Historically, the doctrine of cardialgia has its roots in ancient Greek medicine, which, despite the strongly expressed spiritual component in its concept, relied heavily on the natural causes of diseases and rational methods of treating them. In accordance with ancient Greek ideas about the nature of pain, doctors of that time began to use the terms καρδιαλγια and καρδιγμοσ to describe pain sensations that, in their opinion, emanated from the upper part of the stomach. Subsequently, these terms were borrowed by ancient Roman doctors, but depending on the context they came to mean both pain emanating from the upper stomach and pain emanating from the heart (cardialgia and cardiogmos of Galen, as well as cardiaca passia of Aretius and cardimona of Sorania), with taking into account anatomical proximity and the then prevailing ideas about the origin of pain. In the ancient Roman medical school, the term cardia meant the part of the stomach adjacent to the esophagus, and the term cordial meant pertaining to both the area of the cardia and adjacent organs, including the heart. Such terminological uncertainty persisted in modern times, when the term “cardialgia” received a rebirth in the classical work of K.F. Richter (1671) [1].
To date, the term “cardialgia” has practically disappeared from modern Western medical literature, giving way to such a concept as “chest pain” (chest pain, Thoraxschmerz, douleur thoracique). In the domestic medical literature, the term “thoracalgia” is mainly used in neurological practice, while therapists and cardiologists continue to actively use the term “cardialgia,” emphasizing the peculiarity of the localization of pain syndrome (PS). From a neurological point of view, depending on the location, local, referred and radiating pain in the chest is distinguished. Local pain can be associated with any pathological process that affects pain receptors in the skin, muscles, tendons, ligaments, joints, bones and other tissues and is felt directly in the area of tissue damage. Referred pain spreads within the dermatomes associated with the innervation of damaged structures and is usually caused by pathology of the internal organs. Referring pain associated with stretching, irritation, compression of a root or somatic nerve, is characterized by greater intensity and distal spread to the area of the corresponding dermatome, and is also usually aggravated by coughing, sneezing or physical activity. Depending on the cause, in neurological practice, vertebrogenic (pathogenetically caused by changes in the spine) and non-vertebrogenic thoracalgia are distinguished. For cardiologists and therapists, the presence or absence of ischemic origin of chest pain is more important, therefore the clinical classification of chest pain involves their division into typical angina, atypical angina and chest pain of extracardiac origin (Table 1). Thus, at present, it is advisable to use the term “cardialgia” as an equivalent to pain or discomfort in the chest not associated with acute or chronic myocardial ischemia (non-cardiac chest pain) [2–4].
. Clinical classification of chest pain [5].
It must be said that it is not possible to estimate the true number of people experiencing chest pain of the cardialgia type, since not all of them seek medical help. Based on data from population studies, the prevalence of cardialgia in the population is 13–24%. Of the number of visits to a general practitioner with complaints of pain in the chest, cardialgia accounts for 70–80%, while the frequency of cardialgia in the structure of BS in the chest area when visiting emergency departments decreases to 30%, amounting to 2– 5% of all diagnoses. According to domestic authors, almost a quarter of patients who seek medical help from a general practitioner experience chest pain of the cardialgia type. Due to the high prevalence of cardialgia, the polymorphism of its clinical manifestations, the lack of uniform reliable diagnostic algorithms and standards of medical care for this category of patients, the problem of BS in the chest is also acquiring significant economic importance for the healthcare budget [6–10].
. Characteristic localization of chest pain in various diseases.
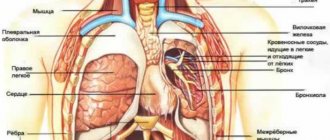
Patients complaining of chest pain represent one of the most difficult categories to diagnose. The phenomenon of pain itself, being for some period leading in the clinical picture, is at the same time in the structure of various affective and autonomic disorders, pathogenetically associated with pain in the heart. In this case, often various sensations (for example, paresthesia, a feeling of pressure, compression, etc.) are generally perceived by patients as “pain,” and the left half of the chest or sternum is designated by them as the “heart” [11, 12]. Differential diagnosis in the presence of these clinical manifestations includes a very wide range of nosological forms and first of all requires the exclusion of diseases that pose an immediate threat to the patient’s life. Thus, the approach to the differential diagnosis of BS in the chest is based, on the one hand, on the presumption of a potentially life-threatening condition, on the other, on an anatomical model that involves a consistent consideration of the likelihood of damage to anatomical formations located in the chest, from the skin to the internal organs [13].
When seeking medical help for patients with new-onset BS in the chest area, the doctor first needs to assess the following aspects [14, 15]: • clinical stability - does the patient require emergency treatment due to the presence of signs of life-threatening conditions (hemodynamic disorders, respiratory failure, etc.); • short-term prognosis – with clinical stability, identification of the risk of life-threatening conditions (acute coronary syndrome - ACS, acute aortic syndrome, pulmonary embolism, etc.); • determination of the procedure and conditions for the provision of medical care - the volume and sequence of necessary diagnostic methods, patient management on an outpatient basis, the need for hospitalization (emergency or planned).
