When expecting the birth of an heir in the family, future parents wonder who he will take the height from, whether he will be born blond or brunette. But, perhaps, the main question is what blood type is and how the Rh factor is transmitted to the child. Some families will not pay attention to this. But its negative meaning in the future life of the baby can turn into a problem.
Therefore, the following issues need to be taken seriously:
- general concepts about the Rh factor;
- how it is formed;
- what does it depend on;
- How is the Rh factor inherited?
- about its danger during pregnancy of the expectant mother;
- how is a hereditary disease inherited with the Rh factor;
The importance of these issues is identified with the importance of other blood characteristics in general.
Reference values
The result is given in the form:
- RHD+SEX;
- RHD+SEX with additional comment - “A weak Rh antigen has been detected. For blood transfusion, it is recommended to use Rh-negative red blood cells”;
- RHD-OTR.
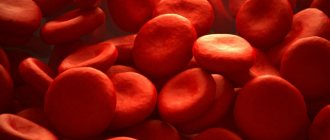
Erythrocytes (red blood cells) carry various proteins (antigens) on their surface. These antigens are inherited from parents.
About 236 erythrocyte antigens have been identified (most of them are rare). They are grouped into blood group systems. One of these systems, which is of great practical importance, is the Rh factor system. Among the Rh antigens, the most important is the D antigen (RhD). It is antigen D that is meant by the term Rh factor. Based on the presence or absence of the D antigen, people are divided into Rh-positive and Rh-negative.
Antigen D (Rh factor) has pronounced immunogenic properties (the ability to cause the formation of antibodies).
Rh conflict (mismatch of Rh affiliation between recipient and donor, mother and fetus) is the cause of hemolytic disease of newborns in 95% of cases, as well as a common cause of severe complications that occur after blood transfusion (post-transfusion complications).
When determining Rh status, several variants of the D antigen are distinguished, which can lead to difficulties in determining it.
Most often, the red blood cells of a Rh-positive person carry all types of D antigen ( normally expressed D antigen
).
Some people have normal types of antigen on their red blood cells, but their amount on the cell surface is reduced - this variant is called D weak
.
If red blood cells do not carry all types of D antigen (they differ qualitatively), then this option is designated as D variant
.
A blood test for Rh status is an important stage in the preoperative preparation of the patient, when there is a possibility that a donor blood transfusion (blood transfusion) will be required. If a person (recipient) with Rh-negative blood is transfused with Rh-positive blood, the recipient’s immune system will recognize this antigen as foreign and trigger the production of antibodies to it (as a rule, a small amount of antibodies is formed, but so-called memory cells (B-lymphocytes) remain) who remember antigen D). Upon repeated contact with foreign erythrocyte antigens, a large number of antibodies are immediately formed, and donor erythrocytes begin to be massively destroyed. This leads to post-transfusion complications - hemolytic anemia (a decrease in hemoglobin capable of carrying oxygen to tissues and organs due to the destruction of red blood cells), acute renal failure, jaundice, post-transfusion shock.
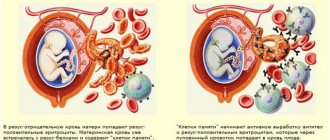
The second possible situation for the occurrence of an Rh conflict is pregnancy, when a Rh-negative mother (there is no D antigen on her red blood cells) is pregnant with a Rh-positive child (the Rh factor is present on the fetal red blood cells). In the later stages of pregnancy, fragments of Rh-positive erythrocytes of the fetus can penetrate into the mother's blood, where they will be perceived as a foreign antigen and cause an immune system reaction - the production of antibodies to the Rh factor. These antibodies, in turn, are able to penetrate the placenta into the child’s body and destroy its red blood cells. During the first Rh-positive pregnancy, the mother’s body usually does not have time to form a sufficiently large number of antibodies, and the fetus does not experience serious complications. However, subsequent Rh-positive fetuses may experience chronic breakdown of red blood cells. Usually, if a miscarriage does not occur, such children are born premature and suffer from anemia (anemia) and jaundice. This condition is called hemolytic disease of the newborn (hemolysis - destruction of red blood cells). It can lead to the death of a child.
