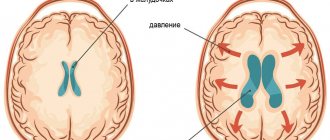
Brain edema is the body’s protective reaction to various types of injuries, hypothermia or infectious diseases. As a rule, the process of cerebral edema passes very quickly, the intercellular space and the cells themselves are filled with fluid, as a result of which the brain increases in volume, intracranial pressure increases, normal cerebral circulation is disrupted, and as a result, rapid death of brain cells begins. The outcome of the disease depends on the prompt and qualified provision of care to the patient.
Varieties, reasons
Brain edema occurs:
- vasogenic;
- cytotoxic;
- interstitial;
- osmotic.
The signs of cerebral edema depend on the type of developing pathology.
Causes of disease progression:
- Vasogenic edema occurs due to increased cerebral vascular permeability.
- Cytotoxic is the “swelling” of brain cells due to an increase in the amount of fluid inside them.
- Interstitial edema develops when there is increased pressure of the cerebrospinal fluid in the ventricles of the brain.
- Osmotic edema - with an increase in the osmolarity of brain tissue.
The most common reasons that cause brain swelling are: brain injury and disruption of its tissues in various pathologies.
Brain edema most often occurs in the following pathological conditions of a traumatic nature:
- brain contusion;
- fracture of the base of the skull;
- intracerebral hematoma;
- subdural hematoma. The prognosis of surgery for cerebral edema depends on its size.
The described pathology develops against the background of such organic brain lesions:
- ischemic and hemorrhagic stroke;
- hemorrhage under the arachnoid membrane;
- tumors;
- infectious diseases - encephalitis (inflammation of brain tissue) and meningitis (inflammation of the meninges).
Extracranial causes of cerebral edema can result from:
- Quincke's edema is a severe allergic reaction of the body;
- infectious diseases - scarlet fever, measles, mumps;
- diabetes;
- liver failure;
- alcoholism.
On our website Dobrobut.com you will find more information about the causes of cerebral edema in a newborn child, the development of pathology in the elderly and other facts.
Hydrocephalus in adults
Department of Emergency Neurosurgery > Diseases
This section is intended for people suffering from hydrocephalus, as well as for their relatives and friends. We hope that the information provided will help you better understand the disease and how to overcome it. Here we will talk about the causes of hydrocephalus in adults, methods for diagnosing it in the early stages, provide a list of necessary studies, reflect modern techniques used in our institute for the diagnosis and treatment of hydrocephalus, as well as prospects for the development of this field of neurosurgery.
Most people, including doctors, classify hydrocephalus as a childhood disease. Indeed, from 1 to 10 children out of every thousand newborns suffer from hydrocele. During a specialized examination of patients over 18 years of age in neurosurgical hospitals, hydrocephalic syndrome is detected in every fourth patient. Due to the lack of clear criteria for diagnosing hydrocephalus, only single operations for the disease in question are performed annually in non-core neurosurgical departments. Patients are discharged from such hospitals with diagnoses: “psycho-organic syndrome”, “dyscirculatory or post-traumatic encephalopathy”, “dementia of mixed origin”, “consequences of traumatic brain injury”, consequences of stroke.” This is not a complete list of diseases, under the guise of which patients are unsuccessfully treated in clinics, neurological hospitals and psychiatric hospitals. Timely and correct diagnosis of hydrocephalus and adequate surgical treatment allow patients to achieve recovery, work and social rehabilitation in almost 100% of cases. Thus, most of our patients return to their previous work, and some of the sick, despite incomplete work adaptation, can live without outside help, perform simpler activities, becoming full-fledged members of society.
A special group of patients in our department are patients with acute forms of hydrocephalus
, mainly with intraventricular hemorrhages and hemotamponade of the ventricles of the brain due to
non-traumatic subarachnoid hemorrhages
.
In cases where there is no specialized surgical care for such patients, they die within the first 12 to 48 hours from the onset of the disease. Modern methods of external drainage
with the introduction of thrombolytics into the ventricles of the brain, used in our department, can not only reduce mortality in this pathology, but also stabilize the condition of patients for a long time.
Below we present the basic concepts and terms necessary to understand the problem of hydrocephalus in adults and how to control it.