If the patient does not need emergency medical care, the doctor has time to conduct a sufficient examination aimed at clarifying the genesis of the disease. The cornerstone of differential diagnosis remains a targeted and thorough collection of complaints and anamnesis, including detailing the characteristics of BS (Table 2).
. Assessment of pain syndrome characteristics [16].
It should be noted that, although some characteristics of BS in the chest have a certain prognostic value in relation to a positive or negative diagnosis of CAD, none of them, either individually or in combination, allows the patient to be safely released without additional examination [17, 18 ]. In addition, a number of studies have shown that nonspecific pain in the chest area of patients with risk factors for developing cardiovascular diseases has an unfavorable prognosis in terms of the development of fatal coronary complications [19].
As a rule, further examination of patients is indicated in the following cases [20–22]: • pain in the chest of a pressing, squeezing nature or a feeling of heaviness; • chest pain radiating to the neck, lower jaw, shoulders, back or arms; • dyspepsia or heartburn, nausea and/or vomiting associated with chest discomfort; • constant shortness of breath; • weakness, dizziness, episodes of loss of consciousness or fainting states.
Types of cardialgia
Psychogenic cardialgia progresses in a person against the background of depression or severe emotional shock. The patient exhibits the following symptoms:
- burning and pain in the area of the projection of the heart and in the left hypochondrium. The person notes that he either has a feeling of fullness in his chest, or, conversely, emptiness;
- the pain is constant, throbbing;
— the sensitivity of the skin in the area of the left nipple increases;
- with the psychogenic form of the disease, pain can radiate not only to the neck, spinal column or lower back, but also to the genitals.
Often the pain syndrome is accompanied by the following unpleasant sensations in certain parts of the body: tingling; crawling; numbness; tingling.
Vertebrogenic cardialgia develops when the cervical spine is affected. Pain syndrome manifests itself when the roots of the nerves that exit this part of the spine are compressed. These nerve fibers have a reflex effect on the heart and coronary blood vessels, as a result of which pressing or aching pain occurs in the area of the projection of the heart muscle.
Pleural pain
Pleural pain is a variant of nociceptive somatic pain associated with irritation of the parietal layer of the pleura. As a rule, pleural pain is acute, quite clearly localized and intensifies with deep breathing, coughing or sneezing. The causes of pleural pain include a wide range of diseases of both the pleura itself and adjacent organs (Table 3).
. The main causes of pleural pain.
If you suspect the pleural nature of the pain, you should evaluate the presence and severity of accompanying symptoms (shortness of breath, cough, hemoptysis, fever), and when directly examining the patient, pay special attention to the presence of the following signs: • increased venous pressure in the jugular veins; • paradoxical pulse; • displacement of the trachea; • pain on palpation of the chest; • change in percussion sound; • pericardial friction noise; • weakening of breathing; • crepitus or moist fine bubbling rales; • signs of deep vein thrombosis of the legs.
Mandatory laboratory and instrumental studies in the presence of pleural pain are a general blood test, an ECG (sinus tachycardia, decreased amplitude of the QRS complex, changes in the right heart, ST segment elevation or depression of the PQ interval), as well as chest x-ray in two projections ( pneumothorax, infiltrative or focal changes in the lungs, pleural effusion, rib fracture) [24, 25].
Chest pain occurs in up to 50% of patients with pulmonary embolism. The diagnosis of acute massive pulmonary embolism (PE) is usually obvious (in the absence of other diseases and risk factors). At the same time, asymptomatic episodes of pulmonary embolism often go unnoticed in a timely manner. The most typical clinical manifestations are shortness of breath, tachypnea, tachycardia, less often cough and hemoptysis, as well as clinical signs of deep vein thrombosis of the lower extremities. In 80–90% of patients with pulmonary embolism, one or more predisposing factors can be identified, the presence of which helps the clinician in establishing the correct diagnosis. Risk factors also facilitate decision-making in the event of “dubious” research results.
The main risk factors for the development of pulmonary embolism: • immobility of the patient due to various reasons: postoperative period, heart failure, contrast-enhanced tomography. Suspicion of pulmonary embolism is an indication for emergency hospitalization [26].
Pericardial pain can be clinically difficult to distinguish from pleural pain. Direct examination of the patient may reveal increased pain in the supine position and relief in the upright position, as well as a pericardial friction rub. However, information obtained from clinical examination is usually insufficient. In this case, the supporting diagnostic signs are the identified characteristic changes on the ECG (Fig. 2) and echocardiography data [27].
The basis of symptomatic therapy for BS in the chest of a pleural or pericardial nature are NSAIDs.