Thus, early examination of the mother and fetus for Rh status helps prevent Rh conflict and the death of the newborn.
Sources:
- Mineeva N.V. Human blood groups. Fundamentals of immunohematology. - St. Petersburg. 2004. 188 p.
- Dutkevich I.G. Practical guide to clinical immunohematology (group antigens and antibodies of human blood, blood groups and their clinical significance, methods of immunohematological research). — St. Petersburg: SpetsLit, 2018. 159 p.
- Connie M. Westhoff. The Structure and Function of the Rh antigen Complex. Semin Hematol. January 2007; 44(1): 42–50.
- Pegoraro V, Urbinati D, Visser GHA, Di Renzo GC, Zipursky A, Stotler BA, et al. (2020) Hemolytic disease of the fetus and newborn due to Rh(D) incompatibility: A preventable disease that still produces significant morbidity and mortality in children. PLoS ONE 15(7): e0235807.
The most basic thing about the concept of blood group
The child's blood depends on the parents and is inherited with the so-called ABO gene, which is located on chromosome 9. The following table will show how likely it is that a group will be taken from its parents.
| Parents' blood types | Heritable blood type in a child as a percentage | ||||
| I | II | III | IV | ||
| I and I | 100% | — | — | — | — |
| I and II | 50% | 50% | — | — | |
| I and III | 50% | — | 50% | — | |
| I and IV | — | 50% | — | 50% | |
| II and II | 25% | 75% | — | — | |
| II and III | 25% | 25% | 25% | 25% | |
| II and IV | — | 50% | 25% | 25% | |
| III and III | 25% | — | 75% | — | |
| III and IV | — | 25% | 50% | 25% | |
| IV and IV | — | 25% | 25% | 50% | |
With 100 percent probability we can say which blood type will be passed on to the baby if they both have the first.
Problem filter
I heard that the problem of Rh sensitization can be solved with the help of plasmapheresis. But can pregnant women do this?
Margarita, Yaroslavl
– Not only is it possible, but it is also necessary! By removing antibodies that are harmful to the fetus from the bloodstream or reducing their concentration, plasmapheresis (blood purification method) is a very effective prevention of Rh conflict. True, if a woman has so-called complete antibodies in her blood, which are slowly synthesized and more difficult to pass the placental barrier. It is much more difficult to “pull out” a pregnancy with incomplete antibodies: they are synthesized in 10–14 hours, and it is impossible to “cleanse the blood” every day. Minimum – in 1–1.5 days. In order to maintain a normal antibody titer, some women have to undergo this procedure throughout their pregnancy.
Plasmapheresis has become a real lifesaver in the treatment of toxicosis in the first and second half of pregnancy, as well as in placental insufficiency, which is the main cause of intrauterine hypoxia (oxygen starvation) and fetal growth retardation.
Sensations in the world of medicine
I would like to mention one, the only (!) scientifically recorded case. After a liver transplant, a fifteen-year-old Australian woman completely changed all her immune system parameters, and her Rh changed from “minus” to “plus.” However, the blood type remained the same, first.
In my opinion, it is also worth mentioning one scientific study that promises to be sensational. Brazilian scientists, in the course of a series of experiments, discovered that during liver and spleen transplantation (with the coincidence of many additional conditions, of course), the protein found in red blood cells can change. This means that a change in rhesus during life is possible. Moreover, the blood type always remains the same.
Thus, this theory is slowly acquiring scientific background. But there is still no conclusive evidence to support it.
That's all. What blood secrets do you know? Share your life situations. We are always happy to communicate.
See you again!
The influence of genetics on the Rh factor
It is now reliably known that the Rh factor in humans is determined by genetics. A pair of genes is considered: D positive and d negative. They can be the same type of components DD or dd (the so-called homozygous pair of genes) and different components, for example Dd (heterozygous), where D is dominant in this case and whether the Rh factor is positive depends on it. It is these genes that are inherited. They are the reason for the birth of a baby with Rh negative from parents who have Rh positive.
