Biochemical blood test for a child
- a highly informative method of laboratory diagnostics, which allows you to diagnose (study) many diseases, pathologies, inflammatory processes and assess the functioning of the internal organs and systems of the child’s body.
A blood test for biochemistry (research, interpretation) helps the pediatrician establish or confirm a diagnosis, prescribe and adjust treatment, and determine at what stage the child’s disease is.
Standards for biochemical analysis in children
The standards for biochemical analysis in children change as they grow. After all, your baby is growing, and his organs and systems are developing and improving. That is why each age group has its own biochemical blood test norms. As a rule, diagnostic laboratories indicate reference (normal) values taking into account age in a separate column on the analysis result form. But, if your laboratory has not written the norms, or indicated the norms without taking into account the child’s age, do not be alarmed. Be sure to consult with your personal pediatrician who knows the norms of biochemical blood tests and the individual characteristics of your baby.
General urine analysis
To collect the analysis, you can use any small glass jar, which must first be boiled. Much more convenient is a special container for collecting urine: it is made of plastic, which means it will not break, and most importantly, the container has already been sterilized in advance and sealed in an impenetrable bag.
Pharmacies also now sell special urine bags; they greatly facilitate the process of collecting urine. The urine bag is a sterile polyethylene bag with an adhesive base for fixation on the child’s skin. After the baby pees, the urine is poured from the urine bag into a container.
Before collecting a urine test, the child must be washed, and here skill will be required from the parents. Usually, as soon as the child is undressed and (or) begins to wash himself, he immediately pees. Therefore, prepare everything you need to collect the analysis in advance and keep the container nearby.
The container must be delivered to the laboratory within 2–3 hours after collection. Until this time, the container must be placed in the refrigerator away from the freezer. During the hot season, when taking tests to the laboratory, you can use a cold pack.
Who can you trust to decipher a biochemical blood test?
Many parents believe that decoding the biochemical analysis of a child’s blood consists only of comparing the age-related norms with the results of the child’s analysis. And, therefore, out of ignorance, they entrust the decoding of the analysis to Internet resources or special tables. This way of deciphering a child's analysis is erroneous and very dangerous.
A pediatrician should decipher the biochemical analysis of a child’s blood. After all, only a doctor knows the child’s complaints, the peculiarities of the mother’s pregnancy and childbirth, the characteristics of the baby’s growth and development from the first day of life, and can conduct an examination and identify the child’s hereditary predisposition. The pediatrician compares all this data with the results of a biochemical analysis of the child’s blood and makes a transcript.
You can make an appointment with a doctor at the Center through:
online appointment form
or by calling the Center in Moscow:
+7,, +7 (962) 947-38-08
during the working hours of the Center (daily, seven days a week and holidays, from 9.00 to 21.00)
PRICE LIST for medical services of the Center | |
| TYPES OF MEDICAL SERVICES | Cost, rub. |
| ** The main types of analyzes are given. It is possible to conduct other types of analyzes - please check with the Center administrators for details. | |
| Potassium | 400 |
| Total calcium | 290 |
| Magnesium | 770 |
| K/Na/Cl | 400 |
| Glucose (blood sugar test) | 280 |
| Phosphorus | 300 |
| Sodium | 770 |
| Rheumatoid factor | 550 |
| C-reactive protein | 550 |
| Bilirubin and its fractions (total, direct and indirect) | 540 |
| Lactate dehydrogenase (LDH) | 280 |
| Alkaline phosphatase | 280 |
| Gamma-GT | 280 |
| Urea | 280 |
| Creatinine | 280 |
| Ionized calcium | 480 |
| Total protein | 290 |
| Total bilirubin | 290 |
| Alamine transaminase (ALT) | 280 |
| Aspartate transaminase (AST) | 280 |
| Laboratory visit within the Moscow Ring Road | 1 720 |
| Alpha-aminase | 370 |
| Emergency laboratory visit within the Moscow Ring Road | 1720 |
| Laboratory visit outside the Moscow Ring Road | 2300 |
| Cholesterol (HDL) | 340 |
| Cholesterol (LDL) | 300 |
| Total cholesterol | 300 |
Boys and girls
Due to physiological characteristics, collecting urine from boys is much easier. You can “catch” the stream of urine with a container or lower your penis into the container and wait. It is very convenient to use a urinal, which is made specifically for boys. Both the penis and testicles are placed in such a urinal.
In little girls, collecting urine is much more difficult. If there is a urinal, then you need to attach it in a circle, capturing only the labia majora. If there is no urine bag, then you will have to use a wide, but not very deep plate. Pre-wash it and pour boiling water over it. Hold the girl over (or next to) a plate and wait for her to pee.