Functional anatomy of the cerebrospinal fluid-containing spaces of the brain and the definition of hydrocephalus.
Normally, each person's central nervous system contains about 120-150 ml of cerebrospinal fluid (CSF, cerebrospinal fluid). The physiological significance of CSF is as follows:
- is a kind of shock absorber for the brain, thus providing its mechanical protection during shocks and shocks
- performs nutritional functions
- maintains osmotic and oncotic balance at the tissue level
- has protective (bactericidal) properties, accumulating antibodies
- takes part in the mechanisms of regulation of blood circulation in the confined space of the cranial cavity and spinal canal.
CSF is formed in the cells of the choroid plexuses of the ventricles of the brain.
The largest amount of CSF is produced by the plexuses of the lateral ventricles of the brain (Fig. 1). The volume of CSF in the cranial cavity and in the spinal canal in an adult does not exceed 125–150 ml. About 500-600 ml of CSF is produced per day and the same amount is continuously absorbed. From the lateral ventricles of the brain, which contains about 25 ml of CSF, which enters the third ventricle through the foramen of Monroe, and from there, through the cerebral aqueduct (Aqueduct of Sylvius), the fluid enters the cavity of the fourth ventricle. The third and fourth ventricles of the brain contain approximately 5 ml of CSF. From the fourth ventricle, through the median foramen of Magendie and two lateral foramina of Luschka, located in the area of the lateral inversions of the fourth ventricle, CSF enters the subarachnoid space of the brain. At the base of the brain, the subarachnoid space expands and forms cavities filled with CSF (basal cisterns). The largest of them is located between the cerebellum and the medulla oblongata - the large cistern of the brain (cerebellar-medullary cistern). From it, CSF enters the premedullary and lateral cerebellar-medullary cisterns, located on the lower and lateral surfaces of the medulla oblongata, respectively. On the lower surface of the pons of the brain there is a rather large prepontine (prepontine) tank, which receives CSF from the above tanks. The prepontine cistern is separated from the midbrain and diencephalon cisterns (covering, interpeduncular, peduncular, chiasmatic, optic nerve) by a sheet of semipermeable membrane (Liliekvist membrane), which promotes one-way flow of CSF in the direction from back to front and from bottom to top. From the cisterns of the brain, CSF enters the convexital part of the subarachnoid space, washing the cerebral hemispheres, then is absorbed into the venous bed through the arachnoid cells and villi. The accumulation of such villi around the venous sinuses of the dura mater of the brain (there are especially many of them in the superior sagittal sinus) is called pachyon granulations. Liquid is partially absorbed into the lymphatic system, which occurs at the level of the nerve sheaths. The movement of CSF in different directions is also associated with vascular pulsation, breathing, and muscle contractions. (Fig. 1-2). If there is a violation of the relationship between the production and absorption of CSF at any of the listed levels (increased production of CSF by the choroid plexuses; closure of the ventricular openings by a tumor, adhesions, blood clots; obstruction of cells, villi and pachyonic granulations by erythrocytes, fibrosis of the membranes after hemorrhage or previous meningitis; occlusion of the sinuses) leads to a significant (maximum up to 12 liters in congenital hydrocephalus) accumulation of CSF, forming the development of hydrocephalus. The term “hydrocephalus” itself is formed by the merger of two Greek words “hydro” - water and “cephalus” - head (“dropsy of the brain”).
Below is the most complete definition of the concept of “adult hydrocephalus”.
Hydrocephalus in adults is an independent nosological form, or a complication of a number of brain diseases (tumor, hemorrhage, trauma, stroke, infectious process, etc.), characterized by an active progressive process of excessive accumulation of CSF in the cerebrospinal fluid spaces, caused by disturbances in its circulation (proximal and distal forms of occlusive hydrocephalus), absorption (aresorptive and dysresorptive forms), or production (hypersecretory form) and manifested morphologically by enlargement of the ventricles of the brain, periventricular leukareosis (decrease in the density of the medulla due to its saturation with CSF) and narrowing of the subarachnoid spaces. Clinical manifestations of hydrocephalus depend on its form.
Diseases that contribute to the formation of hydrocephalus in adults.
It has now been established that almost any pathology of the central nervous system can lead to such a complication as hydrocephalus.
