Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
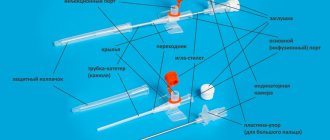
A pacemaker (pacemaker) is a small device, weighing approximately 30-50 grams, capable of creating electrical impulses that regulate heart rate. It is installed when it is necessary to maintain rhythm in patients with bradycardia or atrioventricular block, when the heart works intermittently.
A pacemaker, as a rule, consists of two parts: a metal case containing a battery designed for 7-10 years of operation and a microprocessor unit that provides heart rate setting and other parameters; the second part is the electrodes, through which electrical impulses propagate from the pacemaker into the chambers of the heart. Pacemakers are the best treatment for bradyarrhythmias. The first pacemaker was implanted in 1958.
There are three types of pacemaker (this depends on the location of the electrodes):
- Single-chamber: installed in only one chamber of the heart - the right ventricle or atrium,
- Two-chamber: installed in the atrium and ventricle of the heart,
- Three-chamber: contains a device for the treatment of heart failure, installed on the right atrium and both ventricles.
ECS is also divided into temporary (an external stimulator is installed for a period of several hours to 2 weeks) and permanent (an implanted stimulator is installed).
What is a pacemaker and how does it work?
A pacemaker (pacemaker) is a medical device designed to encourage or impose a normal rhythm on patients whose heartbeat is not fast enough or there is a blockage in signal transmission between different parts of the organ.
It is a small-sized device measuring 3 by 5 centimeters, weighing 30-45 grams, the service life without replacing batteries varies from 5 to 15 years. The operating principle of the device is based on the application of external electrical stimuli produced by the pacemaker to the heart area to ensure normal myocardial contraction. Advanced (frequency-adaptive) pacemakers additionally have sensors that can respond to changes in respiratory rate, nervous system activity, and body temperature. There are also pacemakers equipped with a defibrillator. Modern models have the function of non-invasively changing operating parameters using special devices.
A chip embedded in the device analyzes the signals generated by the heart, transmitting them directly to the myocardium and ensuring their synchronization. Conductors implanted under the endocardium transmit information from the external part of the device to the heart and data about the work of the myocardium itself back. The end of each electrode is equipped with a metal tip that collects indicators of cardiac activity and generates impulses only when necessary. When a critical decrease in heart rate or asystole develops, the pacemaker begins to work in a constant mode, producing stimuli at the frequency specified when it was implanted. If there is a sudden resumption of cardiac automaticity, the device goes into a standby state.
In emergency cases, temporary cardiac pacing is used. With external (transthoracic) pacemaker, electrodes are placed on the chest. Since the procedure is very painful, it requires deep sedation and anesthesia. Transesophageal manipulation involves the installation of a temporary device in the esophagus, and therefore has limited use.
Prohibited:
- 1. Be exposed to strong microwave fields, magnetic and electromagnetic fields, or electric current (for example, when using high voltage equipment, magnets used in industrial areas, radar or other sources of electromagnetic interference).
- 2. Perform magnetic resonance imaging (MRI) in cases where the implantable device is not MRI-compatible.
- 3. Use physiotherapy methods associated with magnetotherapy and electrical influence.
- 4. Use monopolar electrocoagulation during surgical interventions, in cases where the operation of the endocardial electrode is programmed in monopolar mode
- 5. When conducting ultrasound examinations, direct the beam directly to the body of the implanted device.
- 6. Carry out diathermy (treatment using high-frequency currents, short-wave exposure, exposure to microwave currents).
Classification of artificial pacemakers
Depending on the area of influence, there are several types of pacemakers:
- Single-chamber pacemaker. It is located and stimulates contractions in only one of the chambers of the heart (atrium or ventricle). The use of this device is very limited because it does not satisfy the physiological functioning of the muscle. It is used in the presence of a permanent form of atrial fibrillation and is installed in the right ventricle. Disadvantages: the atria continue to work in their own rhythm and when their contractions coincide with the ventricular ones, a reverse flow of blood occurs, bringing it to the heart.
- Double chamber EX. The electrodes are placed in two chambers of the heart: the generation of an impulse alternately causes contractions of the atria and ventricles, ensuring the physiological functioning of the myocardium. When using such a pacemaker, the frequency mode is individually selected, which improves the patient’s adaptation to physical activity.
- The three-chamber pacemaker is one of the newest and most expensive developments. Impulse conductors are placed in the right atrium and ventricles. Used to eliminate chamber desynchronization in severe bradycardia, heart failure of the third and fourth degrees, and rigid sinus rhythm.