What not to do
- There is no need to squeeze the described diaper into a container and submit such an analysis to the laboratory: the results will be unreliable, because various microorganisms and tissue fibers will get from the diaper into the contents of the container.
- There is no need to use homemade urine bags. For example, making them from a plastic bag is both inconvenient and unhygienic.
- You cannot freeze the container with the analysis (any kind). The material collected the day before is unsuitable for research.
- Enemas and laxative suppositories should not be used to stimulate bowel movements, otherwise the laboratory material will contain foreign impurities and the study will be unreliable.
When the baby grows up, the procedure for collecting tests will become much simpler. Both urine and feces can be collected from the potty. The main thing is that before collecting samples, the pot must be washed clean, but without using cleaning products. Just wash it with baby soap or baking soda and rinse thoroughly with water.
Coprogram
You will need a clean container to collect this test. You can buy it at the pharmacy, it is almost no different from a container for collecting urine, the only thing is that it has a small spoon attached to its lid. It is not necessary to wash the child immediately before collecting this analysis.
The easiest way to collect feces is from a diaper - you need to take the contents from the surface. The volume of collected material should be approximately 5–10 g (1–2 teaspoons). If the baby's stool is liquid and analysis is necessary, you will have to place the child on medical oilcloth and then carefully pour the contents into a container.
For dysbacteriosis, feces cannot be collected from a diaper.
Enterobiasis: Collection of biomaterial is carried out only in the morning, before 10.00 am. Do not wash your child either the evening before or in the morning.
Prepare a glass slide by wiping it dry. Place the child on the side, bend the legs at the knees and bring them to the stomach, spread the buttocks and collect scrapings from the perianal folds around the anus using the “print” method in several places with adhesive transparent tape (adhesive tape) 4-5 cm long. Carefully stick the adhesive tape on a glass slide sticky side down. Bring it to the laboratory in this form. The slide can be obtained from the treatment room.
Preparing a child for research
It is worth remembering about preparing your child for research
If the LHC is carried out as planned, then preparation should begin 2-3 days before the scheduled study. At this time, it is recommended to refrain from large meals, especially fatty and fried foods. Dinner on the eve of the study should be light but nutritious. It is allowed to eat cereals, porridge with milk, lean meat soups, and vegetable salad. The last meal should be 8-9 hours before the BAC. In the morning before the test, you are prohibited from eating, chewing gum, or drinking sweet liquids, but you can drink clean water.
2-3 days before the test, you should limit the child’s physical and mental stress, provide him with adequate daytime rest and night sleep. If the child is over 6 years old, on the eve of the analysis the need for the procedure should be explained to him and he should be given moral support. Blood should be taken from newborns and children under 5-6 years of age in the presence of a parent.
In emergency cases, it is possible to draw blood within the next 2-4 hours and obtain the test result within a few hours. Preparation for analysis is not required in these cases.
Blood for BAC is taken from a vein, more often from the vein of the elbow. The child’s skin at the site where it was pierced with a needle should not be inflamed, swollen or have rashes. It is prohibited to take blood for local phlebitis.
What is included in the complex
- Clinical blood test with leukocyte count and ESR (with microscopy of a blood smear to detect pathological changes) (venous blood)
- Total protein
- 25-OH vitamin D total (25-OH vitamin D2 and 25-OH vitamin D3 total result)
- Glucose (fluoride)
- Glycated hemoglobin (HbA1c)
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Gamma-GT
- Indirect bilirubin (direct bilirubin, total bilirubin)
- Total calcium
- Creatinine
- Urea
- Total cholesterol
- FSH
- Estradiol
- 17-OH-progesterone
- DGA-S
- TSH
- Testosterone
- OZhSS (Serum iron, LZhSS)
Little tricks
There are some tricks that help you collect urine quickly and without difficulty:
- if a child sleeps in a diaper at night, then in the morning you just need to unfasten the diaper, the baby will become cool and he will pee;
- turn on the water - the murmur of water will speed up urination;
- press lightly with a warm hand on the lower abdomen, give a small massage;
- If the child already knows how to stand, then in the morning, in advance, turn on the warm water to heat the bottom of the bath. As soon as your baby wakes up, take him to the bathroom, put him in the bathtub and keep a container under him. The result will not take long to arrive.
Usually, the first morning urine is needed for research, but if a special analysis is required (according to Nechiporenko), then an average portion must be collected. But in a small child it is difficult to collect urine at all, and even more so the first urine in the morning. Therefore, just any morning urine sample is suitable for analysis.
