I degree - sensitivity and movement in the limb are preserved:
- IA – coldness, paresthesia, numbness of the limb
- IB - pain in the distal parts of the limb at rest.
II degree – disorders of movement and sensitivity of the limb occur:
- IIA – limb paresis (decreased muscle strength and range of active movements in the distal parts)
- IIB - limb paralysis (lack of active movements)
III degree – necrobiotic phenomena develop:
- IIIA – subfascial edema
- IIIB – partial muscle contracture
- IIIB – total muscle contracture
The degree of limb ischemia is taken into account when choosing a treatment method for acute vascular occlusion.
Symptoms of vascular occlusion
Acute occlusion of the vessels of the extremities is manifested by a symptom complex, designated in the English literature as the “complex of five Ps” (pain - pain, pulselessness - lack of pulse, pallor - pallor, paresthesia - paresthesia, paralysis - paralysis). The presence of at least one of these signs makes one think about possible acute occlusion of the vessels of the extremities.
Sudden pain distal to the site of occlusion occurs in 75-80% of cases and is usually the first sign of acute occlusion of the vessels of the extremities. If collateral circulation is preserved, pain may be minimal or absent. More often, the pain is diffuse in nature with a tendency to intensify, and does not subside when the position of the limb changes; In rare cases of spontaneous resolution of occlusion, the pain disappears on its own.
An important diagnostic sign of acute occlusion of the vessels of the extremities is the absence of pulsation of the arteries distal to the site of occlusion. In this case, the limb first turns pale, then acquires a cyanotic tint with a marbled pattern. Skin temperature is sharply reduced - the limb is cold to the touch. Sometimes, upon examination, signs of chronic ischemia are revealed - wrinkled and dry skin, lack of hair, brittle nails.
Disorders of sensitivity and motor sphere in acute occlusion of the vessels of the extremities are manifested by numbness, tingling and crawling sensations, decreased tactile sensitivity (paresthesia), decreased muscle strength (paresis) or lack of active movements (paralysis) first in the distal and then in the proximal joints . In the future, complete immobility of the affected limb may occur, which indicates deep ischemia and is a formidable prognostic sign. The end result of acute vascular occlusion can be gangrene of the limb.
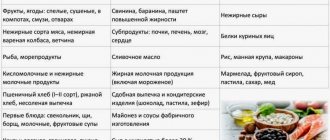
Diet for occlusion
To restore the elasticity of the vascular wall, strengthen it and reduce the severity of occlusion, it is recommended to adhere to certain dietary rules. In case of occlusion, it is recommended to adhere to a special cholesterol-lowering diet, which includes:
- Legumes . Beans and legumes are sources of protein, iron, folic acid and contain absolutely no fatty acids.
- Whole grains (wheat bread, buckwheat, oatmeal and brown rice).
- Cabbage (all types, especially broccoli). Prevents salt deposition, normalizes the lipid spectrum of cholesterol, enriches the body with vitamins K and C.
- Asparagus . Helps lower blood pressure and reduce cholesterol in the blood.
- Persimmon . Rich in fiber and has a pronounced antioxidant effect.
- Spinach . Allows you to reduce blood pressure in hypertensive patients.
- Turmeric . It has an anti-atherosclerotic effect, reduces the volume of cholesterol plaques, and reduces the severity of the inflammatory process.
Diagnosis of acute vascular occlusion of the extremities
The diagnostic algorithm for suspected acute occlusion of the vessels of the extremities involves conducting a complex of physical, laboratory, and instrumental studies. Palpation of the pulse at typical points (on the dorsal artery of the foot, in the popliteal fossa, on the posterotibial and femoral arteries, etc.) reveals the absence of pulsation of the artery below the occlusion and its preservation above the affected area. Important information during the initial examination is provided by functional tests: marching (Delbe-Perthes test), knee phenomenon (Panchenko test), determination of the zone of reactive hyperemia (Moshkovich test).
Laboratory blood tests (coagulogram) in acute occlusion of the vessels of the extremities reveal an increase in PTI, a decrease in bleeding time, and an increase in fibrinogen. The final diagnosis of acute occlusion of the vessels of the extremities and the choice of treatment tactics are determined by ultrasound data (duplex scanning) of the arteries of the upper or lower extremities, peripheral arteriography, CT arteriography, MR angiography.