International device encoding
The first letter of the code designates the chamber of the heart that is being stimulated, the second the cavity whose electrical activity is read by the pacemaker. “T” in the third position means that the device operates in trigger mode (artificial signals are synchronized with the discharges generated by the heart). The designation “D” (dual - TI) indicates that the pacemaker with two electrodes in the right side of the heart operates simultaneously in two modes. The symbol “O” characterizes the “asynchronous” rhythm of the pacemaker (the pulse frequency is set automatically during implantation).
Cardioverter-defibrillator
An implanted cardioverter-defibrillator (ICD) is a mini-copy of a device used during resuscitation in case of cardiac arrest. Because the device has direct access to the myocardium, significantly less shock force is required for effective contraction.
The ICD is intended for the prevention of sudden cardiac arrest in patients with paroxysmal arrhythmias (fibrillation and ventricular tachycardia).
The ICD system is equipped with electrodes fixed under the patient’s endocardium and the device itself, equipped with a microcircuit and a long-lasting battery, which is implanted into the subcutaneous fat on the chest.
The device performs:
- constant monitoring of cardiac activity;
- collection of contractility parameters;
- in case of life-threatening rhythm disturbances, treatment.
Forecast: service life, efficiency
The warranty period for pacemakers ranges from 3 to 5 years, depending on the manufacturer. The service life for which the device’s battery is designed is 8–10 years. After the battery is discharged or the device fails, the pacemaker will need to be replaced.
Often the electrodes passed to the heart are still in good condition. In such cases, they are not touched, but only the main part of the device is replaced - the electrical pulse generator. If the device fails before the expiration of the warranty period, a free replacement under warranty is possible, except in cases where the device broke down due to your fault.
The pacemaker is very effective in eliminating bradyarrhythmias. As for tachyarrhythmias, the device copes with attacks of supraventricular tachycardia in almost 100% of cases, and with atrial flutter, flutter or ventricular fibrillation in 80–99% of cases.
Indications and age-related contraindications: who needs the device and why?
Absolute include :
- sustained bradycardia with characteristic clinical signs;
- documented decrease in heart rate < 40 beats/min. during physical work;
- episodes of absence of rhythm (asystole) on the ECG lasting more than three seconds;
- combination of sustained AV block of II-III degree with delays in impulse conduction along two or three His bundles in patients with post-infarction cardiosclerosis;
- any types of bradyarrhythmias that may threaten the health or life of the patient (if the heart rate is less than 60 beats/min.);
- paroxysms of ventricular arrhythmias (tachycardia, fibrillation, asystole).
Relative readings:
- AV blockade of II-III degrees without changing the patient’s condition;
- loss of consciousness in patients with blockades without connection with ventricular tachycardia with an unknown cause of arrhythmia;
- severe circulatory failure with asynchronous ventricular function (with atrial fibrillation, myocardial infarction).
There are no age-related contraindications to installing a pacemaker. The only limitation is that the operation is not justified.
Installation of a pacemaker: how is the operation performed?
Before the intervention, the patient must undergo a number of instrumental studies:
- ECG with description;
- 24-hour Holter monitoring;
- EchoCG;
- general radiography of the OGK;
- bicycle ergometry, treadmill test;
- transesophageal examination of the cardiac conduction system.
Implantation of an pacemaker or cardiac defibrillator is considered a minimally invasive and low-traumatic procedure that does not require deep anesthesia and is performed under local anesthesia. If necessary, the patient may be given additional sedatives, but the patient remains conscious at all times and can talk to the medical staff. The procedure is carried out in a special operating room with an X-ray machine to constantly monitor the position of the electrodes. Duration – from 30 minutes to 1.5 hours.
Under X-ray control, a puncture of the subclavian vein is performed on the side opposite the leading arm (on the left for right-handed people and vice versa). Through a central catheter fixed to the skin, thin electrical probes are inserted into the heart cavity, which will conduct impulses from the subcutaneous part of the device to the heart. After attaching the electrodes, the cardiologist performs a series of tests to determine the threshold of myocardial sensitivity to signals in response to which an effective contraction should follow.
Throughout the procedure, the electrocardiogram is continuously recorded and interpreted.
During the operation, the doctor asks the patient to perform some tests to ensure that the electrodes are securely attached to the endocardial layer of the heart wall - take a deep breath, cough, slightly tense the abdominal muscles. After calibrating the optimal ECG indicators, the conductor is finally fixed and connected to the outdoor unit.
The pacemaker body is implanted in a pocket formed of fatty tissue or under the pectoral muscle in thin patients. After connecting all the wires, the “bed” is sutured tightly with self-absorbing sutures.
