Ischemia
is a condition characterized by insufficient blood flow to any organ (local anemia).
Lower extremity ischemia
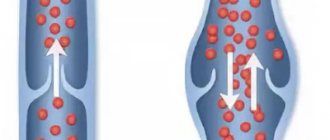
is a weakening of blood circulation in the lower extremities due to blockage (occlusion) or narrowing of the arteries. As a rule, the lowest (most distant) parts of the legs are affected. The tissues cease to receive the necessary amount of oxygen and nutrients delivered by the arterial blood flow. As a result, the leg muscles quickly tire under load, pain occurs, and tissue atrophy on the toes and feet can lead to their death (necrosis). Gangrene (tissue death) requires immediate surgical intervention - amputation of the limb, otherwise death is inevitable.
Causes of ischemia of the lower extremities
The cause of ischemia of the lower extremities may be one of the following diseases:
- atherosclerosis of the lower extremities. In this case, the lumen of the arteries is blocked by atherosclerotic deposits on the walls of the vessels;
- endarteritis (thromboangiitis) – inflammation of the artery walls, causing vessel spasm;
- thrombosis – blockage of an artery by a blood clot at the site of its formation (thrombus); or embolism - blockage (occlusion) of an artery displaced by such a clot;
- diabetic vascular damage.
Diagnosis of thrombosis or embolism
In addition to the clinical picture, it is necessary to use special research methods for diagnosis.
Ultrasound diagnostics makes it possible to clarify the nature of occlusion and identify atherosclerotic plaques during thrombosis. Thrombosis differs from embolism in the initial damage to the arteries; in embolism, the arteries are most often not affected.
Angiography is performed on the operating table to clarify the receiving vascular bed and allows you to determine the nature of the surgical intervention
Multislice computed tomography is performed when there is time for a detailed diagnosis and allows you to very accurately identify the nature of the lesions and determine treatment tactics.
Symptoms of ischemia of the lower extremities
Since ischemia of the lower extremities has such dangerous consequences, if signs of ischemia appear, you must consult a doctor. In medicine, a condition of critical ischemia is distinguished, in which urgent measures are needed to normalize blood circulation. Critical ischemia is a condition characterized by one of the following symptoms:
Leg muscle pain
Ischemia is manifested by pain in the leg muscles at rest (mainly at night).
Ischemic pain cannot be relieved with painkillers. It becomes easier if you keep your leg down (patients often lower their leg off the bed while sleeping). However, in this case, relief is achieved due to the deterioration of the outflow of venous blood, which, accumulating in the tissues, further compresses the arteries; the influx of arterial blood becomes even less, as a result of which the development of trophic phenomena (ulcers and gangrene) rapidly progresses.
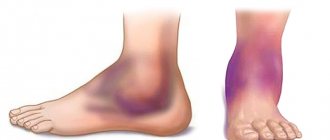
Trophic ulcers
Ulcers occur as a result of lack of nutrition. First of all, the most distant parts of the leg - the toes - are affected, then the entire foot.
Intermittent claudication
Intermittent claudication manifests itself as a forced stop when walking due to pain in the calf muscles. Similar stops may be required every 30 meters of the route.
Intermittent claudication is the main symptom of impaired blood supply to the lower extremities. If the arterial blood flow is insufficient, during physical activity (for example, walking), after some time, numbness and coldness of the leg are observed, as well as pain in the calf muscles, which prevents walking further. It is enough to just stand in one place for a while, and the pain will go away. In the early stages, pain occurs no earlier than after a kilometer of travel. But this is already a reason to consult a doctor, since the disease tends to progress, and in the future the distance that can be walked without pain will decrease.
Anesthesia
An exhausted person needs a break from suffering. Without such rest it is impossible to continue treatment. The body simply cannot withstand any active methods. Long-term epidural anesthesia relieves pain best. A thin catheter is installed in the back, into which a painkiller is injected as needed. Anesthesia allows you to lay the patient horizontally and somewhat eliminate the swelling of the limb, and conduct the necessary studies.
Narcotic analgesics (tramadol, promedol, morphine) do not have a sufficient analgesic effect, but they allow you to dull the sensations and fall asleep. The downside is the development of tolerance and drug dependence. In some surgical departments, the use of drugs and their subsequent withdrawal can persuade the patient to amputate. Non-narcotic analgesics and sleeping pills have a very weak effect on pain, do not counteract the development of depression, and contribute to the development of acute psychosis after restoration of blood flow.
Neurostimulation is an effect on the sensitive bundles of the spinal cord using a special electrical device. Good and long-term pain relief without the administration of drugs. Allows pain relief for patients who refuse surgery. The downside is that gangrene continues, and the price for the device is about $30,000.
Treatment methods for lower limb ischemia
Depending on the degree of development of ischemia and the extent of the affected areas of the arteries, various treatment methods can be used.
First of all, smoking cessation is necessary, since smoking is one of the factors that causes and aggravates diseases that contribute to the development of ischemia of the lower extremities.
In the early stages of the disease, regular exercise is an effective measure to help achieve better blood supply to the limb. A set of such exercises should be prescribed by a doctor, since improperly organized physical activity can worsen the situation. Drug therapy is also provided.
