Multifocal atherosclerosis is a chronic metabolic disease in which fat (lipoproteins, triglycerides) are deposited on the inner wall of the arteries. In the initial stages, the disease is not dangerous, but then these substances form plaques and can cause thrombosis and thromboembolism. Atherosclerosis can affect the aorta, arteries of the heart, brain and limbs, as well as vessels that supply blood to internal organs (kidneys, intestines). It is called multifocal in the presence of several pathological foci, which can be located in any area. It is important to diagnose the disease in time, while its development remains in the early stages - complicated forms either cannot be corrected or require surgical intervention.
Causes and risk factors
Atherosclerosis is one of the most common diseases of the cardiovascular system. The incidence rate ranges from 182 (France) to more than 800 people (Russia) per 100 thousand population. This depends, first of all, on nutrition and the presence of bad habits, on the degree of environmental pollution and other factors. The risk of developing this disease especially increases in the presence of one or more factors:
- bad habits, especially smoking;
- overweight and insufficiently active lifestyle;
- chronic increase in blood pressure;
- consumption of foods high in animal fats;
- diabetes;
- endocrine system disorders and others.
REFERENCE! Cholesterol is found in large quantities in animal fats that undergo heat treatment. It is its components that can be deposited on the inner surface of blood vessels.
Theories of the development of atherosclerosis
Doctors are working to determine the exact cause why multifocal atherosclerosis develops. There are several theories that explain the primary origin of the disease and the mechanism of its development. These include:
- lipoprotein infiltration – accumulation of fats in the walls of blood vessels;
- endothelial dysfunction – deposits are formed due to the weakness of the inner lining of blood vessels and a decrease in its protective properties;
- autoimmune – disruption of the immune system, including increased synthesis of macrophages and leukocytes;
- peroxide – the influence of free radicals and lipid peroxidation reactions, in which cell death occurs;
- hormonal - when the level of certain hormones decreases, the accumulation of cholesterol necessary for their synthesis increases.
And mixed theories of the development of atherosclerosis are also popular. They imply that the disease develops when several factors combine simultaneously, and their results are the destruction of vascular walls.
Multifocal motor neuropathy (MMN)
Multifocal motor neuropathy (MMN) (information for patients and doctors)
What is Multifocal Motor Neuropathy?
- “Multifocal” means multiple lesions.
- “Motor” - that the pathological process involves exclusively the motor fibers of the nerves responsible for muscle strength and the execution of movements.
- “Neuropathy” is damage to the peripheral nerves.
How common is this disease in the population? This is a very rare disease. The incidence of MMN in the population is only 1–2 cases per 100,000 population; is diagnosed 3-4 times more often in men, and the onset (onset) of the disease occurs in working age (20-50 years).
What is the mechanism of development of this disease? MMN is a chronic multiple motor neuropathy , the development of which is based on an autoimmune process, when components of the immune system mistakenly begin to work against the structures of their own body. MMN is based on selective dysimmune damage to the nodal zones of motor nerves - areas of thick nerve fibers rich in ion channels and responsible for the transmission of nerve impulses. As a result of such a lesion, a block in the conduction of excitation along the motor nerve develops and movements are impaired.
What worries patients with this disease?
- asymmetrical muscle weakness in the arms or arms > legs
- There is no pain or sensory disturbances!
MMN begins in most patients with the gradual development of muscle weakness, most often in the arms. Sensory impairment and pain are absent. The initial complaint may be weakness in one arm or arms; much less often, the disease begins in the legs. Weakness in the distal arms (hands) is common and is found in approximately 95% of patients with MMN. More than half of patients experience muscle spasms and twitching. There is no damage to the motor cranial nerves responsible for eye movement, facial muscles, chewing, swallowing and speech. Pelvic functions are not impaired. The course of the disease is slowly progressive or wavy in nature. Muscle wasting (hypo- or atrophy) is uncommon and is present in late stages of the disease, often in untreated patients. There are no signs of damage to the central nervous system.
