Phlebectomy is a surgical operation, the essence of which is to remove varicose veins of the main saphenous veins and their tributaries. Despite the rapid development of modern minimally invasive methods for treating varicose veins (endovasal laser coagulation, radiofrequency ablation, adhesive obliteration), classical phlebectomy still retains an important place in the treatment of certain groups of patients, especially in the later stages of the disease. Currently, this operation is performed with minimal tissue trauma, without large incisions and rough sutures. All veins are removed through skin punctures or micro-incisions, and the only small incision in the groin area is closed with a cosmetic absorbable suture. It is worth noting that with this type of surgical intervention, only the saphenous veins are eliminated, through which the volume of blood flowing from the lower limb is no more than 10%. Therefore, such an operation does not disrupt the normal outflow of blood through the deep veins, but, on the contrary, helps eliminate venous stagnation. Often this type of treatment is complemented by sclerotherapy to achieve the best clinical and aesthetic results.
Preoperative preparation
The operation is preceded by a face-to-face consultation with a vascular surgeon – phlebologist. After collecting an anamnesis and conducting an examination, an ultrasound duplex scanning of the veins is performed, after which indications and contraindications for treatment are determined. Preoperative preparation includes standard tests, an electrocardiogram, chest x-ray, as well as consultation with a therapist to obtain permission for surgical treatment if the patient has serious concomitant diseases.
Indications for phlebectomy
Surgical treatment of diseases of the venous system is indicated in cases where alternative methods do not bring stable results. The main indications for phlebectomy are:
- extensive varicose veins;
- increased swelling and fatigue of the legs with varicose veins;
- burning sensation in the veins;
- swelling of the venous nodes;
- pathological expansion of the saphenous veins;
- thrombophlebitis, trophic ulcers and other complications of varicose veins;
- impaired blood flow in the absence of pronounced varicose veins of the superficial veins (swelling, heaviness in the legs).
How is phlebectomy performed?
Classic phlebectomy is usually performed under spinal anesthesia in a hospital setting, where there is the ability to cope with any unforeseen situation.
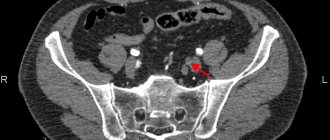
On the morning of surgery, you will need to shower and completely shave the leg that will be undergoing surgery. Then the operating surgeon, under ultrasound control, makes special markings, which makes it possible not to lose sight of pathologically altered veins, sometimes not visible during a normal external examination. This approach guarantees the usefulness of the intervention and minimal risk of relapse in the future.
The operation itself consists of several stages:
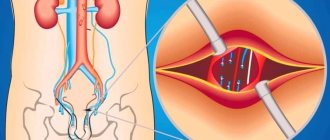
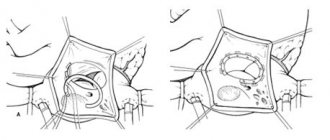
- Crossectomy - ligation and intersection of the trunk of the great or small saphenous vein and all tributaries at the point of entry into the deep venous network (in the groin or popliteal region)
- Stripping is the removal of a large or small saphenous vein affected by varicose veins by pulling the vessel using a special probe through a small incision or puncture
- Miniphlebectomy – removal of varicose tributaries and large perforating veins through micro-incisions or punctures, which, as a rule, does not require sutures and leaves virtually no marks on the skin in the future
- After the operation is completed, a special compression stocking is put on the legs or an elastic bandage is applied.
Such operations currently do not require the use of general anesthesia and after the intervention the patient is immediately sent to the ward.
Progress of classical phlebectomy
The operation can be performed under general or spinal anesthesia (when an anesthetic is injected into the spinal canal, and the patient loses sensitivity to pain below the lumbar level, but remains conscious). In any case, the patient’s body is fixed so that he does not harm himself with a sudden movement during the intervention: he is tied to the table with tapes across the torso.