Below we provide a list of only the main diseases in which hydrocephalus most often occurs:
- Brain tumors (usually stem, para-stem, or intraventricular localization).
- Inflammatory and infectious diseases of the central nervous system (meningitis, ventriculitis, encephalitis, tuberculosis, etc.).
- Subarachnoid and intraventricular hemorrhages (traumatic and non-traumatic), most often due to rupture of aneurysms and arteriovenous malformations of cerebral vessels.
- Acute cerebrovascular accidents of ischemic and hemorrhagic type.
- Encephalopathies of various origins (alcoholism, chronic hypoxic conditions, etc.).
In the department of emergency neurosurgery of the Research Institute of Emergency Medicine named after.
N.V. Sklifosovsky's priorities are the problems of diagnosis and treatment of acute and chronic hydrocephalus in non-traumatic subarachnoid hemorrhages due to rupture of arterial aneurysms of cerebral vessels or arteriovenous malformations, as well as post-traumatic hydrocephalus. Classification and pathogenesis of hydrocephalus.
- Based on its origin, hydrocephalus is divided into congenital and acquired.
Congenital hydrocephalus, as a rule, debuts in childhood. The causes of its occurrence are various intrauterine infections, hypoxia and, mainly, congenital developmental anomalies, leading either to disruption of the CSF circulation (stenosis and occlusion of the Sylvian aqueduct, Dandy-Walker anomaly, Arnold-Chiari anomaly, etc.), or accompanied by underdevelopment of structures, involved in CSF resorption (aresorptive hydrocephalus).Acquired hydrocephalus is further classified depending on the etiological factor (see causes of hydrocephalus).
- According to pathogenesis, there are three main forms of hydrocephalus.
- Occlusive (closed, non-communicating) hydrocephalus, in which the flow of cerebrospinal fluid is disrupted due to closure (occlusion) of the cerebrospinal fluid pathways by a tumor, a blood clot, or a post-inflammatory adhesive process. In the event that occlusion occurs at the level of the ventricular system (foramen of Monro, aqueduct of Sylvius, foramina of Magendie and Luschka), we are talking about proximal occlusive hydrocephalus. If the block in the path of the CSF flow is at the level of the basal cisterns, then they speak of a distal form of occlusive hydrocephalus.
- Communicating (open, dysresorptive) hydrocephalus, in which the processes of CSF resorption are disrupted due to damage to the structures involved in the absorption of CSF into the venous bed (arachnoid villi, cells, Pachionian granulations, venous sinuses).
- Hypersecretory hydrocephalus, which develops due to excess production of CSF (choroid plexus papilloma).
Previously, a fourth form of hydrocephalus was also identified, the so-called external (mixed, ex vacuo) hydrocephalus, which was characterized by an enlargement of the cerebral ventricles and subarachnoid space in conditions of progressive brain atrophy. However, this process should still be attributed to brain atrophy, and not to hydrocephalus, because the enlargement of the ventricles of the brain and the expansion of the subarachnoid space are not caused by excessive accumulation of CSF, due to disruption of the processes of its production, circulation and resorption, but by a decrease in the mass of brain tissue against the background of atrophy. - Based on current rates, they are distinguished:
- Acute hydrocephalus, when no more than 3 days pass from the first symptoms of the disease to severe decompensation.
- Subacute progressive hydrocephalus, developing within a month from the onset of the disease.
- Chronic hydrocephalus, which develops over a period of 3 weeks to 6 months or more.
- Based on the level of cerebrospinal fluid pressure, hydrocephalus is divided into the following groups:
- Hypertensive
- Normotensive
- Hypotensive
Clinical picture and diagnosis of hydrocephalus in adults.
With occlusive hydrocephalus, especially acutely developing, symptoms of increased intracranial pressure come first, which include:
- Headache;
- Nausea and/or vomiting;
- Drowsiness;
- Stagnation of the optic discs;
- Symptoms of axial dislocation of the brain.
Headache is most pronounced in the morning upon awakening, which is associated with an additional increase in intracranial pressure during sleep.