Symptoms of cardialgia
As the disease progresses, the following symptoms appear:
- pain syndrome localized in the left half of the chest, behind the sternum. In rare cases, pain also occurs in the armpit area. It is noteworthy that pain directly depends on the position of the person’s body. For example, it can intensify if a person bends forward or raises his left arm up;
- sleep disturbance; sense of anxiety;
- violation of the swallowing reflex;
- darkening of the eyes;
- the patient cannot take a full breath, so he has a feeling of lack of air;
- in severe cases, the development of pre-fainting or convulsions is possible;
- if the symptoms of the disease appear in a state of complete rest, then this may indicate the progression of neurocircular dystonia. In this case, the following symptoms join the main clinical picture: constant fatigue, weakness, lethargy, decreased performance.
Aortic pain
Acute aortic syndrome is a general term to describe conditions caused by acute progressive disruption of the integrity of the aortic wall. This group includes aortic dissection, intramural hematoma and penetrating atherosclerotic aortic ulcer. The appearance of the term “acute aortic syndrome” is associated with the practical need to choose treatment tactics before establishing the final etiology of aortic dissection. The classic clinical sign of aortic dissection (almost 90% of cases) is sudden, sharp pain in the chest, back or epigastric region. The peculiarity of BS is its intensity, the absence of a relieving effect of narcotic analgesics and its migrating wave-like nature (starting in most cases behind the sternum, the epicenter of pain gradually moves to the back, interscapular space and epigastric region). The migration of pain corresponds to the distribution
dissection of the aortic wall. The main diagnostic signs are asymmetry of pulse (unilateral disappearance of pulsation in the peripheral arteries is detected in 5–30% of cases) and blood pressure (when measured in the brachial arteries, the pressure difference exceeds 20 mm Hg), as well as signs of aortic regurgitation (murmur of aortic regurgitation listen in 10–30% of cases). To exclude acute myocardial ischemia, an electrocardiogram (ECG) is recorded and a chest x-ray is also performed. Suspicion of acute aortic syndrome is an indication for emergency hospitalization in a specialized medical institution. To diagnose thoracic aortic dissection and intramural hematoma, transthoracic and transesophageal echocardiography, multislice computed tomography with intravenous contrast, or magnetic resonance angiography are used. The choice of diagnostic method is determined by the ability of the medical institution to conduct this or that study in emergency cases, as well as the experience of the staff of the diagnostic department [23].
Diagnosis of cardialgia
If pain occurs in the area of the projection of the heart, it is important to immediately visit a medical facility for a full diagnosis of this condition, because such a symptom may indicate both cardialgia and the presence of pathologies of the cardiovascular system. Only a qualified specialist will be able to conduct a competent differential diagnosis and prescribe adequate treatment.
The standard diagnostic plan for cardialgia includes the following examinations: echocardiography; X-ray; EGDS of the stomach; ECG; Ultrasound; MRI of the heart; CT scan of the heart.
Newspaper "News of Medicine and Pharmacy" 11-12(331-332) 2010
1. Relevance of the topic. Diagnostics, differential diagnosis, standards of therapy
Diagnosis and differential diagnosis of cardialgia lie within such disciplines as cardiology, rheumatology, pulmonology, neurology, vertebrology, psychiatry, and endocrinology. A thorough analysis of pain makes it possible to correctly diagnose IHD in 60–70% of cases at the outpatient stage, without resorting to complex instrumental research methods. In 90% of cases, the causes of cardialgia are associated with ischemic heart disease, pathology of the pleura and lungs, pathology of the musculoskeletal system, and neuropsychiatric disorders. However, there are a large number of patients in whom the diagnosis of cardialgia is due to incorrect interpretation of pain and instrumental studies. Despite the introduction of more and more new research methods that make it possible to verify the nature of the pathology, the number of medical errors when pain in the chest occurs does not decrease. Therefore, recognition of a specific pathology, taking into account the nature of the pain syndrome, remains an urgent problem for its positive and timely solution by both young doctors and specialists with extensive medical experience.
2. Definition of pain and its brief characteristics
Pain is an extremely unpleasant aggravating experience that traumatizes the human psyche, depriving him of many qualities of normal life and activity and determining his psychophysiological state, which signals the action of factors that threaten the body and causes a certain reaction of its organs and systems. The reaction to pain in sensitive people can be so unbearable that it leads to mental disorders that may be incompatible with life.
3. Characteristics of pain arising in the region of the heart and the causes of its occurrence
Pain in the heart area is caused by impaired blood flow in cellular and tissue structures, associated with spasm of smooth muscles, inflammatory and dystrophic processes; pain occurs when peripheral nerves, afferent pathways that are part of the sympathetic and parasympathetic nervous system are irritated, and is also associated with dysfunction of opiate receptors, activation of neurohormones - enkephalins and endorphins; pain may be caused by disorders in the central nervous system.