Operation stages:
- A crossectomy is performed. The use of crossectomy as an independent operation is possible in emergency cases, for example, with thrombosis of the superficial veins, in order to prevent thrombosis of the deep ones.
- Stripping is performed in several ways:
- Using a Babcock probe, when a metal tourniquet is inserted into the vein through the incision left from the previous stage to the end of the vein being removed. A second incision is also made to bring the end of the probe beyond the pathological vein. At the end of the probe there is an olive with a cutting surface. The doctor slowly pulls the handle, the vein is cut off from the surrounding tissue and stretched. This is the most traumatic method.
- The vein is also pulled out with an intussusception probe, but it seems to be turned inside out. A probe is inserted into the upper incision, and through the lower incision it is fixed to the vein. Then the tissue vessel is separated under the action of a pulling movement, and the vein is gradually turned inside out, like a stocking.
- PIN stripping is similar to the previous method, but it only requires one cut left from the first stage.
- Cryostripping is performed using a special cryoprobe, which causes the end of the vein to freeze to it and it is turned out and pulled out of the leg, as with the intussusception method. An alternative to this stripping is radiofrequency and laser vein removal.
- Ligation of perforating veins. Necessary to prevent the discharge of blood from deep veins to superficial ones and as preparation for the next stage. It is performed subfascially or suprafascially (that is, the fascial sheath covering the muscles is dissected (if subfascial) or not (if suprafascial).
- Miniphlebectomy can be used at the initial stage of the disease as an independent operation, when there is a single altered vein. For this purpose, punctures are made in the areas marked before the operation, the varicose vein or node is crocheted and intersected, and then removed.
Classic phlebectomy is performed during hospitalization. If the intervention stages are replaced with minimally invasive ones - radiofrequency or laser treatment - then they are carried out on an outpatient basis under local anesthesia.
Rehabilitation period
The length of hospitalization is currently reduced to a minimum and is in most cases 2-3 days (in rare cases up to a week).
An important step in the recovery period is wearing compression garments and regular moderate physical activity. The duration and intensity of each stage is determined by the attending physician.
The rehabilitation period depends on the initial stage of varicose veins, compliance with medical recommendations, the presence of concomitant diseases and can vary from 2-3 weeks to 2-3 months.
Contraindications to phlebectomy
Phlebectomy has age restrictions and is not indicated for patients over 65 years of age, since with age such surgical intervention is difficult to tolerate due to the presence of a sufficient number of concomitant pathologies. Other contraindications include:
- pregnancy and lactation;
- deep vein thrombosis - late stage of varicose veins;
- inflammatory processes on the legs;
- coronary heart disease, severe arterial hypertension and other cardiovascular diseases;
- atherosclerosis of the lower extremities;
- severe infectious diseases;
- diabetes.
Choosing a clinic for the treatment of varicose veins and surgery
Conservative and surgical treatment of varicose veins is carried out today in many public and private medical centers. The clinic to which you entrust your health should have a serious reputation and experienced doctors. At the TN-Clinic, treatment of varicose veins is carried out by highly qualified surgeons who are proficient in various techniques of vein surgery.
In high-tech operating rooms, classical phlebectomy, mini-phlebectomy, sclerotherapy (in various variants), etc. are performed. It is important that the choice of method by the doctor is always strictly justified by the clinical picture and is discussed with the patient, the pros and cons of the methods, the risks of consequences and possible complications are explained. For example, in a clinic for the treatment of varicose veins
It is not always advisable to use minimally invasive (“easy”) techniques. Contraindications for this: severe varicose veins, thrombophlebitis, blood clotting disorders and others. In this case, a combined operation is performed to achieve a good result.
For doctors at a clinic treating varicose veins
, the results of therapy and the condition of patients are very important - both in the early and late postoperative period. That is why our surgeons are always in touch and ready to answer any questions of interest to operated patients.