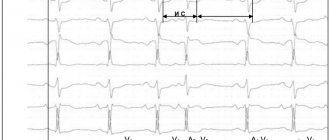
On what basis is the diagnosis made and what examinations can be prescribed for me to confirm it? Currently, clear criteria for the diagnosis of “Multifocal motor neuropathy” have been developed (EFNS/PNS 2011). According to these criteria, an analysis of the history of the development of the disease, a neurological examination and electroneuromyography are sufficient:
- Electroneuromyography makes it possible to detect conduction blocks along the motor fibers of peripheral nerves in places atypical for their compression (outside the tunnels), while the study parameters of sensory fibers are unchanged. In addition, this study excludes damage to other structures of the peripheral neuromotor apparatus (motor neurons, muscles).
- Additionally, neuroimaging may be required - ultrasound of peripheral nerves and MRI of the brachial plexuses with contrast, which are also highly informative and help confirm the diagnosis and exclude other pathologies.
However, in practice, difficulties may arise in making a diagnosis when patients come for consultation years after the onset of the disease with severe motor impairment, muscle atrophy, or an atypical form of the disease. In these situations, a differential diagnosis is required.
When carrying out a differential diagnosis, the list of examinations expands:
- routine laboratory tests of blood and urine, MRI of the spine and spinal cord do not help in making the diagnosis of MMN, but will exclude possible other causes of multiple nerve damage (such as diabetes mellitus, rheumatoid arthritis, vertebrogenic myelopathy, Hiroyama disease, etc.)
- blood test for antibodies to peripheral nerve gangliosides - antibodies to GM1 gangliosides are present in approximately half of cases of MMN
- genetic blood test for mutations of the PMP22 gene - will exclude possible hereditary causes of neuropathy
- etc.
Of course, not all of these examinations are always prescribed. In most cases, only an ENMG study is sufficient. It should be emphasized that the ENMG study must be carried out by a well-trained and experienced specialist in a high-class myorapha. Methodological errors and insufficient size of this study often lead to erroneous diagnoses. Therefore, we recommend performing ENMG in our center.
What treatment is there? MMN is a chronic disease, complete cure is impossible. But effective treatment has now been developed that can control the disease. Intravenous immunoglobulin (IVIG) therapy is the only treatment for MMN that has been shown to be effective in controlled studies.
The effective dose is 2 g of IVIG per 1 kg of patient weight (dose administered over 3-5 days). The vast majority of patients respond positively to this therapy. However, the improvement is short-term and long-term maintenance therapy is required: periodic infusions of IVIG drugs - 1 g of IVIG drug per 1 kg of patient weight every 3-4 weeks (administration 3 days before) or administration of 2 g of the drug per kg of weight every 1-2 months (introduction in 3-5 days).
It should be remembered that not all IVIG drugs are suitable for the treatment of MMN. The main requirements for human immunoglobulin preparations are:
- safety of the drug with respect to transmission of infection;
- IVIG should be well tolerated;
- the IgG content must be at least 95% of the total IgG content;
- IgA content should be minimal;
- the drug should not exhibit thrombogenic (procoagulant) activity;
- possibility of high-dose therapy (no daily dose limitation);
- preference is given to 10% solutions.
Contraindications to IVIG therapy are hypersensitivity (allergy) to IVIG components, as well as IgA deficiency. Therefore, before treatment, a study of IgA levels is recommended. If its deficiency is detected, treatment is carried out with caution, in particular, premedication and special preparation are used. In the absence of therapy, irregular administration of IVIG, or treatment with insufficient doses of the drug, motor deficits can slowly, steadily, and irreversibly progress due to secondary axonal damage.
Glucocorticosteroids and plasmapheresis are ineffective in patients with MMN!
What is the prognosis for this disease? Approximately 80% of patients respond to IVIG treatment. MMN does not lead to death, since the muscles involved in the acts of swallowing and breathing are not involved in the pathological process. Because MMN primarily affects the muscles of the hands, writing and fine motor skills may be limited. In this regard, alternative professional employment options should be considered.
There are 40 patients with MMN under the supervision of cPNS specialists. We are able to diagnose this disease and determine the optimal personalized treatment regimen with IVIG drugs.
Employees of the Center for Peripheral Nervous System Diseases provide consultations to patients on an outpatient basis within the framework of compulsory medical insurance and on a commercial basis. Make an appointment,
Be healthy!!!