The inheritance table below shows all possible predictions of a child's Rh factor, depending on what the parents' Rh factor is:
| Rh factors of parents | Rh factor of the child | ||
| mothers | father | (Rh+) | (Rh-) |
| Rh+ | Rh+ | 50% | 50% |
| Rh+ | Rh- | 50% | 50% |
| Rh- | Rh+ | 50% | 50% |
| Rh- | Rh- | — | 100% |
As can be seen from the table, if two parents are Rh negative, then the child will be born with a negative Rh factor; in other cases, it all depends on how the genes are inherited.
General principles of inheritance of characters.
Simply put, every trait in the body (hair color, eye color, blood type, Rh factor) is encoded by two genes.
In reality, the number of genes that determine the trait is much greater. For each trait, the child receives one gene from the mother, another from the father. In genetics, dominant and recessive genes are distinguished. The dominant gene is designated by a capital letter of the Latin alphabet, and in its presence the recessive gene, as a rule, does not manifest its properties. A recessive gene is indicated by a capital letter of the Latin alphabet. If for some trait an organism contains two identical genes (two recessive or two dominant), then it is called homozygous for this trait. If an organism contains one dominant and one recessive gene, then it is called heterozygous for this trait, and at the same time those properties of the trait that are encoded by the dominant gene are manifested. For example: A is a dominant gene that determines brown eye color and A is a recessive gene that determines blue eye color
Possible genotype options: AA - homozygote, brown eyes Aa - heterozygote, brown eyes aa - homozygote, blue eyes
Example 1:
wife AA - homozygous, brown eyes, both genes are dominant; husband AA - homozygous, blue eyes, both genes are recessive
When germ cells (egg and sperm) are formed, one gene goes into each germ cell (gamete), i.e. in this case, the female body forms two gametes containing one dominant gene each, and the male body forms two gametes containing one recessive gene each. When germ cells merge, the embryo receives one maternal and one paternal gene for this trait.
wife AA + husband aa Gametes: A A a a Child: Aa Aa Aa Aa
Thus, in this situation, 100% of the children will have brown eyes and be heterozygotes for this trait.
Example 2:
wife Aa - heterozygote, brown eyes husband Aa - heterozygote, brown eyes wife Aa + husband Aa gametes: A a A a child: AA, Aa, Aa, aa
In this case, the probability of having children with brown eyes (homozygotes) is 25%, heterozygotes are 50% with brown eyes, and blue eyes (homozygotes) are 25%.
Example 3:
wife Aa - heterozygote, brown eyes husband aa - homozygote, blue eyes Wife Aa + husband aa Gametes: A a a a Child: Aa, Aa, aa, aa
In this case, 50% of children have brown eyes and are heterozygotes and 50% have blue eyes (homozygotes)
Why might it change?
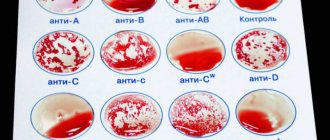
The group is determined by the adhesion of red blood cells. To do this, serum containing antibodies (agglutinins) α, β, α and β are dripped onto a special plate. Then a drop of blood is added to each, and there should be about ten times more serum. After this, the agglutination reaction (sticking together) of red blood cells is observed under a microscope for five minutes. Based on the results of this reaction, the blood type is determined:
- if gluing did not occur in any serum, then it is I;
- if the reaction is positive with sera containing α and α+β antibodies, then this is II;
- if agglutination occurred in serum with antibodies β and α+β, then this is III;
- if all sera give positive results, this means that the blood contains both antibodies and belongs to type IV.
Blood group determination
Why might the group change? To do this, it is necessary that red blood cell antigens cease to be produced or their production is greatly weakened. There is an opinion that this can happen with infectious diseases, pregnancy, tumors, and some diseases associated with increased production of red cells. In this regard, in laboratory tests, antibodies cannot detect such a small amount of antigens or the reaction is so weak that it is not visible. Thus, under certain conditions, a temporary change in test results is possible, but not a change in group membership.