4. What factors and processes are associated with the differentiation of pain?
Painful sensations have qualitative and quantitative characteristics, depending on their duration, distribution, emotional coloring, conditions of their appearance and intensification, accompanying manifestations, and methods of alleviating them. The therapeutic (therapeutic and relieving) and iatrogenic (increasing pain sensations or provoking their occurrence) nature of the patient’s pain depends on how the doctor approaches the assessment of pain.
5. What are the characteristics of the mental state of a patient with angina pectoris and his perception of pain?
When examining patients with mild manifestations of angina, no significant deviations in their psycho-emotional state are noted. Intense attacks of angina pectoris lead to hypochondriacal and depressive mental disorders in patients; they constantly feel anxious, show excessive impressionability, and lack confidence in their actions and decisions. Many hide their feelings, but some of them are punctual and strive to follow all the doctor’s recommendations.
6. What are the peculiarities of the psyche of patients with unstable angina and threatening myocardial infarction?
This category of patients has a feeling of subconscious fear and a feeling of approaching death.
7. What are the characteristics of pain during angina?
Features of angina pain are in its nature: pain is paroxysmal, pressing, squeezing, burning, associated with physical or emotional stress, meteorological conditions, for example, moving from a warm room to a cold one, going out into the cold in winter. Localization of pain is retrosternal with irradiation to the left half of the neck, shoulder blade, upper jaw or both extremities. Duration of pain - from 20 s to 2-3 minutes, maximum 15 minutes. Provoking factors are physical stress, emotional distress, overeating. Relief of pain attacks with nitroglycerin.
8. What is the basis for the differential diagnosis of the neurotic form of chest pain and acute coronary insufficiency (invariant angina and angina of exertion and rest)?
In table 1 presents 13 differential diagnostic symptoms and signs of three pathological conditions.
9. What is the basis for the diagnosis of neurocirculatory dystonia (NCD)?
Hereditary and constitutional data, personality traits, acute and chronic psycho-emotional stress, physical and intellectual stress, infectious diseases with a latent or recurrent course. This is a kind of cardialgia plus neurovegetative symptoms.
10. What is the peculiarity of vegetative paroxysms in NCD?
Autonomic paroxysms occur spontaneously, more often at night during sleep or morning awakening; accompanied by palpitations, pain in the heart, a feeling of lack of air, and increased blood pressure. Their duration is 2–3 hours; After the attack, a feeling of weakness remains for several days.
11. Diagnostic criteria for NCD.
Main: A. Peculiar cardialgia (pain in the precordial region, “lumbago”, nitroglycerin has a negative effect, causing headache or tachycardia; there are 5 types of cardialgia according to V.I. Makolkin, S.O. Abakumov, Moscow). B. Breathing disturbances are typical (shallow and accelerated breathing with short inhalations, a feeling of throat spasms, “dissatisfaction” with short exhalations, poor health in a stuffy room). B. Unusual lability of pulse and blood pressure. D. Rhythm disturbances in combination with changes in the T wave. D. Lability of T waves and the ST segment during functional ECG tests.
Additional:
A. Cardiac symptoms: tachycardia, bradycardia, extrasystoles, hyperkinetic state of blood circulation. B. Autonomic paroxysms, headaches, hyperalgesia. B. Psycho-emotional disorders: feeling of internal trembling, irritability, agitation, anxiety. D. Asthenic syndrome: decreased performance indicators. D. Benign course of the disease without severe neurological and mental disorders.
A reliable diagnosis is established if two main criteria and at least two additional criteria are present.
12. What are the principles of treatment for NCD?
At the first stage of treatment - psychotherapy, gymnastics, autogenic training, reflexology. For irritability - valerian root, motherwort, multivitamins with microelements, tranquilizers; for tachycardia - beta blockers, verapamil; for depression - antidepressants; metabolic drugs - asparkam, ATP-long, espo-lipon.
13. What is included in the concept of “vegetative-dishormonal myocardial dystrophy”?
Complications of premenstrual syndrome caused by chronic inflammation of the appendages, repeated abortions, pathological childbirth, psychotrauma, as well as menopausal myocardial dystrophy.
14. What are the methods for diagnosing menopausal myocardial dystrophy?
The diagnosis of climacteric myocardial dystrophy is based on the identification of cardiac, asthenic and vegetative-pathological syndromes. Cardiac syndromes manifest themselves in the form of heart pain, palpitations and difficulty breathing. All of the above occurs against the background of vegetative manifestations (hot flashes, feeling hot, headaches, polyuria). The psychological and neurological status is dominated by anxiety, hypochondria and depression. The ECG shows a negative T, diffuse nature of the pathology and positive ECG tests with potassium chloride and beta blockers to level out the negativity of the T wave.
