Nowadays, it’s rare for anyone to boast of healthy blood vessels in their legs. At the end of the working day, the legs begin to ache tiredly, buzz and ache, veins treacherously bulge on the skin and more and more spider veins appear.
Spider veins (telangiectasia) are dilated intradermal capillaries that form a “star” on the skin. The appearance of spider veins is a signal that you need to strengthen your blood vessels. Unfortunately, this is not just a cosmetic defect, but a manifestation of the initial stage of varicose veins and a serious reason to consult a phlebologist and treat blood vessels in the legs.
Types of spider veins
Telangiectasia can be different in color (red and blue), shape (vascular formations in the form of a “tree”, “mesh”, “star”, “spider”), localization (formed both on the face and body).
Red linear telangiectasias most often form on the face (on the nose and cheeks).
On the legs there are red or blue linear and tree-shaped spider veins, which are formed due to the bursting of blood vessels in the legs. Spider telangiectasias are usually red in color and occur on the back or abdomen
In women with spider veins on the legs, vascular formations are most often located in groups (on the inner side of the thigh they are located parallel to each other and have a linear appearance, and on the outer side they are circumferential and have a “tree-like” shape).
Causes of the disease
Spider veins appear due to the fact that intradermal capillaries lose their tone. There are many reasons for this:
- Pregnancy, postpartum period (often “stars” appear due to hormonal imbalance and compression of the pelvic vessels);
- hormone therapy;
- varicose veins;
- hereditary predisposition;
- hypertension (high blood pressure dilates the capillaries);
- chronic liver diseases;
- excessive physical stress;
- abuse of the sun, solarium, sauna, bath;
- alcohol abuse;
- prolonged load on the legs in a vertical position, etc.
Spider veins appeared on the legs
Spider veins, or telangiectasia, are a persistent dilatation of small vessels of a non-inflammatory nature.
Not only small veins can be affected, but also arteries and capillaries. They differ in color: dilated arterioles and capillaries are red and do not stand out above the surface of the skin. Dilated veins have a bluish tint and may protrude slightly. The stars are usually localized on the inner and back of the thighs, calves and ankles (but can also be on other parts of the body, in particular on the face). Over the age of 75, about 70% of the population suffers from this disease, however, among young people under 45, about a third note the appearance of a fine network of blood vessels on the legs.
The diameter of the dilated vessels does not exceed 1 mm. The configuration of the “stars” can be very different - actually star-shaped, tree-shaped, or in the form of several parallel thin lines or spots. All these formations, regardless of form, are of a similar nature.
Spider veins do not cause discomfort: they do not cause pain or other unpleasant sensations. This explains why patients go to the doctor only when small vessels on the legs become an “aesthetic” problem: for example, before the summer season. Meanwhile, a visit to a phlebologist should not be postponed if spider veins appear on the legs.
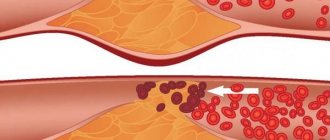
Bleeding from varicose veins
Poor circulation can lead to varicose veins with the formation of blood clots. If the disease is not treated, complications will invariably arise that can be life-threatening. Along with varicose veins, varicose veins are formed - bubbles that have an uneven shape. Deformation and thinning of the wall of varicose veins often lead to the development of bleeding from varicose veins at the slightest trauma to the vessels. Bleeding from varicose veins occurs daily in patients in European countries, Moscow and the Moscow region. Leading specialists of both public and private city phlebological centers weekly face the problem of bleeding from varicose veins. Innovative technologies can easily prevent bleeding from varicose veins, but even the most advanced medical innovations are sometimes unable to save a person’s life if precious time is lost.
Bleeding from varicose veins
Reasons for the appearance of stars on legs
The main cause of spider veins on the legs is hormonal imbalance, including those caused by taking oral contraceptives. This explains why telangiectasia affects more women than men. Other reasons include the following:
- genetic predisposition
- pregnancy
- chronic skin diseases, including rosacea
- overweight
- increased load on the legs
- excessive exposure to solar radiation
- hypertension
- endocrine pathologies
- chronic venous insufficiency
- bad habits (in particular, smoking) and others.
Bleeding from varicose veins. Emergency measures in case of bleeding from varicose veins
- Call an ambulance. In such cases, you should never leave a sick person at home. You cannot predict exactly how much blood loss will occur. In some cases, it can be so great that failure to provide medical care can lead to death.
- Before the ambulance arrives, it is better to try to stop the bleeding yourself. In this case, there is no need to apply a very tight bandage (the bleeding is venous, not arterial), it is enough just to bring the leg with the injured varicose vein to a position that will be above the level of the body, and secure the wound well with a gauze bandage or an elastic bandage.
- Blood loss can cause dizziness and loss of consciousness, so it will be better if the victim takes a lying position and does not make sudden movements.
In advanced stages of varicose veins, the threat of the risk of developing venous bleeding is constantly present and it would be good to remember this.
Methods to stop bleeding from veins
Most bleeding from varicose veins is not life-threatening. But some of them, especially in the presence of concomitant diseases, can be extremely dangerous. In some cases, the leading and best specialists in Moscow and the Moscow region will not be able to help you.
Why are varicose veins dangerous?
To this question, most of us will probably answer that spider veins are purely an aesthetic problem. Indeed, you no longer want to wear a short skirt or shorts with veined stars. However, this is not the main thing.
A network of small vessels that appears on the skin may indicate that you are developing varicose veins. In particular, you may already have dilated reticular veins - superficial vessels that have a diameter of about 2 mm and feed the spider vein. In addition, a fine network of red or blue vessels may indicate the presence of chronic venous insufficiency - a set of symptoms that indicates poor circulation in the veins.