This is facilitated by vasodilation due to the accumulation of carbon dioxide, which is accompanied by blood flow, stretching of the walls of blood vessels and the dura mater of the brain at the base of the skull. Nausea and vomiting also worsen in the morning and sometimes lead to a decrease in headaches. Drowsiness is the most dangerous sign of increased intracranial pressure; its appearance precedes a period of sharp and rapid deterioration of neurological symptoms.
The development of stagnation of the optic discs is caused by an increase in pressure in the subarachnoid space surrounding the nerve and a disruption of the axoplasmic flow in it.
With the development of dislocation syndrome, there is a rapid depression of the patient's consciousness to a deep coma, oculomotor disorders appear (due to the expansion of the cerebral aqueduct), and sometimes a forced position of the head. Compression of the medulla oblongata manifests itself in rapid depression of breathing and cardiovascular activity, leading to the death of the patient.
The clinical picture is fundamentally different in the formation of chronic hydrocephalus
. The main manifestation of chronic dysresorptive hydrocephalus is a triad of symptoms:
- dementia;
- apraxia of walking or lower paraparesis;
- urinary incontinence.
The first symptoms of the disease usually appear 3 weeks after hemorrhage, trauma, meningitis or another disease leading to the development of hydrocephalus.
Disturbances in the sleep-wake cycle come first: patients become drowsy during the day with disturbances in night sleep. Subsequently, the general level of activity of the patients sharply decreases, they become spontaneous, lacking initiative, and inert. Among memory disorders, short-term memory disorders, especially numerical memory, come first. Thus, a patient with hydrocephalus cannot name the date, month, year, and incorrectly indicates his age. In the later stages of the disease, severe mnestic-intellectual impairments develop; patients can no longer care for themselves; they answer questions asked in monosyllables with long pauses, often inadequately. Apraxia of walking is that a patient with hydrocephalus can freely pretend to walk in a lying position or ride a bicycle, but as soon as he takes a vertical position, this ability is instantly lost, the patient walks with his legs wide apart, unsteadily, his gait becomes shuffling. In the later stages stages of the disease, lower paraparesis develops.
Urinary incontinence is the most late and variable symptom.
Stagnation of the optic discs is atypical for chronic hydrocephalus; as a rule, there are no changes in the fundus of the eye in such patients.
Diagnosis of hydrocephalus.
Computed tomography and magnetic resonance imaging play a leading role in the diagnosis of hydrocephalus (Fig. 1).
Rice. 1. Chronic dysresorptive hydrocephalus on CT: symmetrical expansion of the ventricular system with balloon-like enlargement of the anterior horns (one arrow), lack of visualization of subarachnoid fissures, foci of periventricular leukareosis (two arrows).
In the department of emergency neurosurgery of the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky organized round-the-clock operation of the computed tomography department. We perform a CT scan on incoming patients with subarachnoid hemorrhage in the first hours after hospitalization to assess the nature and extent of the hemorrhage, then we conduct a CT scan as a control after surgery, or when the first signs of hydrocephalus appear.
To assess the stage of hydrocephalus and determine indications for surgical intervention, our department calculates ventriculo-cranial coefficients, which show the degree of expansion of the ventricular system and its decrease after the operation.
Computed tomography also makes it possible to clarify the presence and extent of concomitant ischemic brain damage in patients with subarachnoid hemorrhages.
To predict the outcome of surgical treatment of hydrocephalus, all patients undergo a tap-test
. The essence of the test is that when at least 40 ml of cerebrospinal fluid is removed during lumbar puncture, patients with chronic hydrocephalus experience a short-term improvement. In the case of a positive test, the patient's recovery after surgery can be more likely to be predicted. However, a negative result often does not indicate the impossibility of a good outcome in the late postoperative period.
Treatment of hydrocephalus.
Conservative treatment of hydrocephalus in adults with a full-blown clinical picture is ineffective.
- Treatment of acute hydrocephalus.
- Treatment of chronic hydrocephalus.
Acute hydrocephalus, which often occurs with intraventricular hemorrhages with the development of ventricular hemotamponade, is a serious complication requiring immediate neurosurgical intervention, the purpose of which is to “unload” the ventricular system, ensure normal cerebrospinal fluid flow, and reduce intracranial pressure
and
express sanitation of cerebrospinal fluid
.
