli and perceives them as such, as outside speech. A paradoxical reaction arises.
- Memory impairments of various types. Amnesia, failures. The feeling of a repetition of something that once happened (déjà vu).
Prevention of strokes
Hereditary predisposition to stroke, the presence of cardiac diseases, pathology of blood vessels and blood composition, age over 40 years, obesity and diabetes require a number of preventive measures:
- Maintaining normal blood pressure, taking antihypertensive drugs as prescribed by a doctor, monitoring blood pressure.
- Maintaining a normal level of physical activity, exercise, walking 30-40 minutes a day (for example, walking the dog).
- Conducting preventive examinations, including a standard set of laboratory parameters. During a preventive examination, the following tests are additionally required: gene diagnosis of CADASIL syndrome using the PCR method, plasma factors of the blood coagulation system, antibodies to prothrombin of the IgG and IgM classes to determine the risk of thrombosis, determination of polymorphisms associated with the risk of arterial hypertension, diabetes mellitus, lipid disorders exchange, in order to identify a predisposition to diseases that increase the risk of stroke, von Willebrand factor (a glycoprotein that ensures the formation of blood clots), complex laboratory tests for preclinical diagnosis of cardiovascular diseases are offered (“ELI-ANKOR-Test-12”, “Cardiorisk”).
- Avoiding chronic and acute stress, maintaining mental hygiene.
- Normalization of weight (BMI <25 kg/m2).
- Healthy eating (for example, Mediterranean diet, limiting salt to 5 5 g/day).
- Quitting smoking and taking psychoactive substances.
- Treatment of diseases that are a risk factor for stroke [8, 11].
Bibliography
- Hemorrhagic stroke in adults: clinical recommendations of the Ministry of Health of the Russian Federation, 2021. Developers: Association of Neurosurgeons of Russia. - Electronic text. - URB: (access date 08/18/2020).
- Efremova M.D. Stroke as an urgent socio-psychological problem / M.D. Efremova – electronic text//Skif. Questions of student science.- 2021 - No. 2(24) URB: (date of access 08/17/2021) Access mode: Cyberleninka electronic library system. — Text: electronic.
- Ischemic stroke and transient ischemic attack in adults: clinical recommendations of the Ministry of Health of the Russian Federation, 2021 developers: All-Russian Society of Neurologists, National Association against Stroke, Association of Neurosurgeons of Russia, Association of Neuroanesthesiologists and Neuroreanimatologists, Union of Rehabilitologists of Russia. - Electronic text. - URB: ( access date 08/18/2020).
- Machinsky P.A. Comparative characteristics of incidence rates of ischemic and hemorrhagic stroke in Russia / P.A. Machinsky, N.A. Plotnikova, V.E. Ulyankin [and others] – Direct text.// News of higher educational institutions. Volga region. Medical Sciences.- 2021.- “2(50)-P.112 – 132 DOI 10.21685/2072-3032-2019-2-11.
- Monitoring the implementation of the federal project “Combating Cardiovascular Diseases” - Presentation Department of Organization of Medical Care and Sanatorium Affairs of the Ministry of Health of the Russian Federation URB: (date of access 08/17/2021).
- Order of the Ministry of Health of the Russian Federation dated November 15, 2012 N 928n “On approval of the Procedure for providing medical care to patients with acute cerebrovascular accidents.” — URB: (access date 08/17/2021) Access mode: Electronic library system “Garant”. — Text: electronic.
- Order of the Ministry of Health of the Russian Federation dated July 31, 2021 No. 788n “On approval of the Procedure for organizing medical rehabilitation of adults.” – URB: (date of access 08.17.2021).- Access mode: Electronic library system “Garant”. — Text: electronic.
- Prevention of cerebrovascular accidents: textbook. manual / Compiled by: L.B. Novikova, A.P. Akopyan. – Ufa: Publishing house of the State Budgetary Educational Institution of Higher Professional Education BSMU of the Ministry of Health of Russia, 2015.-58 p.
- Stakhovskaya L.V. Analysis of epidemiological indicators of recurrent strokes in the regions of the Russian Federation (based on the results of the territorial-population register 2009-2014) / L.V. Stakhovskaya, O.A. Klochikhina, M.D., Bogatyreva, etc.]. CONSILIUM MEDICUM, 2021, vol. 5, no. 9, p. 8-11.
- Shamalov N. A. Analysis of the dynamics of the main types of stroke and pathogenetic variants of ischemic stroke / N. A Shamalov, L. V Stakhovskaya, O. A Klochikhina [and others]. Direct text. // Journal of Neurology and Psychiatry named after. S.S. Korsakov. Special issues. 2019;119(3-2):5-10. doi.org/10.17116/jnevro20191190325.
- 1RRE Electronic edition. Updated daily Stroke Day is celebrated on October 29, 2021 URB: (accessed 08/17/2021).
Author:
Pugonina Tatyana Alekseevna, Therapist