1.General information
Periarteritis nodosa was first described by Adolf Kussmaul and Rudolf Mayer in 1866, and to this day is often called Kussmaul-Mayer disease in the literature. You can also find the names “polyarteritis”, “panarteritis”, “systemic necrotizing vasculitis”, etc.
This is an inflammatory process that primarily affects small and medium-sized arteries (arterioles). With the development of the process, pronounced pathological changes occur in all layers of the vascular walls; Accordingly, circulatory function suffers more and more, and the greatest danger is no longer vascular pathology itself, but circulatory disorders in vital organs caused by fibrosis.
According to available epidemiological data, the disease is most often detected in the age range from 30 to 60 years. Among those affected, approximately three times more men than women.
A must read! Help with treatment and hospitalization!
Publications in the media
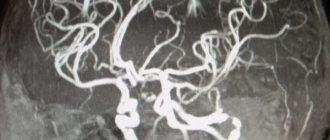
Polyarteritis nodosa (UP) is a disease of small and medium-sized arteries with the formation of microaneurysms and secondary damage to organs and tissues. Statistical data. Prevalence: 0.7–6.3 per 100,000 population. Average age 38–43 years. Men over 40 years of age get sick 3 times more often. Etiology • Hepatitis B viruses (30–80% of cases, at any stage of hepatitis without correlation with its activity) and C • HIV • Parvovirus B19 • HTLV • Drugs (sulfonamides, penicillins, iodides, thiouracil, bismuth preparations, thiazide diuretics, guanitidine) • Very rarely, secondary UP develops against the background of rheumatoid arthritis or Sjögren's syndrome. Pathogenesis. The mechanism of damage to the vascular wall in UP is not clear. Damage to muscular arteries is typical with the development of necrotizing panvasculitis, and the formation of aneurysms is possible. The consequences of vasculitis are heart attacks, hemorrhages, and scars. Inflammation of blood vessels is accompanied by a violation of the rheological properties of blood, thrombosis, and disseminated intravascular coagulation syndrome.
Clinical picture • General manifestations •• Fever •• Myalgia, most often in the calf muscles •• Loss of body weight (up to cachexia) correlates with the activity of the process. • Transient migratory arthritis of large and medium-sized joints, without deformities. • Kidney damage •• Isolated urinary syndrome: proteinuria, microhematuria, leukocyturia (not associated with infection) •• Arterial hypertension: in the early stages it is associated with renal vasculitis or renal infarction, in the later stages - with glomerular damage; hypertensive syndrome often acquires malignant features •• Rupture of renal artery aneurysms with the development of perinephric hematoma (rare). • Damage to the nervous system •• Combinations of peripheral neuritis of the tibial, ulnar, radial, sural nerves. Features of polyneuritis in UP: asymmetry, predominance of motor disorders, severe pain syndrome •• Guillain-Barré syndrome •• CNS: cerebral infarctions, convulsions, psychoses. • Damage to the cardiovascular system •• Arrhythmias •• Coronaryitis with ischemic syndrome, possible MI, often painless •• Heart failure. • Skin •• Hemorrhagic purpura •• Nodules (aneurysmal changes in the arteries) •• Livedo reticularis (“marbled skin”). • Abdominal syndrome is a consequence of vasculitis of the abdominal vessels •• Pancreatitis •• Perforation of small intestinal ulcers •• Necrosis of the gallbladder. • Orchitis, epididymitis (more often with HBV-associated UP). • Eye damage: conjunctivitis, iritis, occlusion of the central retinal artery. • Lungs (rare): pulmonary vasculitis, interstitial pneumonia.