Advice from a phlebologist
Despite the choice of surgical techniques for removing varicose veins and the possibility of minor outpatient interventions, any operation requires a rehabilitation period and careful attention to one’s health. Therefore, from the very first appointment until the end of medical supervision after the operation, you must follow all the recommendations of the phlebologist.
:
- first of all, wearing medical jersey; special underwear is worn immediately after surgery, after phlebectomy. The first two days, as a rule, it is recommended to wear knitwear around the clock. Next, daily wear for 3-6 weeks (according to the doctor’s indications);
- after endovasal interventions (laser therapy), which are not combined with any other methods, compression therapy is not necessary; in the case of a combined operation, wearing is required for a month or two. For the first two days, the knitwear is left overnight.
- other recommendations of the phlebologist
relate to physical activity and a healthy lifestyle, control of excess weight and changes in working conditions if it involves prolonged static load on the legs. You need to walk every day for 40-60 minutes. You can add special exercises to your daily walks to strengthen your veins and blood vessels. During the first two months after surgery, perform all physical exercises wearing compression stockings. Remove squats and weight lifting (dumbbells, barbells) from the complex. Also, do not put a lot of stress on the lower abdomen.
In general, the most important condition for successful correction of varicose veins is the cooperation of the doctor and the patient. Trusting your doctor, following all his recommendations and subsequently following the rules of prevention helps to maintain the health and beauty of your feet.
Operations phlebectomy, miniphlebectomy, at TN-Clinic
- carried out by qualified surgeons-phlebologists, Ph.D. having extensive practical experience in carrying out such operations. All manipulations are carried out under ultrasound control, in accordance with the standards and recommendations of the World Health Organization;
— the procedure takes place in absolutely sterile operating room conditions, which eliminates any possibility of complications;
— after the manipulations, the patient spends some time in a comfortable day hospital under the supervision of nurses;
— upon returning home, TN-Clinic patients are in touch with the doctor who operated on them until complete recovery
Complications
The success of surgical treatment of varicose veins depends on many factors: the age of the patient, the degree of advanced disease, concomitant diseases, etc. Depending on this, complications may arise after phlebectomy. The most common negative consequences of phlebectomy include:
- Bleeding. In the postoperative period, light bleeding from surgical wounds may occur during the first 24 hours. The reason for this is small cutaneous and subcutaneous vessels. The complication is nonspecific and is associated with errors in the surgeon’s operative technique. In some cases, bleeding may be associated with the use of anticoagulants (blood thinners). If the bleeding does not stop, revision of the wound (unraveling of sutures in the operating room) may be required.
- Hemorrhages and hematomas. The source of hemorrhage and the appearance of a hematoma after phlebectomy are small vessels that break during surgery. Hemorrhages are the soaking of blood into the skin and subcutaneous tissue (hemorrhages) or the accumulation of blood in cavities (hematoma) and are a natural complication of traumatic phlebectomy. Prevention of this complication is the use of modern low-traumatic methods of vein removal (intussusception stripping, cryostripping, miniphlebectomy), careful hemostasis both during surgery (manual compression) and after surgery (elastic bandaging and compression hosiery). Typically, hemorrhages and bruises after phlebectomy resolve on their own within 7-10 days, leaving behind slight pigmentation for up to 1-2 months.
- Infectious and inflammatory complications, such as inflammatory infiltrates (indurations) and wound suppuration. In case of development, removal of sutures and open wound management with local use of antimicrobial agents is indicated. Seals after phlebectomy are much more common (up to 15% of all phlebectomies) and represent an infectious inflammation without purulent fusion of tissue. Most often, the infiltrate forms in the area of maximum trauma and blood accumulation (hematoma infection). To treat infiltrates, antibacterial therapy and local use of anti-inflammatory and antimicrobial agents are used.
- Lymphorrhea (leakage of lymph through the surgical wound) and lymphocele (formation of a cavity filled with lymph in the surgical area) are the result of damage to lymphatic vessels and nodes due to rough handling of tissues. Lymphorrhea is treated conservatively. Lymphocele requires emptying by puncture or opening a wound. The main method of prevention is careful adherence to surgical technique and careful handling of tissues.