To prevent complications, a sterile bandage is applied to the vein puncture site and a prophylactic course of broad-spectrum antibiotics is prescribed.
Strict bed rest is required for the first 24 hours (there is a risk of displacement of the conductors inside the heart). The patient is under 24-hour supervision by a doctor on duty. On the second day, an X-ray inspection of the installed device is performed, the pacemaker system is adjusted (the operation of the device is optimized depending on the patient’s own rhythm), and daily electrocardiographic monitoring is carried out.
Immediately after the operation, sudden movements should be avoided: swinging the arm on the implantation side, quickly getting out of bed, bending the body, coughing. Also, do not sleep on your stomach, putting pressure on the place where the stimulator was installed.
Features of implantation in the elderly
A pacemaker can be installed in a patient of any age. The only nuance typical for older people is an increased risk of rejection due to an immune reaction to a foreign object. Due to combined pathology (the presence of atherosclerosis, type 2 diabetes mellitus), the level of complexity of installing the device increases, the procedure for implantation and healing of the postoperative scar is lengthened. The likelihood of developing purulent complications does not depend on the patient’s age. The doctor takes into account all the pros and cons of installing a pacemaker of each type for a particular patient and chooses the safest option.
How to live after the intervention?
The low-invasiveness of the procedure allows the patient to be discharged from the hospital within 3-5 days. The time spent in the hospital is necessary to set up optimal operation of the pacemaker, prevent postoperative complications, and select adequate therapy for the patient’s heart disease (dose reduction or complete withdrawal of the drug).
During the first 4-6 weeks, the patient may feel a slight tingling sensation at the site where the device was implanted. These are microdischarges that excite tissue. Often, tingling and discomfort disappear on their own; sometimes reprogramming the device is required. The rehabilitation period lasts 7-14 days. A prophylactic dose of antiarrhythmic drugs is prescribed for 7-10 days. Patients at this stage should avoid heavy emotional stress and physical labor.
After two weeks, the person returns to his previous life activities and can start working, and young women can become pregnant and give birth to a child.
There are several prohibitions in professional activities:
- working with heavy vibrating tools;
- with high-frequency heating devices;
- with electrocarbon welding devices, induction furnaces;
- with electrical appliances with a strong magnetic field or high voltage lines;
- with an electric welding machine;
- on radio and television towers.
After discharge from the hospital, you must strictly follow several rules:
- take medications prescribed by a cardiologist;
- adhere to a schedule of visits to check the operation of the pacemaker;
- Always carry with you a patient card with an implanted pacemaker.
After three, six months, and then every year, the patient must undergo a follow-up examination with a doctor and check the condition of the pacemaker using a special device that programs the operation of the device. Checking the ECS consists of:
- analysis of electrode position;
- assessing the optimality of the program;
- checking the battery charge, predicting the date of replacement of the power source;
- eliminating complications that have arisen, educating the patient.
As the pacemaker's power supply gets closer to being replaced, the frequency of visits to the doctor will increase.
There are several considerations for patients with ICD:
- driving with extreme caution;
- It is not recommended to wear a mobile phone over an implanted mechanism;
- do not linger between security gates in shops and airports;
- MRI examinations and medical procedures using certain instruments (electrocautery, diathermy, external defibrillator, ultrasound lithotripsy, radiofrequency ablation, radiation therapy) are prohibited.
Patient Prognosis
Installation of an artificial pacemaker can prolong a patient’s life for decades and significantly improve its quality.
Disability for a patient with ECS can only be established if his complete dependence on the device is proven. For this purpose, it is necessary to conduct a forensic medical and social examination (MSE), during which the patient’s health condition and the degree of circulatory failure will be assessed. Also, to prove dependence on the pacemaker, you need to temporarily turn off the device recording the electrocardiogram. If there is asystole lasting more than 5 seconds (or for 2 seconds followed by a rhythm of less than 30 beats/min), the person is considered completely dependent on the device. If the heart rate is > 40 beats/min. assignment of a disability group will be denied.
Pacemaker and long journeys
There are no travel restrictions for people with ECS. After three months, patients can easily fly on an airplane with a pacemaker. For safe travel, you must adhere to a number of rules:
- Plan a trip 3 months after pacemaker implantation.
- Be trained in the rules of behavior in the event of a device breakdown.
- Indicate to the tour operator the presence of an artificial pacemaker and arrange insurance.
- Take your ECS patient card with you (at the airport it allows you to pass a manual search instead of a magnetic frame).
- Do not stay inside the metal detector for more than 15 seconds.