Laboratory data • Blood test: increased ESR, leukocytosis, thrombocytosis, increased urea concentration in the blood serum, anemia (rare) • Urine test: proteinuria, hematuria • Test: Hepatitis B Ag (50% of cases); RF in low titer or absent; ANAT in low titer or absent; hypocomplementemia with kidney or skin damage. Instrumental data • Biopsy is twice as informative from areas of affected skin or muscles • X-ray of joints: no changes • Visceral angiography - microaneurysms of the affected arteries. Diagnostic tactics . The nosological uniqueness of the clinical picture of UP is given by asymmetric motor polyneuritis, multiple organ symptoms (coronaryitis with the development of painless MI, specific forms of damage to the kidneys and gastrointestinal tract, etc.). Diagnostic criteria (American Rheumatological Association, 1990) • Weight loss of more than 4 kg, not associated with other causes • Livedo reticularis • Testicular pain not associated with infection, trauma or other causes • Myalgia (weakness or tenderness in the muscles of the lower extremities) • Mononeuritis, polyneuropathy or a combination of mononeuritis • Diastolic blood pressure above 90 mmHg • Increased serum creatinine concentration more than 132.5 µmol/l, not associated with dehydration or urinary tract obstruction • Presence of HBV markers in the blood • Changes detected by arteriography : aneurysms or occlusion of visceral arteries not associated with atherosclerosis, fibromuscular dysplasia and other non-inflammatory diseases • Histological examination of small and medium-sized arteries demonstrates granulocytic and mononuclear infiltration of the arterial walls. To make a diagnosis, 4 criteria must be met. Sensitivity 98.9%, specificity 95.2%. Differential diagnosis • Microscopic polyarteritis (kidney damage without arterial hypertension, but with rapid development of renal failure, sometimes with nephrotic syndrome; biopsy reveals capillary damage) • Wegener's granulomatosis (with UP there is no ulcerative necrotizing rhinitis, sinusitis, laryngitis) • Churg's syndrome –Strauss: bronchial asthma, fever, eosinophilia >10%, mononeuritis or polyneuritis, migrating pulmonary infiltrates, biopsy shows perivascular infiltrates containing eosinophils. Complications • Gangrene of the extremities • Infarction of internal organs • Intraorgan bleeding due to rupture of aneurysms.
TREATMENT General tactics Immunosuppressive therapy is necessary; its absence worsens the 5-year survival prognosis by 8 times. However, immunosuppressive therapy complicates the sanogenetic immune response in the setting of HBV infection, which requires a special approach to this group of patients. Diet. Cyclophosphamide should be prescribed while taking large amounts of fluid to prevent the development of hemorrhagic cystitis. Drug treatment • GCs are used in high doses. Initial pulse therapy with methylprednisolone (1 g/day IV for 3 consecutive days) is proposed, followed by a transition to prednisolone 1 mg/kg orally daily until the onset of clinical effect (on average for 1 month). The dose is then gradually reduced to maintenance (10 mg/day) and then completely discontinued (total treatment duration is 12–24 months and may be shorter if GCs are used in combination with immunosuppressants. • Cyclophosphamide is preferably used intravenously in an individually tailored regimen according to 0.5–2.5 g 1 r/week or 1 r/month (for example, 0.6 g/m2 monthly for a year). When choosing a dose, they are guided by the state of renal function and the viability of the bone marrow. Development of side effects of cyclophosphamide (bladder cancer, hemorrhagic cystitis, infertility, bone marrow suppression) correlates with the total dose. During treatment with cyclophosphamide, especially in combination with GC, the likelihood of developing secondary infections is high. • For cases of HBV-dependent UP, the use of prednisolone in a dose of 1 is proposed mg/kg/day for 1 week, rapid withdrawal during the second week and subsequent antiviral therapy •• recombinant IFN - in courses of 12 weeks or continuously for a year • NSAIDs - for joint syndrome. • ACE inhibitors, for example captopril 75-150 mg/day, enalapril 20-40 mg/day - in the presence of arterial hypertension, provided there is no stenosis of the renal arteries. Non-drug therapy . Plasmapheresis is indicated for refractory UP, HBV-dependent UP and patients on hemodialysis. Surgical treatment is indicated for the development of renal failure (nephrectomy, donor kidney transplantation) and thrombosis of the mesenteric arteries. Forecast. Unfavorable prognostic factors • serum creatinine level >140 µmol/l • proteinuria >1 g/l • involvement of the gastrointestinal tract in the pathological process • cardiac damage • central nervous system symptoms. The greatest dangers are intestinal perforation and malignant arterial hypertension. Synonyms • Kussmaul-Mayer disease • Panarteritis nodosa • Periarteritis nodosa • Periarteritis nodosa • Polyarteritis nodosa. Reduction . UP - periarteritis nodosa.