15. What are the standards of treatment for climacteric myocardial dystrophy?
For palpitations - bellataminal, reserpine, but in the absence of depression, sex hormones - estrogens and androgens - are indicated. Metabolic therapy is widely used - asparkam, ATP-long, espalipon.
16. What are the features of pain syndrome in myocarditis?
Cardialgia is observed in half of patients with acute and recurrent inflammatory processes of the myocardium. The etiological variants of myocarditis are viral, allergic, due to chemical and physical damage, myocarditis of unknown origin. Pain with myocarditis in the precordial region is constant, stabbing, squeezing and burning without irradiation, occurring at rest and aggravated by emotional and physical stress, resistant to nitrates and relieved by non-steroidal drugs and analgesics. Cardialgia is accompanied by shortness of breath, palpitations, extrasystoles, and the appearance of 1st and 2nd degree blockades. The ECG shows tachycardia, extrasystole, blockade, ST depression, pointed or negative T wave with normalization of ECG parameters during the period of convalescence, but with the development of myocardial cardiosclerosis.
Differential diagnosis of myocardial and diffuse cardiosclerosis is presented in table. 2.
17. What are the manifestations of cardialgia in patients with mitral valve prolapse (MVP)?
The leading complaints with MVP are an unpleasant sensation in the heart area and squeezing, stabbing, aching pain of a prolonged nature, occurring suddenly with psychophysical and physical effort. Cardialgia with MVP is explained by ischemia of the papillary muscles and walls of the left ventricle due to compression by sagging mitral valves and increasing regurgitation of blood from the ventricles of the heart into the atria. The pain is accompanied by asthenoneurotic and vegetative-vascular syndrome with irritability, emotional lability, fatigue, syncope, sleep disturbances and headaches. On auscultation, a systolic murmur is usually heard by doctors in adults since childhood. On examination - asthenic constitution, poorly developed muscles, chest deformation. These observations are evidence of a genetic defect in connective tissue, including heart valves. Sudden rhythm disturbances are an objective manifestation that leads to disruption of cerebral circulation, and with significant physical stress, for example when running long distances, ends in sudden death due to ventricular fibrillation as a consequence of instability of the heart rhythm with the appearance of extrasystole “R on T” , i.e. when R seems to be “layered” on T. Systolic murmur of a late nature, i.e. at the end of systole, is heard at the apex of the heart and is accompanied by a “click”, i.e. an accentuated sound on the heart during auscultation and recorded on a phonocardiogram, which can either appear or disappear. The ECG shows flattening of the T wave or giant T wave with ST depression and extrasystoles. Treatment with beta blockers, motherwort or valerian.
18. How are cardialgia characterized by pericarditis?
Inflammation of the pericardium can be bacterial, viral, allergic, post-infarction (Dresler syndrome) or of unknown nature. Distinctive features of pain during pericarditis and cardialgia are presented in Table. 3.
19. Characteristics of functional cardiopathy in accordance with the classification of primary and secondary cardiomyopathies
Functional heart disease is a very common type of pathology, the main symptoms of which are very similar to the corresponding organic diseases. They are united by a large group of diseases, which are based on disorders of neuroregulatory systems that do not lead to the development of irreversible degenerative processes and a decrease in the basic functions of the heart and internal organs.
In table 4 shows the modern classification of primary and secondary cardiomyopathies.
Differential diagnosis of organic pathology (angina pectoris) with primary cardiopathy (psychogenic cardialgia) and secondary cardialgia (cervicothoracic osteochondrosis) is presented in table. 5.
20. What are the characteristics of pain during pleurisy?
With left-sided pleurisy, the patient complains of pain in the lower and lateral parts of the chest for several days against the background of general weakness, a dry hacking cough; the pain intensifies when breathing. On examination, there is a lag of one or another half of the chest; during auscultation - pleural friction noise of various timbres (from gentle to rough); pain decreases with the use of analgesics.
21. What is adhesive cardialgia?
These are primarily pleuropericardial adhesions, in which acute stabbing or cutting pain occurs in the region of the heart, which intensifies with sudden bending of the torso, raising the head or sharply tilting the head back. Painful attacks often occur during climate changes, especially among meteopaths.
22. What are the features of pain syndrome during pulmonary embolism (PE)?
Pain syndrome with pulmonary embolism occurs against the background of acute respiratory failure, tachycardia and decreased blood pressure. With this pathology, against the background of pulmonary infarction, fever occurs, associated with pain and aggravated by breathing and coughing. With major lesions of the main trunk of the pulmonary artery and its large branches, the pain is intense and prolonged, localized behind the sternum in its upper part with irradiation to the interscapular region, upper limbs and epigastrium. The duration of pain when lobes and segments of the lungs are affected is from 10 minutes to several hours. Reducing pain from narcotic analgesics and neuroleptoanalgesia drugs (fentanyl, droperidol) in combination with fibrinolytic agents (actilyse) and anticoagulants (heparin) improves the condition of patients. If there is no effect from the therapy, emergency removal of the thrombus-embolus from the pulmonary artery is performed in a cardiac surgery department.