In our department, similar operations are performed, which involve the application of external ventricular drains followed by the introduction of streptokinase into the ventricular cavity - a drug that dissolves blood clots and thereby ensures normal cerebrospinal fluid flow.
In addition, the department carries out direct measurement of intracranial pressure
such patients in order to select optimal infusion therapy and adequately monitor the dynamics of the patient’s condition.
The goal of the operation is to create an artificial pathway to drain excess CSF to an area where fluid can be easily absorbed. To achieve this goal, special liquor shunt systems are used.
Shunt system design. Each CSF shunt system consists of three components:
- Ventricular catheter - intended for installation in the lateral ventricles of the brain.
- A valve is a device that allows you to regulate the outflow of CSF. The valve is designed for certain values of cerebrospinal fluid pressure and when a certain pressure is reached, the valve opens and CSF begins to flow out of the ventricular system. When the pressure normalizes, the valve closes and the flow of cerebrospinal fluid from the ventricles stops.
- Peripheral catheter - designed for installation in various cavities of the body that have the ability to absorb fluid (abdominal cavity, pelvic cavity, atrium, etc.) (Fig. 2).
a) b)
Rice. 2. Scheme of the ventriculoperitoneal shunt operation: a) cranial stage; after puncture and drainage of the anterior horn of the right lateral ventricle from Kocher's point (one arrow), the ventricular catheter is passed into the postauricular region, where it is connected to the valve of the shunt system at the level of the projection of the foramen of Monroe (two arrows); b) peritoneal stage; additional incisions in the supraclavicular region and at the level of the xiphoid process are marked with an arrow.
Every year, our department performs about 50 surgeries for hydrocephalus in adults.
We use the most advanced technologies in the installation of cerebrospinal fluid shunt systems: we use programmable valves
that allow non-invasive regulation of CSF pressure;
we install valve systems with a built-in anti-siphon device
that prevents the reverse flow of cerebrospinal fluid when the body position changes;
To implant a catheter into the abdominal cavity, endovideolaparoscopic equipment
, which allows to minimize the trauma of the operation and achieve the best results (Fig. 3).
a) b)
Rice.
3. Outcome of shunt surgery for chronic dysresorptive hydrocephalus. a) CT scan after non-traumatic subarachnoid hemorrhage. Severe internal hydrocephalus is determined (VKK2-26%). b) CT scan after implantation of a ventriculoperitoneal shunt. The normalization of the dimensions of the ventricular system is determined with the regression of foci of periventricular leukareosis and the appearance of visualization of subarachnoid fissures. Timely and correctly performed surgical intervention for hydrocephalus allows in almost 100% of cases to achieve recovery of patients, their labor and social rehabilitation.
Signs of cerebral edema
Symptoms depend on how quickly brain swelling develops.
Signs of acute cerebral edema:
- disturbance of consciousness - from slight stupor to a state of coma with cerebral edema;
- convulsions – occur as swelling progresses;
- muscle atony – develops after seizures;
- membrane symptoms.
Gradual increase in edema – additional symptoms of cerebral edema in adults:
- headache;
- nausea and vomiting that does not bring relief;
- movement disorders;
- visual and speech disorders;
- hallucinatory syndrome.
Signs indicating critical development of the condition:
- paradoxical breathing (deep breaths with long gaps between them);
- a sharp decrease in blood pressure;
- unstable pulse;
- increase in body temperature above 40 degrees Celsius.
The appearance of such signs indicates compression of the brain stem, which leads to death.
Treatment of hydrocephalus in children
Depending on the type and nature of the pathology, treatment for hydrocele can be conservative or surgical. Conservative tactics are used only in cases with a non-progressive open form of the disease, which is caused by external factors. It involves medication to relieve symptoms and eliminate the cause.
In all other situations, it is rational to use surgical treatment methods, which are aimed primarily at eliminating the obstacle that impedes the outflow of cerebrospinal fluid (tumor, abscess, intracranial hematoma, developmental anomalies). In cases where it is not possible to eliminate the cause of the pathology, a special operation is performed - bypass surgery. The technique involves introducing a system of tubes and valves into the brain, which will drain excess cerebrospinal fluid to other parts of the body.