ICD-10 • M30 Polyarteritis nodosa and related conditions
2. Reasons
The etiology and pathogenesis of Kussmaul-Meier disease remains unclear to this day - despite more than a century and a half of research history. The most likely cause today is considered to be an inadequate immune response (or an autoimmune attack on one’s own vascular walls) due to the presence of viruses - in particular, hepatitis B and C viruses, rubella virus, herpes virus, cytomegalovirus, etc. The hypothesis about the possible role of hereditary predisposition is also considered.
Proven risk factors include intoxication, taking medications and vaccines, hypothermia and exposure to intense solar radiation, infections - in general, any conditions that can provoke a surge in sensitivity and a violent (auto)immune response.
Visit our Dermatology page
Etiology
There is no clear cause of the disease. Currently, two main factors have been identified:
- drug intolerance;
- persistence of hepatitis B virus.
There are already about a hundred medications that have been associated with the occurrence of periarteritis nodosa.
In 30-40% of patients, hepatitis B surface antigen (HBsAg) or immune complexes including it, as well as other hepatitis B antigens (HBeAg) and antibodies to the HBcAg antigen, formed during viral replication, were detected in the blood. It is known that in France, the incidence of HBV-associated polyarteritis nodosa has decreased from 36% in the early 1980s to less than 5% in the 2000s, due to mass vaccination against hepatitis B.
Also, 5-12% of patients have hepatitis C virus, but its role in causing the disease has not yet been proven. Other viruses are also being considered: HIV, cytomegalovirus, Epstein-Barr virus, rubella, parvovirus B 19, human T-lymphotropic virus type 1, but their role has not yet been proven.
Separate observations have also been published on the occurrence of symptoms of polyarteritis nodosa after administration of a vaccine against hepatitis B and influenza.
Another suspected etiological factor is hereditary predisposition, but it has not yet been possible to establish a connection with a specific HLA antigen.
3.Symptoms
There are several clinical variants of periarteritis nodosa, which differ quite strongly from each other (cutaneous, asthmatic, etc.). Thus, the skin form with the formation of specific granuloma nodules, which gave the name of the disease, occurs only in 20-25% of cases and is distinguished by a significant variety of manifestations (marble pallor, pigmentation, rash of one or another nature, color and distribution). However, the further development of the clinical picture is determined by which internal organs suffer the most due to circulatory disorders, which in turn are caused by necrotizing fibrosis, thrombosis, and aneurysms. Typical is the formation of joint-muscular, cardiovascular, renal, pulmonary syndromes, often in combination with severe arterial hypertension, damage to the central nervous system and gastrointestinal tract, visual organs, and endocrine glands. In many cases, there is a febrile state that is practically not controlled by antibiotics or anti-inflammatory drugs.
The course of the disease also varies widely in different cases - from benign and slowly progressing to fulminant, with death a few months after manifestation.
The natural consequences of necrotizing fibrosis of arterioles include ischemia and infarction of internal organs, hemorrhages due to rupture of aneurysms, perforated ulcers, severe damage to the meninges, which sooner or later results in disability.
Symptomatically, periarteritis nodosa can imitate many diseases, so evidence-based diagnosis requires their exclusion. Differential diagnosis is carried out on the basis of clinical and laboratory criteria (microscopic analysis of skin samples is considered the most informative). Instrumental methods usually include Doppler sonography, angiography, and chest x-ray.
About our clinic Chistye Prudy metro station Medintercom page!
Clinical picture
The disease usually begins with general syndromes: constant fever, progressive weight loss, muscle and joint pain.
Fever occurs in 95-100% of patients, usually of the wrong type, unresponsive to antibiotics, but disappears with corticosteroids. As a rule, it disappears later, when organ pathology appears.