- Impaired skin sensitivity: decreased sensitivity on the inner surface of the leg and foot (hypoesthesia) or the appearance of unpleasant sensations such as crawling (paresthesia) is associated with damage to the nerves passing in close proximity to the trunks of the saphenous veins. This is observed when using traumatic methods of safenectomy. The method of prevention is careful handling of tissues.
- Thrombosis and embolism. Thrombosis of the deep veins of the leg, as well as the development of thrombophlebitis after phlebectomy, is extremely rare, which is associated with mandatory elastic compression after surgery and early activation of the patient.
Description of the disease
Varicose veins in the legs are a common disease in which gross changes in the walls of the veins occur and the development of functional insufficiency of the valve apparatus. As a result, a circulatory disorder occurs, which is accompanied by corresponding clinical symptoms.
Women are more likely to develop CVD than men. This is due to cyclical changes in the concentration of hormones in the body. Due to this, the elasticity of the vein walls increases and the valve apparatus loosens. Among the main causes of varicose veins of the lower extremities are:
- hereditary predisposition;
- prolonged standing or sitting;
- lack of physical activity;
- regular weight lifting;
- long-term use of estrogen-containing drugs;
- age over 30 years.
Symptoms of varicose veins in the legs are heaviness, a feeling of fullness, itching or burning. An aching, pulling, throbbing pain appears in the lower extremities. The most typical localization of pain is the calf muscles. Symptoms of varicose veins worsen after standing for a long time. A decrease in the severity of clinical signs is observed when walking, lying horizontally, and wearing compression garments. Depending on the severity of the condition, cramps may occur at night.
When examining the lower extremities, visible tortuous veins of a bluish color are determined. Many people mistakenly mistake spider veins for the initial manifestations of varicose veins of the lower extremities. This symptom is characteristic of various vascular pathologies. Therefore, when a clinical sign appears, it is recommended to consult a doctor to make a correct diagnosis.
If you do not seek medical help in a timely manner, the course of varicose veins becomes severe. As a result of prolonged circulatory disturbances, trophic changes occur in the affected area. Early signs of ulcer development are hyperpigmented areas. Next, the pathological process spreads to the subcutaneous fat. Compacted areas appear. In addition to the formation of trophic ulcers, severe swelling of the lower extremities occurs. The appearance of the above symptoms requires consulting a doctor. Specialists at the Yusupov Hospital carry out all types of diagnosis and treatment of varicose veins and its complications. For this purpose, the latest equipment and modern materials are used.
Make an appointment
Doctor's comment
You have been prescribed a combined phlebectomy, and you are experiencing quite natural anxiety about the upcoming operation? Our clinic uses the most modern methods of treatment and diagnosis, including original techniques and their modifications to avoid additional tissue trauma. In addition, thanks to a special technique and tactics of execution (invagination PIN stripping of the large and (or) small saphenous veins with special proprietary probes), making mini-incisions along the bikini line, using absorbable intradermal sutures, we manage to achieve good and excellent cosmetic results - postoperative Scars after healing after 2-3 months are almost invisible. Moreover, the combined phlebectomy techniques used in our clinic minimize hospital stay. This operation is performed under anesthesia, so any painful sensations and the patient’s “presence” at the operation are excluded. We are against a single template for treating patients with chronic venous disease. For each patient, we select a set of surgical intervention techniques based on the individual characteristics of the course of the disease, the presence and severity of concomitant pathology, physical and social activity, attitude towards one’s disease, and motivation for a good long-term result. Make an appointment and you will learn everything about the nature and prognosis of your illness. Together with you, we will draw up not only a detailed preoperative examination plan to exclude risk factors and contraindications to treatment and anesthesia, but we will also determine the optimal set of surgical intervention techniques for you, allowing you to minimize the risk of possible complications and relapse of the disease. Based on our experience, the principles of continuity in treatment and family medicine, the “open door” principle, when the patient has the right to contact the operating surgeon if necessary at any time. We will determine the frequency of further follow-up examinations for timely detection and minimally invasive outpatient elimination of disease relapse and correction of conservative treatment. Considering the chronic, multi-cause nature of varicose veins, we have moved away from the impersonal “operate and forget” system to a lifelong monitoring system, including annual ultrasound angioscanning. Together with you, we will try not only to save you from severe manifestations of the disease and its possible relapse, but also to significantly improve the quality of your life in the future.