23. What are the features of pain syndrome with dissecting aortic aneurysm?
Characterized by sharp and severe pain in the chest, back, and epigastric region. The pain radiates down to the lower back, to the lower extremities, which is accompanied by a sharp agitation of the patient. Soon a picture of collapse sets in. Depending on the location of aortic dissection, there are cerebral, gastrointestinal, renal and cardiovascular variants. Treatment is carried out through surgery (resection and replacement of the aorta).
24. What are the symptoms of chest pain due to lung cancer?
The first manifestations of central cancer are cough and chest pain caused by tumor growth and invasion of the bronchial wall. With left-sided cancer, pain in the heart area is observed in 20–70% of patients; this pain can be dull; as it spreads, the pain intensifies and can be relieved with non-steroidal anti-inflammatory drugs, tramadol, aminazine; with further intensification of pain, narcotic drugs are indicated: promedol, omnopon, but at some stage resistance to them develops.
Differential diagnosis of pain syndrome in diseases of the chest cavity, accompanied by various pain sensations and other manifestations, is presented in Table. 6.
25. What role does osteochondrosis of the cervical and thoracic spine play in simulating heart disease?
Cervicothoracic osteochondrosis is a degenerative process in the cartilaginous and bony parts of the spine, which causes thinning of the intervertebral discs, the formation of disc herniations and bone growth with disruption of the paravertebral structures, resulting in injury to the paravertebral ganglia, vertebral artery and sympathetic ganglia that surround the cervicothoracic section of the spine. Clinically, all this is manifested by a variety of subjective symptoms and objective signs.
The clinical picture of lesions in the upper spine consists of chest and neck pain symptoms, sympathalgia with autonomic disorders. The nature of the pain is aching, boring (projection pain), burning (sympatalgia), accompanied by “lumbago” (radicular syndrome) and lasts several weeks.
Pain in the heart region associated with coronary artery disease often coincides with exacerbations in the cervicothoracic spine. However, the positive effect on the course of coronary artery disease from the treatment of osteochondrosis should not dull the doctor’s attention regarding self-treatment of angina pectoris and the possibility of developing myocardial infarction in these patients, who may perceive an exacerbation of osteochondrosis, leading the doctor down the wrong path of their subjective feelings.
Treatment methods for osteochondrosis consist of the use of therapeutic exercises and the Shants collar, electrophoresis of potassium iodide and novocaine, phonophoresis of hydrocortisone, pulse therapy, as well as drugs aflutop, zinaxin, rumalon, etc. as background therapy.
26. What are the features of diagnosing interscapular pain syndrome (IPS)?
This MBS is a manifestation of thoracic osteochondrosis. The pain associated with arthrosis of the spinal-costal joints, felt during forced breathing, spreading along the intercostal spaces, is perceived as compression of the chest by a “hoop” and continues for hours, but goes away with a certain movement of the torso. Treatment boils down to prescribing fastum gel, non-steroidal drugs, diclofenac sodium intramuscularly.
27. Humeroscapular periarthrosis (PHP). What is its connection with pain syndrome?
PLP, or Duplay syndrome, develops gradually and is associated with limited movement of the shoulder joint. First, pain in the shoulder joint occurs during movement in it; then the pain manifests itself spontaneously, taking on an aching or burning character. The pain intensifies when dressing, putting your hands behind your back. Left-sided PLP mimics angina or the onset of myocardial infarction.
28. Shoulder-hand syndrome (Steinbrock syndrome). What is its connection with pain characterized by the properties of sympathalgia?
Steinbrock syndrome is characterized by the occurrence of swelling of the hand and is manifested by sympathalgia; duration of edema is 6–12 months. Atrophy of the hand muscles and osteoporosis in the hand and shoulder area gradually develop. The final stage is complete loss of finger function. Treatment is analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), tranquilizers.
2
9. Scapular-costal syndrome (SRS). How does it simulate left-sided pain, perceived by patients as angina? The main clinical manifestation of LRS is a feeling of heaviness and pain in the scapula area. The pain is aching, burning, radiating to the neck, shoulder girdle, and anterior chest wall; with left-sided localization, the pain is perceived by patients as cardiac. Treatment comes down to novocaine-hydrocortisone infiltration at the site of muscle attachment to the scapula, electrophoresis with novocaine and potassium iodide.
30. Vertebral artery syndrome, or posterior cervical sympathetic syndrome (PCSS), as a variant of simulating cardiac pathology
The main manifestation of SSSS is sympathalgia, manifested by pain in the heart area. Patients complain of a feeling of heat, discomfort in the left shoulder; a triad of symptoms dominates: pain in the occipital region spreading to the head, transient imbalance, tinnitus. Treatment boils down to the use of Cavinton for 2 months, cynarizine, Sermion, piracetam, NSAIDs.