Weight loss with periarteritis nodosa is pathognomic. In some cases, body weight decreases by 30-40 kg in a few months, and the degree of cachexia is higher than in cancer.
Myalgia and, less commonly, arthralgia occur at the onset of the disease. They manifest themselves as characteristic pain in the calf muscles and large joints.
With the development of periarteritis nodosa, five types of organ pathologies are most common. They determine the specific clinical picture of the disease.
Renal vascular lesions occur in 75-90% of patients. The appearance of symptoms indicates a deep stage of the disease. Arterial hypertension usually develops, stable, persistent, leading to severe retinopathy and even loss of vision. Proteinuria (1-3 g per day), microhematuria, and occasionally macrohematuria are observed in the urine.
In some patients, the aneurysmally dilated vessel ruptures with the formation of a perinephric hematoma.
Kidney damage in chronic periarteritis nodosa usually leads to the development of renal failure within 1-3 years.
When the blood vessels of the organs and tissues of the abdominal cavity are affected, symptoms often appear in the early stages of the disease. Abdominal pain is typical, diffuse, persistent, and increasing in intensity. Dyspeptic symptoms are also characteristic: usually diarrhea with a stool frequency of up to 6-10 times a day mixed with blood. Anorexia, nausea, and vomiting occur.
Peritonitis often develops as a result of perforation of an ulcer or intestinal gangrene. Gastrointestinal bleeding is possible.
In 50-70%, damage to the coronary vessels of the heart occurs, although usually not accompanied by anginal pain. Myocardial infarctions develop, mostly small focal ones. Cardiosclerosis progresses rapidly, which leads to rhythm disturbances, conduction disturbances, and heart failure.
Lung damage occurs in about a third of patients with periarteritis nodosa. Manifested by bronchospasms, hypereosinophilia, eosinophilic pulmonary infiltrates.
The development of vascular pneumonia is typical, characterized by a cough with a scanty amount of sputum, occasionally hemoptysis, and increasing signs of respiratory failure.
X-ray examination shows a sharp increase in the vascular pattern, reminiscent of congestive lung, infiltration of lung tissue, mainly in the hilar zones.
Damage to the peripheral nervous system occurs in approximately half of patients. Manifested by the development of asymmetric mono- or polyneuritis. Sharp pain, paresthesia, and sometimes paresis are observed. The lower extremities are mainly affected. Sometimes a picture of polymyeloradiculoneuritis with paresis of the hands and feet develops.
In some patients (15-30%), nodular formations (which give the name of the disease) can be identified along the vascular trunks. Sometimes ulcerative-necrotic changes in the skin occur.
Sometimes damage to peripheral vessels with periarteritis nodosa can lead to soft tissue necrosis and the development of gangrene.
4.Treatment
The drug of choice is corticosteroid hormones, the withdrawal of which, however, leads to a relapse of the disease. Skin symptoms can also be relieved with hormone-containing ointments; It is often necessary to add antibiotics to the treatment regimen to suppress the associated purulent bacterial infection.
As a rule, patients require constant monitoring and therapeutic support for many years, or take treatment for life. Mild forms of the disease are considered completely curable, subject to timely diagnosis and initiation of adequate therapy.
Other options are serious diseases with a poor prognosis (with complete absence of treatment, the five-year survival rate is only about 10%). In approximately half of patients, it is possible to achieve, at best, high-quality remission.
Pathogenesis
Pathogenesis consists of a hyperallergic reaction of the body in response to etiological factors, an autoimmune antigen-antibody reaction (including to the vascular wall), and the formation of immune complexes.
Since endothelial cells have receptors for the Fc fragment of IgG and the first fraction of complement Clq, this facilitates the interaction of immune complexes with the vascular wall. Immune complexes are deposited in the vascular wall, which leads to the development of immune inflammation in it.