However, in most cases, critical ischemia cannot be avoided without surgical treatment.
Conservative treatment
Conservative methods (physiotherapy, drug treatment) are used to open bypass routes through which arterial blood could enter the lower limbs. Conservative treatment is also aimed at increasing blood flow, preventing thrombosis and atherosclerotic deposits.
The set of measures may also include actions aimed at increasing the level of oxygen in the blood.
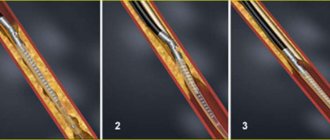
Endarterectomy
Endarterectomy is a surgical treatment method that involves removing atherosclerotic deposits from the lumen of the artery.
Stenting
Balloon angioplasty and stenting can expand the lumen of the vessel.
Femoropopliteal bypass surgery
Bypass surgery restores the flow of arterial blood into the arteries below the blocked area. Femoropopliteal bypass is used for occlusion of the femoral artery.
More information about the treatment method
Femoral-tibial bypass
If, along with the femoral artery, the popliteal artery is also affected, a femoral-tibial bypass is used.
More information about the treatment method
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
1.General information
Ischemia is one of the frequently used terms that sounds (as the main or concomitant diagnosis) in a variety of branches of medical science and everyday clinical practice. “Ischemia” literally translated from Greek means “stopping, retention of blood.” This is the name for a local, in a limited area, sharp reduction in blood supply, or its complete cessation. At the cellular level, this means the absence of oxygen bound to red blood cells, immune factors, nutrients and microelements, which normally should be supplied uninterruptedly and around the clock.
The consequences of ischemia for a tissue or organ can be very different: some structures are more sensitive and vulnerable to “blood starvation” (eg, heart, kidneys, neural tissues), others less so. Much depends on the speed and extent of development of ischemia; Thus, with a chronic lack of blood supply in the tissues, dystrophic-degenerative changes gradually increase, and at distant stages, atrophy (volume reduction and gradual death) may begin. Acute severe ischemia leads to rapid mass death of functional cells: large-scale necrosis develops (ischemic infarction), and under certain circumstances, ischemic gangrene.
Circulatory disorders in the legs are one of the most serious problems of modern medicine, since they combine several pathogenic factors inherent in a civilized person: upright posture, physical inactivity, self-destructive habits, environmental and occupational hazards, unhealthy diet. In addition, a certain role is played by the fact that the legs are the most distal (remote from the center, in this case, from the myocardium) area in the blood supply circuit, at the same time taking on themselves (together with the spinal column) the entire load when lifting weights, carrying cargo, etc.
Etiological factors and pathogenetic mechanism
The main reasons are all pathological conditions and processes that lead to impaired vascular patency:
- atherosclerotic disease;
- diabetes;
- prolonged smoking;
- inflammatory process in the wall of the vessel;
- congenital vascular anomalies;
- thrombosis and thromboembolism of arterial vessels of the legs.
HAN can provoke four groups of pathologies:
- pathological processes manifested in metabolic disorders (atherosclerotic lesions, diabetes mellitus);
- prolonged inflammation in the arteries with the presence of an autoimmune component (nonspecific aortoarteritis, thromboangitis obliterans, vasculitis);
- pathologies with a disorder of the innervation of arterial vessels (Raynaud's disease and syndrome);
- exocompression of arterial vessels.
Arterial insufficiency of the legs is mostly caused by damage to the abdominal segment of the aorta or great vessels as a result of atherosclerosis (80%). Nonspecific aortoarteritis is recorded in about 10% of patients, mainly young women.
Diabetes mellitus provokes microangiopathies in 5% of patients. Thromboangiitis obliterans accounts for less than 2%, mainly affects males 20-40 years old, and is characterized by an undulating course with exacerbations and remissions.
The main risk factors for CA are: smoking, dyslipid metabolism, high blood pressure, diabetes mellitus, excess body weight, physical inactivity, alcohol abuse, psycho-emotional factors, genetic predisposition, infections, etc.
Diagnosis
- Special examination techniques are non-invasive and invasive. The most common non-invasive method is segmental manometry with assessment of the ankle-brachial index. It allows you to measure blood pressure in different parts of the legs in comparison with that in the arms. The normal index is 1.2-1.3, in case of pathology it is less than 1.0.
- Ultrasound. Including duplex scanning. Helps in assessing arterial lumen, speed and direction of blood flow.
- Aortoarteriography is the main method of diagnosing and determining treatment tactics.
- X-ray CT with contrast, MRI or electron emission angiography.
Forecasts
In the absence of timely adequate treatment, critical ischemia will lead to the need for limb amputation.
Without timely surgery, a year after the first signs of critical ischemia appear, most patients undergo limb amputation due to the onset of gangrene. When performing endovascular treatment using angioplasty, in most patients the effect lasts for 6-24 months, and after that the patient has to undergo repeated intervention. Surgical treatment of critical ischemia using arterial bypass is more long-term and effective, despite the high risk of postoperative complications and the technical complexity of the operation. As a rule, the patency of the artery after such an intervention is maintained for 3-5 years, and the risk of recurrence of critical leg ischemia is very low.