In situations that threaten the child’s life, when immediate assistance is required, external ventricular drainage is performed - an operation during which excess cerebrospinal fluid is quickly pumped out of the ventricles of the brain using the drainage system.
With timely diagnosis and adequate treatment, a child after hydrocephalus grows and develops in accordance with the norms; the disease does not affect the mental or mental state in any way.
Diagnostics
Cerebral edema should be suspected if impairment of consciousness increases, meningeal symptoms are observed, and the patient's condition worsens.
Instrumental methods that are used to confirm the diagnosis of cerebral edema:
- computed tomography (CT);
- magnetic resonance imaging (MRI). This is an important diagnostic method - you can detect swelling of the spinal cord on MRI, and not just the brain.
Of the laboratory research methods, general and biochemical blood tests are important.
It is dangerous to perform a lumbar puncture for diagnostic purposes - displacement of brain structures and jamming of the brain stem in the occipital foramen of the skull may occur.
Disease prevention
The list of measures that can prevent the development of pathology includes:
- pregnancy planning;
- prevention of birth injuries;
- giving up bad habits before conceiving a baby and during pregnancy;
- vaccine prevention of infectious diseases of the brain (meningitis, encephalitis);
- early perinatal diagnosis;
- regular monitoring of children at risk by a pediatrician and neurologist;
- timely completion of preventive examinations up to a year;
- providing the child with safe living conditions to prevent household traumatic brain injuries.
Parents need to closely monitor the development and condition of young children, promptly contacting doctors in case of infectious diseases, falls and injuries affecting the head and neck area.
Specialists at the SM-Doctor clinic will conduct a detailed diagnosis if hydrocephalus is suspected, plan treatment and monitor the child throughout therapy and rehabilitation.
Treatment of cerebral edema
The main principles of treatment for cerebral edema are:
- dehydration;
- improvement of metabolic processes in the brain;
- etiotropic treatment;
- symptomatic therapy.
What consequences of cerebral edema during stroke and other pathologies will accompany the patient depends on the timeliness and competence of the therapy.
Dehydration therapy
Its purpose is to remove excess fluid from brain tissue. Based on the appointments:
- osmotic diuretics (diuretics);
- magnesium sulfate and glucose solution - they enhance the effect of diuretics and also improve brain nutrition;
- L-lysine escinate - the drug is not a diuretic, but removes fluid.
Improving brain processes
For this purpose the following are appointed:
- metabolic drugs;
- glucocorticosteroids;
- oxygen therapy.
Etiotropic therapy
When treating cerebral edema, it is necessary to eliminate the causes of the development of the pathology and “destroy” the mechanism of edema formation. Destination:
- antibiotics;
- removal of tumors and hematomas;
- shunt operations, after which cerebral blood supply improves
This treatment is carried out after the patient’s condition has stabilized.
Symptomatic therapy
It is aimed at eliminating cramps, vomiting, pain, and so on. In addition to conservative therapy, surgical treatment can be used:
- decompression craniotomy;
- Ventricular drainage.
Principles for preventing fatalities
The high mortality rate due to cerebral edema is caused by untimely or erroneous treatment. Elimination of pathology should occur only in the intensive care unit, otherwise death is inevitable.
The speed of diagnosis, detection of the etiological factor, as well as medical care provided directly affects the patient’s chance of survival. Complete elimination of cerebral edema occurs only after eliminating the cause of its occurrence.
The following therapeutic rules will help avoid death in this acute condition:
- relieve the patient from excess fluid thanks to administered diuretics;
- maintain acid and electrolyte balance with physiological solutions;
- constantly carry out oxygenation ;
- to equalize heart rate and stabilize blood pressure, use various medications that support the activity of the body’s “motor”;
- to improve metabolic processes in the brain, as well as reduce the level of damage to nerve tissue, use agents that block proteolysis enzymes;
- to regenerate microcirculation and use corticosteroids;
- high temperature increases the intensity of swelling, so you need to use antipyretic drugs;
- take anticonvulsant medications.
The etiological treatment process depends on the factors that led to the edema. Antibiotics are used to eliminate inflammatory diseases, glucocorticoids are used for allergic reactions, and for stroke, therapy is aimed at restoring oxygenation of the gray matter. If the pathological condition is formed due to a malignant tumor, then surgery is performed to remove it.