The formed immune complexes activate complement, which causes vascular damage, as well as the formation of chemotactic substances that attract neutrophils to the lesion. They phagocytose immune complexes, but in this case they release lysosomal proteolytic enzymes that damage the structures of the vascular wall. Neutrophils are also able to adhere to the endothelium and, in the presence of complement, release activated oxygen radicals, which aggravate vascular damage.
The endothelium also increases the release of factors that promote blood clotting and thrombus formation in the inflamed vessel.
Treatment of polyarteritis nodosa and prognosis
Recommendations for polyarteritis nodosa are based on the use of corticosteroid drugs. To relieve complications, it is recommended to prescribe cytotoxic drugs.
The prognosis is extremely difficult if adequate treatment is not prescribed. The disease develops very quickly, almost at lightning speed. Death can occur due to:
- renal failure;
- necrosis and perforation of the intestinal wall;
- critical damage to the cardiovascular system.
If treatment with corticosteroids is not prescribed, then 13% of patients survive for 5 years from the onset of the disease; if prescribed, 40% survive, but such patients experience permanent disability.
You can read more about the treatment of polyarteritis nodosa on our website https://www.dobrobut.com/.
How does periarteritis nodosa develop?
Using histological and histochemical studies, it was found that morphological changes in the vessels during periarteritis occur in a certain sequence.
First, mucous degeneration of the vascular walls occurs. Due to the separation of protein-polysaccharide complexes of connective tissue into parts, vascular permeability increases. Next, fibrous necrosis occurs, characterized by the loss of fibrin masses into the walls of the arteries. Against this background, an inflammatory reaction of cells develops, in which the walls of blood vessels are covered with lymphocytes and leukocytes. Also in the infiltrate, fibroblasts and plasma cells are detected, which very quickly become predominant, which leads to sclerosis of the arterial walls.
The disease develops immediately or sequentially in many organs. But the most often affected by periarteritis nodosa are the kidneys, blood vessels of the heart, brain, and intestines. Local changes occur in tissues and organs affected by arteritis:
- Hemorrhages are hemorrhages of varying severity.
- Violation of cellular metabolism of the parenchyma.
- Formation of ulcers and necrosis in the affected areas.
- Heart attacks with scar formation.
- Violation of vascular elasticity.
- Cirrhotic changes.
The prevalence of vascular inflammation and the severity caused by the process of secondary changes are very diverse, which speaks of the disease as polymorphic.
Non-drug therapies
When treating periarteritis nodosa, clinical recommendations are as follows:
- Therapeutic measures should be carried out under the constant supervision of medical personnel and the treating doctor. Both adults and children should be hospitalized during acute periods of pathology.
- During the period of exacerbation, the patient's motor mode is limited. Correct posture should be maintained when walking or when the patient is sitting. You need to sleep on a hard mattress and a small thin pillow.
- Eliminate mental and emotional stress.
- Daily short walks in the evening are shown. Staying in the sun should be avoided.
- Due to the immunopathological mechanism of the disease, all patients are required to follow a hypoallergenic diet. With significant progressive weight loss, a protein diet is indicated. With renal syndrome, the patient's fluid intake is controlled.
- To prevent osteoporosis, it is recommended to consume foods high in calcium and cholecalciferol (vitamin D).
- Physical therapy is carried out depending on the patient’s condition and his individual capabilities.
Surgical methods are used extremely rarely. The main methods of surgical treatment are prosthetics, bypass surgery (mostly the operation is performed on the heart, less often on the stomach), and kidney transplantation.
Polyarteritis nodosa: diagnosis
The diagnosis is made on the basis of very different patient complaints, taking into account the presence or absence of drug allergies, as well as data from additional research methods.
Is polyarteritis nodosa easily detected? Diagnosis depends on the doctor’s ability to associate manifestations of various organs and systems with this type of lesion.
The following are important in diagnosis:
- weight loss of more than 4 kg, which does not depend on nutrition;
- increase in diastolic pressure more than 90 mm Hg. Art.;
- detection of antibodies to the hepatitis B virus;
- disorders detected by arteriography;
- biopsy data - sampling of tissue from the vascular wall with subsequent examination under a microscope.