Causes of bleeding from varicose veins
The leading cause of bleeding from a varicose vein is its rupture, which can occur due to several circumstances:
- Mechanical damage. In this way, you can provoke a rupture of both those varicose nodes that are located outside and visible to the eye, and those that are located deeper.
- Thinning of the wall of the varicose vein. Often a complication of varicose veins is thrombophlebitis - inflammation of the venous wall. It thins out and becomes fragile. Therefore, when, without treatment, a varicose node increases in size, its wall simply cannot withstand the load and bursts.
Of course, bleeding from varicose veins is a manifestation of an advanced stage of varicose veins; therefore, in order to avoid such complications, it is necessary to promptly contact a good European phlebologist in Moscow, who will prescribe appropriate modern treatment. And it is better to find a specialist who knows innovative methods of treating veins for the most effective treatment. Only modern technologies today meet state European standards.
Varicose veins, which may cause bleeding from the veins
Treatment of spider veins on the legs
Spider veins require complex treatment: in most cases it takes place in two stages. The varicose veins feeding the sprocket should be removed first. This is done by sclerotherapy: during the procedure, a special drug, a sclerosant, is injected into the lumen of the vein, which “glues” it together. Thus, it is excluded from the bloodstream, its functions are taken over by other veins. Gradually the sclerotic vessel resolves.
After this, it’s time to remove the asterisk itself, for which doctors at the Phlebology Center use a neodymium laser. Its advantages are the ability to individually select the laser wavelength, as well as the precise, targeted effect of the laser beam on the vessel. The laser has the same effect on the veins as a sclerosant - it glues them together. As a result, small vessels disappear completely, and larger vascular formations, such as hemangiomas, become less noticeable.
For complete or almost complete removal of spider veins, a course of treatment of 2-4 procedures is required.
To make the treatment more effective, as well as to prevent relapses, patients should wear the recommended compression stockings after the procedure, which ensures correct pressure on the veins.
Symptoms
Before the venules appear, signs of a developing disease appear:
- patients complain of weakness and increased fatigue of the legs;
- pain appears, intensifying with pressure on the foot;
- swelling and local hyperemia cannot be excluded;
- itching occurs at the suspected site of formation;
- During the day there is discomfort in the lower extremities;
- increased frequency of seizures;
- sensation of running “goosebumps”;
- rarely numbness of the legs.
The branches that appear do not cause discomfort, however, some patients note an increased feeling of dryness of the dermis and itching.
If blood vessels rupture and a bruise forms, moderate pain on palpation, muscle tension and local hyperthermia are possible. The skin acquires a bluish tint, in the center of which there is a vascular branch.
Prevention
In order for the disease not to lead to serious problems, you should be able to prevent it. Doctors recommend following simple rules to prevent the formation of spider veins and damage to capillaries:
- harden the body;
- give preference to a contrasting shower;
- monitor your diet;
- wear comfortable shoes;
- dress according to the weather;
- do gymnastics to strengthen blood vessels;
- take vitamins;
- measure blood pressure;
- visit a manual specialist.
Simple tips will help prevent illness and strengthen the walls of blood vessels.
Diagnostics
To identify the disease, hardware diagnostic methods and tests are used to identify the cause.
Hardware methods include:
- ultrasound diagnosis of the lesion;
- duplex scanning of veins - used in cases of aggravated medical history and pronounced symptoms;
- Dopplerography - allows you to identify disorders of the circulatory system and blood supply;
- angiography is a high-tech method that determines the condition of the vascular wall and the lumen of the capillaries;
- capillaroscopy.
Tests to determine the cause of the disease:
- pinch method - most often used when the process is localized in the upper part of the body;
- the tourniquet method proposed by Troyanov;
- The hammer method is also applicable in the upper part of the patient’s body (chest, back).
By the nature of the formations at the site of mechanical impact, the cause and form of the pathology are judged.
A positive result is regarded as a basis for a detailed diagnosis. Also, for diagnostic purposes, the chemical composition of the blood and its ability to clot (hemostasis system) are examined.
Treatment of phlebitis
The first step to recovery is diagnosing the disease. Diagnosis is carried out by a phlebologist during a personal conversation with the patient and examination of the affected veins. Then the doctor prescribes a set of examinations to recognize the type of phlebitis and formulate a treatment strategy suitable for the patient.
A set of examinations may consist of different procedures. And it is compiled depending on the condition of the patient’s blood vessels and his overall health. For example, general and biochemical blood tests, blood coagulogram, ultrasound of blood vessels, MRI of the affected limb.
The second step of treatment depends on the form of the disease. Treatment of phlebitis of the superficial veins is carried out on an outpatient basis. Severe stages requiring surgery are treated with hospitalization. In this case, the patient spends 24 hours in the Vascular Center: 2 hours before the operation to prepare, during the operation and time for observation after the operation.
Complex forms are treated surgically. The following types of surgical intervention are used:
- crossectomy - ligation and removal of a vein;
- thrombus extraction - removal of blood clots;
- thrombolysis therapy - restoration of blood flow in the vessel due to the dissolution of the blood clot;
- installation of a vena cava filter - a device for catching blood clots.
Mild forms are treated with medication. The patient is prescribed:
- antibacterial drugs (for infectious phlebitis);
- anti-inflammatory drugs;
- ointments, gels with heparin;
- drugs to improve blood microcirculation:
- disaggregant - prevent the formation of blood clots;
- antihistamines, if the patient is allergic to drugs;
- glucocorticosteroids - prevent joint destruction.
The complex of drugs depends on the form of the disease. Treatment is also accompanied by wearing compression hosiery and mechanotherapy (the use of special devices and simulators to increase the functionality of the patient’s limbs).