Explanation of results and reasons for deviation of normal values
Correct interpretation - correct diagnosis
| Indicator and decoding | Increase in indicator | Decrease in indicator |
| Total protein: a combination of various protein fractions, characterizes the synthetic function of the liver and the adequacy of the breakdown of protein molecules | The growth of globulins indicates:
| At:
|
| Albumin: the main blood protein, maintains plasma oncotic pressure and acid-base status, transports chemical compounds, creates a reserve of amino acids | Can be observed with dehydration, severe injuries, poisoning, burns, cholera. | At:
|
| Glucose: characterizes carbohydrate metabolism and energy reserves in the body | It may be due to a violation of the technology for taking blood (not on an empty stomach), impaired glucose tolerance, or diabetes mellitus. It occurs with pathology of the pituitary gland, adrenal glands, thyroid and pancreas. Side effects of certain medications: ACTH, corticosteroids, diuretics, thyroxine. | At:
|
| Creatinine: participates in the energy metabolism of muscle tissue and characterizes kidney function | At:
| In case of exhaustion, muscular dystrophy or atrophy. |
| Urea: the result of the exchange of nitrogenous compounds, a product of neutralized ammonia | At:
| In cases:
|
| Uric acid: product of purine base conversion reactions | At:
| At:
|
| Total cholesterol: a lipid necessary for the synthesis of cell membranes, nerve sheaths, and steroid hormones | At:
| When:
|
| HDL cholesterol: transport form of cholesterol from tissues to liver | At:
| Reduced when:
|
| LDL cholesterol: the main transport form of cholesterol | When:
| Happens when taking statins or nicotinic acid. |
| Triglycerides: neutral fats | At:
| Occurs when:
|
| Bilirubin: bile pigment, its increase is manifested by jaundice syndrome | Direct bilirubin is increased when:
Indirect bilirubin is increased when:
| Reduced with prolonged fasting. |
| AST and ALT: aminotransferases | At:
| Has no diagnostic value. |
| Alkaline phosphatase: most active in liver, bones, intestines | At:
| For: hypothyroidism, anemia, zinc deficiency. |
| GGTP: most active in the hepatobiliary system | For: diseases of the liver and pancreas, blockage of the bile ducts. | Has no diagnostic value. |
| Amylase: pancreatic enzyme | For acute and chronic pancreatitis. | |
| Creatine kinase: energy element | Different fractions increase with damage to the brain, heart muscle, and skeletal muscles. | When exhausted. |
| C-reactive protein: an indicator of inflammatory activity | For inflammatory processes of any localization. | Normally absent. |
| Rheumatoid factor: a type of autoantibody | At:
| Has no diagnostic value. |
| Calcium: forms bones, participates in the functioning of the heart, muscles, nervous system, hemostasis | In case of hyperparathyroidism. | At:
|
| Phosphorus: supports muscle and bone tissue | In case of thyroid diseases, bone tissue decay, injuries, diabetes. | For rickets and food deficiency. |
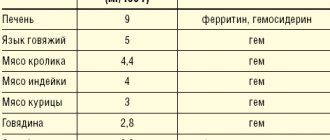
| Iron: found in hemoglobin | At:
| At:
|
| Magnesium: participates in the functioning of the nervous system, glands, muscles | In case of pathology of the thyroid gland and adrenal glands. | For chronic gastritis, enteritis, helminthic infestations, poor nutrition. |
A comprehensive laboratory examination, including basic health indicators for a child up to one year old, including blood and urine tests, as well as an assessment of protein, carbohydrate and fat metabolism.
Synonyms Russian
Laboratory examination of a child up to one year old, preventive (screening) tests up to one year old.
English synonyms
Laboratory check-up, Infancy, Infant Health Check up.
What biomaterial can be used for research?
Venous, capillary blood, an average portion of morning urine.
How to properly prepare for research?
- The child should not eat for 30-40 minutes before the test.
- Do not eat for 12 hours before the test; you can drink clean still water.
- Avoid (in consultation with your doctor) taking diuretics for 48 hours before collecting urine.
- Completely avoid (in consultation with your doctor) taking medications for 24 hours before the test.
- Avoid physical and emotional stress for 30 minutes before the test.