Head of the Vascular Surgery Center Girsiashvili Aleko Givievich
Why is it better to perform combined phlebectomy at the Swiss University Hospital?
- In our Center for Vascular Surgery and Phlebology, operations are carried out using proprietary methods (in particular, invagination PIN stripping using special probes), thanks to which it was possible to reduce the trauma of surgical intervention, which leads to faster healing and a reduction in the duration of the rehabilitation period, improving the quality of life.
- We were one of the first in the country to use minimally invasive techniques as part of combined phlebectomy in the treatment of patients with chronic venous diseases; we own more than 40 patents for bloodless operations.
- Vascular surgeons (phlebologists) of our clinic have many years of experience in performing surgical interventions, each of our specialists is fluent in all the techniques used in our clinic. Each surgeon has performed more than 2,500 successful operations for varicose veins with analysis of long-term results.
- Ultrasound diagnosis of diseases of the main veins of the lower extremities and the exclusion of local contraindications before scleroobliteration, ultrasound control of the scleroobliteration procedure is carried out by vascular surgeons (phlebologists) using expert-class equipment at the highest professional level. Doctors of the Center for Vascular Surgery are certified specialists of the highest qualification category with an academic degree.
- We have developed and put into practice a protocol for ultrasound duplex scanning of the veins of the lower extremities, which allows not only to map in detail varicose veins and their sizes, but also to accurately determine the variants of pathological reflux with the location of sources of reflux, routes of spread of reflux, channels of blood return to the deep vein system. This protocol allows you to adequately select the method and scope of minimally invasive surgical intervention. Thus, in our practice, the number of tactical errors associated with the choice of method and volume of surgical intervention has significantly decreased, which has a qualitative impact on the results.
- The Vascular Surgery Center is equipped with expert-class equipment from world-famous manufacturers (such as Karl Storz, Covidien, ACUSON-Siemens, Valleylab, etc.). Cooperation with leaders in equipment production makes it possible to be several years ahead of other clinics and be one of the first to apply innovative technologies, scientific and medical developments in practice. To perform combined phlebectomy, we use, in addition to proprietary, low-traumatic surgical instruments, certified disposable surgical instruments.
- We provide treatment in accordance with international standards, the quality of the services provided is assessed by international organizations that regularly visit our clinic to verify compliance with international standards.
- For each patient, we select a set of surgical intervention techniques, based on the individual characteristics of the course and severity of varicose veins, the presence and severity of concomitant pathology, physical and social activity, attitude towards one’s disease, and motivation for a good long-term result.
- We strictly and unswervingly adhere to the principles of continuity of treatment and family medicine, the principle of “open doors”, when the patient has the right to contact the operating surgeon if necessary at any time.
- Considering the chronic nature of the course of chronic venous diseases and the tendency to relapse, we have moved away from the impersonal “operate and forget” system to a lifelong monitoring system, including annual ultrasound examination.
- We will determine the frequency of further follow-up examinations and examinations for timely detection and minimally invasive outpatient elimination of recurrent varicose veins and correction of conservative treatment.
- When determining whether a patient is suitable for combined phlebectomy, we do not follow his wishes, observing, first of all, the principle of “do no harm.”
- Together with you, we will try not only to save you from severe manifestations of chronic venous diseases and possible relapse of varicose veins, but also to significantly improve the quality of your life in the future.