Mechanism of disease development
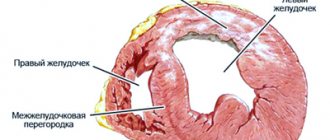
The process of development of atherosclerosis is called atherogenesis. It consists of several successive stages, as a result of which the vessel loses strength and elasticity. Normally, its wall consists of smooth muscles, and the inside is lined with intima - a single-layer membrane of endothelium. Each of the layers plays its own role, and together they provide the ability of the vascular wall to stretch and contract. With atherosclerosis, tissues become saturated with harmful deposits, and plaques can additionally form on the inner surface of the vessel.
- Accumulation of fat cells. At the first stage of the disease, lipid stains are found on the inner surface of the arteries. Only low and very low density lipoproteins participate in their formation, and their other types do not have atherogenic activity. These compounds form bonds with the components of the intercellular substance and remain in the form of single spots.
- Activation of leukocytes and formation of xanthoma cells. In the area of the lipid stain, the migration of leukocytes, especially lymphocytes and monocytes, increases. Further, monocytes play a major role in the development of atherosclerosis. In the vascular intima they transform into macrophages and participate in the formation of xanthoma (foam) cells.
- Pro- and antiatherogenic factors are compounds that can accelerate and slow down the development of atherosclerosis. Macrophages release cytokines and growth factors. They enhance the division of vascular smooth muscle cells and intercellular substance, which is used as a building material for atherosclerotic plaques. Next, there is a decrease in the processes of synthesis of smooth muscle cells and collagen, which ensures the density and elasticity of the vascular wall.
- The role of smooth muscle cells. They represent the inner lining of the artery wall, and they are synthesized by the intercellular substance. Their proliferation becomes the main point in the development of atherosclerotic plaque. If normally the tissue is capable of contracting and lengthening many times over, in the obvious stages of the disease this ability is lost, the vessels become fragile and brittle.
- Formation of a complicated plaque. This formation begins to gradually sprout with its own vessels. They cause hemorrhage, thrombosis and thromboembolism - a dangerous condition in which the plaque enters the lumen of the blood vessel and circulates with fluid flow.
IMPORTANT! Not every lipid stain goes through all stages of development and transforms into atherosclerotic plaques. However, these processes are interconnected, and the disease can progress.
Atherosclerosis is an acquired disease, the development of which is influenced by lifestyle and bad habits.
Symptoms
Multifocal atherosclerosis develops in stages. It is difficult to diagnose in the early stages, since clinical changes are visible only on test results. The patient has no complaints. In the future, they depend on the type of artery affected.
- With atherosclerosis of the arteries that participate in the nutrition of the myocardium, chest pain, heart rhythm disturbances, and coronary artery disease occur. The patient experiences severe pallor of the skin and mucous membranes, shortness of breath, and trembling of the limbs. These symptoms are especially worse after exercise.
- With atherosclerosis of the arteries of the brain, there is a decrease in performance, deterioration of hearing and vision. In addition, the disease often causes strokes, which are life-threatening and require emergency medical attention.
- Atherosclerosis of the extremities (usually the lower ones) leads to a deterioration in their blood supply. As a result, patients complain of severe pain in the legs, numbness and pins and needles sensation, cramps and trophic ulcers. In the initial stages, the clinical picture is mild and worsens only after prolonged physical activity, and in advanced stages it can even appear during sleep. A typical sign of atherosclerosis of the lower extremities is intermittent claudication, in which the patient experiences pain alternately in the right and then in the left leg.
Advanced forms of multifocal atherosclerosis are accompanied by acute pain. In addition, the formation of aneurysms is observed - pathological dilations of blood vessels, which are formed as a compensatory reaction of the body to insufficient blood circulation. In advanced stages they become noticeable under the skin. In these areas, the vascular walls are thin and fragile, so rupture of an aneurysm is a common and dangerous occurrence that poses a threat to the patient’s life. In areas that lack normal trophism, ulcers appear that do not respond to conventional treatment methods and may not heal for a long time.
Pathogenesis and clinical manifestations
The basis of atherosclerosis is the formation of thickenings of the inner lining of the arteries - the so-called plaques. They consist of an accumulation of cholesterol, proteins, dead immune cells and overgrown smooth muscle tissue. As a result, the lumen and elasticity of the vessel are significantly reduced. All this leads to a decrease in blood flow in it. Due to disturbances in blood rheology and the hemostasis system, blood clots can form on atherosclerotic plaques, which subsequently causes final blockage of the artery. This happens especially often in the lower extremities, where blood flow is very slow.