- Find several nearby medical facilities that can provide assistance in an emergency.
People with an artificial pacemaker can drive without interference. The only precaution is that if you need to travel for a long time behind the wheel, it is recommended to wrap the seat belt straps with a towel to reduce the load on the site where the pacemaker is implanted.
Sex, bathhouse and other entertainment after implantation: when and to whom is it possible?
Patients with installed pacemaker have no restrictions on diet and alcohol consumption. But you should follow nutritional recommendations for cardiac pathology and drink alcohol in moderation. Two weeks after implantation of the pacemaker, if the patient feels well, the patient can return to sexual activity.
Patients with ECS can play sports with the exception of:
- contact sports (football, martial arts);
- scuba diving, scuba diving;
- sport shooting (recoil from the buttstock can damage the contacts or the body of the device).
Doctors' recommendations differ regarding relaxation in the sauna. Some categorically prohibit visiting the steam room, others are of the opinion that a short stay in the bathhouse is possible after three months from the time of the operation. In any case, it is necessary to build on the condition of the individual patient.
The following types of physical activity are not recommended:
- Lifting weights more than 5 kg.
- Contact sports such as karate, wrestling, football, etc., during which blows may be delivered to the area where the device is implanted or falls may be caused.
- Shooting from a shotgun and rifle due to the fact that recoil during a shot can damage the stimulator stock.
- When working on a personal plot, using lawn mowers, splitting, chopping wood.
- Working with rotary hammers and electric drills.
- Physical activity associated with lifting and circular movements of the arm from the side of the device implantation (swimming butterfly, crawl, backstroke).
Consequences and complications of the operation
Implantation of an artificial heart pacemaker is a surgical intervention in which there is a risk of complications:
- perforation of the myocardial wall;
- venous bleeding;
- pneumothorax;
- thrombosis of the subclavian vein.
During the recovery period, the following may develop:
- infectious inflammation of the area where the pacemaker is installed;
- endocarditis;
- conductor migration;
- pacing syndrome.
The latter develops in patients with a single-chamber pacemaker installed. The disorder is based on asynchronous contraction of the atria and ventricles, as a result of which the diastolic filling of the cavities of the heart decreases - the patient experiences increased symptoms of heart failure. Pacemaker syndrome requires additional studies (radiography, Holter rhythm monitoring) and reprogramming of the device.
In rare cases, after ICD placement, shocks may be generated when the rhythm is normal or cardioversion may not be performed when needed. The main causes of the problem are: migration of the electrode inside the cardiac cavity, an increase in the threshold of sensitivity to impulses, or complete discharge of the power supply.
Symptoms that require you to consult a doctor:
- fever, redness of the postoperative scar, pain, swelling, discharge of fluid, pus;
- uncharacteristic sensations in the area of the pacemaker;
- dyspnea;
- attacks of dizziness, loss of consciousness;
- decreased tolerance to physical activity;
- constant fatigue, drowsiness;
- chest pain;
- constant hiccups;
- increasing swelling of the legs;
- heartbeat;
- heart rate decreases below the programmed level.
Electrode dislocation
The situation represents a shift in the position of the electrode relative to the area of its installation. Most often it occurs in the first day or several weeks after surgery. The electrocardiographic picture will depend on the position of the torn conductor:
- disordered unresponsive stimuli with imposed complexes;
- failure of synchronization and stimulating function of the device;
- stimulation of the atrium or phrenic nerve.
Symptoms of dislocation of electrodes in a pacemaker manifest themselves in the form of an increase in the symptoms of heart failure and require immediate correction of the position of the conductors or their complete replacement.
Despite positive reviews of pacemakers from patients, an artificial driver or cardioverter-defibrillator is implanted to correct the heart rhythm, and this does not eliminate the root cause of the disorders.
Cost of services of an arrhythmologist
| Payment code | Nomenclature of the Ministry of Health and Social Development | Name | Price, rub.* |
| 1089 | B01.043.003 | Appointment (examination, consultation) with a doctor for X-ray endovascular treatment of cardiac arrhythmias | 4 300 |
| 1090 | B01.043.004 | Appointment (examination, consultation) with a doctor for X-ray endovascular treatment of cardiac arrhythmias with checking the operation of the pacemaker | 6 100 |
| 9004 | A05.10.006 | Electrocardiogram registration | 1 600 |
| 9006 | A05.10.008 | Holter heart rate monitoring (HM-ECG) | 4 800 |
| 15023 | A16.10.014.003 | Implantation of a two-chamber pacemaker (pacemaker), without the cost of the electrode and pacemaker | 125 000 |
Sign up for a paid appointment