31. Anterior thoracic syndrome (APCS). What is his attitude towards cardialgia?
Unlike angina, pain with SPH continues for days, weeks, or years. They are provoked by cooling the body, sudden movements; on palpation - pain in the pectoralis major muscles; Irradiation is not typical for angina. Pain decreases with the use of analgesics.
32. Tietze syndrome. What is its relationship to concomitant cardiovascular diseases, COPD and oncopathology?
Costochondral syndrome, or Tietze syndrome, is manifested by aching pain sensations radiating to the neck and shoulder; provoking factors - forced breathing, coughing, cooling. There is swelling of the costal cartilages the size of a hazelnut. Treatment boils down to pain relief with analgesics.
33. Herpes zoster (ZH) and intercostal pain syndrome (IPS). How can they manifest themselves as destabilizers of the course of angina pectoris and myocardial infarction?
Diagnostic difficulties arise in the initial stages of the disease, and to a lesser extent after the appearance of rashes, when the patient is bothered by burning pain. AL can disrupt the stable course of angina and complicate the course of myocardial infarction; For treatment, acyclovir and virazole are used for 1–2 weeks.
MBS manifests itself as spontaneous pain, which spreads when palpating the intercostal spaces and identifying their soreness. MBS is differentiated from spinal cord tumors. Determination of MBS requires a thorough examination; You should refrain from performing physiotherapeutic procedures.
Complications and consequences
Complications and consequences of cardialgia depend on the cause that caused it.
- Some diseases are characterized by a favorable course, for example, neuro-circulatory dystonia (disorder of the nervous system) or osteochondrosis (destruction of intervertebral discs with compression of nearby nerves).
- Other diseases, if not detected in a timely manner, significantly worsen the quality of life and can shorten its duration. For example: tumors of the mediastinum and lungs can cause breathing difficulties and bleeding into the chest cavity;
- myocarditis (inflammation of the heart muscle) leads to heart rhythm disturbances and heart failure;
- Gastric ulcer (formation of defects in the stomach wall) can be complicated by ulcerative bleeding or malignancy (transition to a cancerous tumor).
Esophageal pain
One of the most common causes of pain in the chest are various diseases of the esophagus, among which the most important are gastroesophageal reflux disease (GERD), diseases accompanied by impaired motility of the esophagus, and functional disorders of the esophagus, which, in accordance with the Rome criteria of the III revision, are designated as functional pain in the chest, presumably of esophageal origin. GERD accounts for more than half of all cases of esophageal pain, although the detailed mechanism of GERD-related cardialgia is unknown. In particular, it is not clear why the effect of acid on the mucous membrane of the esophagus is felt by some patients as heartburn, and by others as chest pain, especially since some patients complain of heartburn and retrosternal pain. It can be assumed that a number of patients respond to irritation of the mucous membrane of the esophagus with a reflex spasm of its smooth muscles, but convincing evidence confirming this hypothesis has not yet been presented. In some patients suffering from GERD, an esophageal-cardiac reflex is detected - a reflex spasm of the coronary arteries in response to any stressful irritation. This spasm occurs despite good vascular patency according to angiography, and leads to a decrease in coronary blood flow with the development of typical BS in the chest and the appearance of electrocardiographic changes characteristic of myocardial ischemia. In the absence of sufficient evidence to establish a diagnosis of GERD, esophageal dysmotility is often suggested as a likely pathogenetic mechanism. It is believed that pathological contractions of the esophageal wall can irritate specific mechanoreceptors, causing pain. If we consider the causes of cardialgia against the background of esophageal motility disorders not associated with GERD, the “nutcracker” esophagus is most often detected (48%), followed by a nonspecific esophageal motility disorder (36%), diffuse esophageal spasm (10%), increased tone of the lower esophagus sphincter (4%) and esophageal achalasia (2%). At the same time, the only type of disorder of the motor-tonic function of the esophagus, the role of which has been clearly proven in the occurrence of “esophageal” pain, is achalasia of the esophagus (achalasia cardia, cardiospasm). The leading pathogenetic mechanism underlying functional chest pain, presumably of esophageal origin, is the so-called. visceral hypersensitivity. It is assumed that increased sensitivity of the peripheral sensory endings of afferent nerve fibers may cause hyperreactivity of the esophageal mucosa in response to various physiological or pathological stimuli. In addition, disturbances of central origin may occur in the process of processing sensory information entering the brain from the esophagus, with localization of enhanced perception of afferent stimuli at the level of the brain or dorsal horns of the spinal cord.