Since the process of formation of atherosclerosis is very long, symptoms may not appear at first. Another reason for such a hidden picture is the development of collaterals, bypass routes of blood supply, with the help of which the body independently tries to cope with the restriction of blood flow.
Unlike classic atherosclerosis, multifocal atherosclerosis produces many more manifestations because it affects several vessels at once. Against the background of its course, the following may develop:
- coronary heart disease (narrowing of the lumen of the coronary arteries);
- stroke (both hemorrhagic, due to high blood pressure, and ischemic, due to blockage by a blood clot);
- angiopathy of the legs, which can lead to amputation;
- intestinal ischemia;
- nephropathy;
- visual impairment.
Diagnostic methods
Diagnosis of multifocal atherosclerosis is an important stage, thanks to which it is possible to determine the localization of the pathological focus and the stage of the disease. For this purpose, instrumental and laboratory techniques are used to monitor the condition of blood vessels. These include:
- initial examination and medical history, identification of typical symptoms;
- palpation (palpation) of all superficial arteries located under the skin, as well as listening to them in areas accessible for diagnosis;
- determining the degree of filling of blood arteries and their integrity;
- blood test with mandatory determination of various types of fats and their percentages, including cholesterol;
- radiography, ultrasound examination – basic techniques;
- Dopplerography is an assessment of the conductivity of blood vessels at any part of their passage, using a contrast agent.
When diagnosing atherosclerosis, it is important to determine the location of the pathological area. And also in the process it is possible to differentiate this disease from many chronic diseases of the heart and blood vessels, which manifest themselves with a similar set of symptoms.
Obliterating atherosclerosis of leg vessels
Treatment
Treatment of multifocal atherosclerosis and its duration depend on the stage of the disease. A mandatory step will be the correction of lifestyle and nutrition. It is not always possible to return the vessels to their previous condition, but they can be maintained in the same condition for many years.
Non-drug methods
The most important stage of atherosclerosis treatment takes place at home. It includes following all the recommendations of doctors, thanks to which you can establish fat metabolism and prevent further deposition of lipids on the inner wall of blood vessels. Treatment at home consists of several stages:
- nutrition correction - exclusion of animal fats, especially during heat treatment of other products;
- giving up bad habits, including smoking and drinking alcohol;
- normalization of body weight;
- physical activity that will correspond to the state of health - it is better to check with your doctor what loads you can bear with atherosclerosis.
Without following simple rules, treatment of multifocal atherosclerosis is not possible. It is important to understand that they will have to be carried out throughout your life. Since poor diet and smoking are considered the main predisposing factors to atherosclerosis, it is important to give up habits to slowly restore all biochemical processes.
Drug treatment
Drugs for the treatment of multifocal atherosclerosis are aimed simultaneously at several targets. They participate in lipid metabolism and gradually normalize it, but they should be taken regularly. The selection of drugs is carried out individually, taking into account the diagnostic results. Four main groups of drugs are used to treat this disease:
- drugs that prevent further absorption of cholesterol;
- substances that inhibit the synthesis of lipoproteins in the liver, thereby reducing their concentration in the blood;
- means for processing and rapid removal of atherogenic compounds;
- additional medications, including agents to strengthen the inner surface of blood vessels.
REFERENCE! Treatment can be carried out at home. However, its timeliness and gradualism are important. Those remedies that will help in the early stages of the disease will be ineffective at further stages.
Surgery
The operation is prescribed for patients diagnosed with vascular aneurysms or other pathologies that are not amenable to conservative treatment. One of the common types of surgery is the removal of a section of a vessel, especially if it has an aneurysm. If previously the process required full access, now operations are easily carried out under the control of an endoscope.
Multifocal atherosclerosis is a dangerous disorder that gradually progresses and can lead to dangerous consequences. The disease occurs with a violation of fat metabolism and has several pathological foci. Treatment must be timely to avoid complications and the need to perform surgery to remove the affected vessel.
Causes
The exact cause of the development of multifocal motor neuropathy has not yet been established. However, the disease is thought to be immune-mediated because an impressive number of MMN patients develop autoaggressive antibodies that target specific peripheral nerve lipids (GM1 gangliosides). The role of these antibodies in the occurrence of MMN has not been fully studied - it has not yet been established whether they are the main provoking factor or, on the contrary, a “by-product” of the course of the disease.