General information about the study
Infancy is the period of life from birth to 1 year. It is characterized by certain features both during normal development and when diseases occur during this period. Often, diseases of the infancy period manifest themselves in the form of such nonspecific signs as poor appetite, restlessness, sleep disturbances, uncontrollable crying, decreased activity, hypotonicity, and fatigue. These signs can hide quite serious diseases, such as congenital heart defects. On the other hand, these same signs can be observed from time to time in healthy infants. Thus, a clinical examination does not always allow an accurate assessment of the child’s health. In order to more accurately assess the child’s health in the period up to 1 year, additional laboratory tests are carried out - preventive (screening) tests. A comprehensive laboratory examination is especially convenient for the pediatrician and the patient, in which all the necessary tests are performed with a single collection of biomaterial (blood and urine).
This comprehensive analysis includes basic general clinical and biochemical parameters.
A complete blood count (CBC) allows you to obtain basic information about the function of the infant’s hematopoietic system, exclude congenital and acquired anemias, and suspect signs of hypoxia in congenital diseases of the cardiovascular and respiratory systems. Using the analysis of the leukocyte formula, one can suspect congenital immunodeficiencies or identify torpid infections. An additional indicator that is used to identify the current infectious and inflammatory process is the erythrocyte sedimentation rate (ESR).
Urinalysis with sediment microscopy is the best initial test for diagnosing diseases of the urinary system. It includes a macroscopic assessment of urine (color, odor, transparency), its physicochemical properties (relative density, pH, presence of protein, glucose) and microscopic examination (presence of leukocytes, epithelium, red blood cells, additional inclusions). Urinalysis can detect signs of infection and occult bleeding in both the lower and upper urinary tract. Diagnosis of congenital anomalies of the urinary system (for example, posterior urethral valve syndrome), although it requires a more thorough instrumental examination (ultrasound), also always begins with a urine test.
To assess the infant's nutritional status, total protein, glucose, and cholesterol are examined. Total protein is an integral indicator of protein metabolism in the body. Of greater importance is a decrease in total protein, which in pediatric practice can be observed with malnutrition (an extreme option is kwashiorkor), long-term infections (including helminthiasis and parasitosis), and congenital malformations of the digestive tube (congenital pyloric stenosis, duodenal atresia). Glucose is an integral indicator of carbohydrate metabolism. Hypoglycemia may indicate malnutrition, the presence of liver diseases (glycogenosis) and adrenal glands (autoimmune polyendocrine syndrome). A special condition is hypoglycemia, observed in newborn mothers with diabetes. Hyperglycemia may accompany an ongoing infectious-inflammatory process (for example, sepsis) or indicate congenital disorders of carbohydrate metabolism (for example, congenital adrenal hyperplasia). Cholesterol (cholesterol) is an integral indicator of the body's fat metabolism. Cholesterol is the main component of cell membranes and is absolutely necessary for the normal growth and development of not only infants, but also adults. Low cholesterol levels are more likely to indicate malnutrition. The cholesterol levels of breastfed and bottle-fed babies can vary greatly. Thus, by 6 months, exclusively breastfed infants have total cholesterol levels of about 200 mg/dL (roughly the same as adult cholesterol levels), while exclusively bottle-fed infants have cholesterol levels of about 140 mg/mL . Hypercholesterolemia in infancy often indicates congenital diseases of cholesterol metabolism (for example, familial hypercholesterolemia).
Bilirubin is a pigment formed by the breakdown of hemoglobin and some other heme-containing proteins in the liver, spleen and bone marrow. An increase in bilirubin levels can be observed in many diseases of the hepatobiliary system (biliary atresia, hepatitis B), hemolytic anemia, as well as in many other conditions, including hypothyroidism, sepsis, galactosemia, Crigler-Nayjar syndrome and others. To clarify the cause of hyperbilirubinemia, separate determination of direct and indirect bilirubin, as well as studies of the levels of liver enzymes, gamma-GT and alkaline phosphatase may be required.
This comprehensive analysis allows us to exclude major diseases of infancy. Additional laboratory tests may be required to obtain more complete information about the infant's health. It is recommended to perform repeated tests using the same test systems, that is, in the same laboratory.
What is the research used for?
- For a comprehensive assessment of the health status of a child up to one year old;
- for timely detection of major diseases of infancy.
When is the study scheduled?
- During a preventive examination of a child;
- if the baby has poor appetite, insufficient weight gain, hypotension, uncontrollable crying, poor sleep, and fatigue.
What do the results mean?
Reference values
Separately for each indicator included in the complex:
- [02-005] Clinical blood test (with leukocyte formula)
- [02-006] Urinalysis with microscopy
- [02-007] Erythrocyte sedimentation rate (ESR)
- [06-015] Plasma glucose
- [06-035] Total protein in serum
- [06-036] Total bilirubin
- [06-048] Total cholesterol