In typical cases, esophageal cardialgia is described as chest pain, sometimes radiating to the mid-back, lower jaw and left arm, which may be clinically indistinguishable from angina. In this regard, the first stage of the diagnostic search is aimed at excluding coronary heart disease as a cause of BS in the chest. The presence of accompanying symptoms, such as heartburn, rumination and regurgitation, should not mislead the doctor, because due to the high prevalence in the population of both ischemic heart disease and
diseases of the esophagus, there is a high probability of their combination. Only after careful exclusion of cardiovascular pathology with the obligatory participation of a cardiologist should one think about possible pathology of the esophagus (including GERD, motor dysfunction and visceral hypersensitivity). Esophagogastroduodenoscopy is the gold standard for detecting erosive esophagitis and complications of GERD such as stricture, ulceration, or Barrett's esophagus. If “alarm symptoms” are detected (weight loss, dysphagia, odynophagia, anorexia, bleeding from the upper digestive tract, anemia), the examination of a patient suffering from “esophageal” pain should begin with an endoscopic examination. It should be noted that in 30–60% of patients with severe symptoms, endoscopic examination does not reveal visible changes in the mucous membrane, so X-ray examination of the esophagus has not lost its practical significance. Over the past few years, approaches to diagnosing esophageal disorders have undergone certain changes. This is due to the beginning of the widespread use of diagnostic tests with proton pump inhibitors (PPIs) and the identification of low sensitivity of a number of previously quite popular studies.
In accordance with the principle of general medical practice “treatment precedes diagnosis,” in patients without warning symptoms for ex juvantibus diagnosis, a course of PPI therapy in double dosages is recommended (usually omeprazole at a daily dosage of 60–80 mg, rabeprazole at 40 mg/day, or lansoprazole at 60 mg/day). –90 mg/day). The duration of the trial treatment course depends on the frequency of chest pain in the patient and can range from 1 to 28 days. In particular, when recording episodes of non-cardiac chest pain 1-2 times a week, the duration of the diagnostic test with PPI should be at least 2 weeks. If there is no effect, referral to a specialized gastroenterology department is recommended for additional examination (esophageal pH-metry and manometry). When spastic type motor dysfunction is established (nutcracker esophagus, diffuse esophagospasm), theophylline is recommended; in case of functional disorders, pain modulators (tricyclic antidepressants, serotonin reuptake inhibitors) are recommended [28–30].
Causes
Cardiac syndrome develops not only due to heart disease, but also for other reasons not related to the functioning of the cardiovascular system. Chest pain can be caused by pathological changes in the internal organs, spine, and respiratory system.
Related to the heart
Severe pain syndrome may be associated with the following heart diseases:
- Angina pectoris . The disease is associated with a violation of the supply of oxygen and nutrients to the myocardium.
- Myocarditis is an inflammatory process in the heart muscle.
- Myocardial infarction . Progressive ischemia provokes necrosis of the heart muscle.
- Cardiomyopathy is an increase in the size of the heart cavities and a decrease in its pumping function.
- Heart valve defects.
- Pericarditis.
- Hypertrophy of the right or left ventricle.
Other factors
Cardiac syndrome can be caused not only by heart disease. In this case, the pain radiates from another source and imitates cardialgia. Pathologies that provoke extracardiac cardialgia:
- Diseases of the musculoskeletal system: scoliosis , osteochondrosis , Falconer-Weddell syndrome , intervertebral hernia .
- Nervous system disorders ( heart neurosis , manifested by a complex of disorders).
- Dysfunctional disorders in the digestive tract: diaphragmatic hernia , ulcerative lesions of the intestines and stomach, esophagitis .
- Disturbances in the functioning of the endocrine system.
- Diseases of the respiratory system: pneumonia , bronchitis , pulmonary hypertension , pleurisy .
Pain syndrome can be caused by traumatic injury to the spine, pulmonary system, or abdomen.
Women during menopause, as well as during pregnancy, may experience chest pain of an idiopathic nature. In children and adolescents, pain may be associated with hormonal changes and a period of active growth. Such conditions do not require specific treatment and go away on their own.
Treatment of cardialgia with folk remedies
Traditional medicine can help alleviate conditions and reduce the severity of pain, but the use of herbal remedies does not exclude a full examination and identification of the true cause of pain.
- Add figs, lemon, walnuts and honey to 50 ml of vodka. Infuse the mixture for 4 days. You need to take the tincture twice a day, 1 teaspoon.
- Boil hawthorn fruits in water. The resulting infusion should be taken three times a day, 30 drops.
- Add lemon peel, figs, honey and persimmon to vodka. Leave the mixture in a cool, dark place for a week. You need to take the solution three times a day, 1 tablespoon.
- Add dried rosemary to vodka. The resulting mixture should be taken 30 minutes before meals three times a day, 35 drops.
- Mix hawthorn fruits, marsh cudweed, motherwort, sage and oregano. The herbal mixture should be infused in a water bath for 10 minutes. Take the resulting infusion once a day, half a glass. The duration of treatment is 21 days.