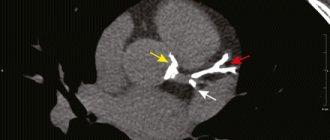
CT angiography of the abdominal aorta and its branches. Complete occlusion of the lumen of the left internal iliac artery
Differential diagnosis is carried out with a dissecting aneurysm of the abdominal aorta and acute thrombophlebitis of the deep veins.
Chronic occlusions of the coronary arteries
Chronic occlusions make up a significant portion of coronary artery lesions detected in patients during diagnostic coronary angiography. In the case of multivessel disease, the patient may be offered either coronary artery bypass surgery or an endovascular coronary artery stenting procedure.
If multi-vessel lesions of the coronary arteries are detected, it is possible to perform a one-stage endovascular procedure for myocardial revascularization on several coronary vessels or to perform a staged endovascular procedure. Recanalization of chronic occlusions, in turn, requires special training of the radiosurgeon and sufficient experience in performing such operations.
An example of successful treatment of a patient with multivessel disease and chronic coronary occlusions
Patient A., 44 years old, was admitted to the Clinic of Innovative Surgery in September 2015. For a long time, the young man was bothered by chest pain and shortness of breath with little physical activity, and a sharp impairment in his ability to work. After a detailed examination, a diagnosis was made - coronary heart disease, functional class 3. Coronary angiography was recommended and performed.
Coronary angiography revealed multi-vessel multi-level occlusive-stenotic lesion of the coronary bed:
- LKA barrel: normally positioned, not changed,
- RCA: in the proximal segment there is extensive chronic occlusion, the post-occlusion section is satisfactorily filled through intra- and intersystem collaterals.
- 1DV: large branch, in the proximal third from the mouth there is stenosis up to 80%.
- Intermediary artery: large branch, 80% stenosis in the proximal third.
- OA: in the middle segment there is chronic occlusion, the post-occlusion section is satisfactorily filled through intra- and intersystem collaterals.
- RCA: the previously installed stent in the middle segment is passable, without signs of restenosis.
Taking into account the data from the clinical picture, laboratory and instrumental research methods, and coronary angiography, a collective decision was made on the need for surgery to restore the patency of the arteries. Considering all the risks and possible complications, the patient categorically refused coronary bypass surgery and insisted on having coronary stenting. The department's doctors were ready to help him.
Operation stages
After careful medical preparation, the patient underwent recanalization and stenting of the circumflex branch of the left coronary artery, as well as recanalization of the anterior descending branch of the left coronary artery, followed by bifurcation stenting of the LAD and diagonal branch of the LMCA. The complex operation lasted several hours. However. For the patient, it was painless - the intervention was performed under local anesthesia with novocaine at the puncture area in the femoral artery. During the procedure, the anesthesiologist and surgeons were able to communicate with the patient, he was conscious.
The result of the long and painstaking work of the clinic’s team of doctors was the complete restoration of the patency of all arteries of the heart and, as a result, a significant improvement in the patient’s quality of life.
Treatment of acute vascular occlusion of the extremities
If acute occlusion of the vessels of the extremities is suspected, the patient requires emergency hospitalization and consultation with a vascular surgeon. For tension ischemia and degree IA ischemia, intensive conservative therapy is carried out, including the administration of thrombolytics (intravenous heparin), fibrinolytic agents (fibrinolysin, streptokinase, streptodecase, tissue plasminogen activator), antiplatelet agents, and antispasmodics. Physiotherapeutic procedures (diadynamic therapy, magnetic therapy, barotherapy) and extracorporeal hemocorrection (plasmapheresis) are indicated.
In the absence of positive dynamics within 24 hours from the onset of acute occlusion of the vessels of the extremities, it is necessary to perform an organ-preserving surgical operation - thromboembolectomy from a peripheral artery using a Fogarty balloon catheter or endarterectomy.
In case of ischemia of degrees IB–IIB, emergency intervention is necessary to restore blood flow: embolism or thrombectomy, bypass surgery. Prosthetic replacement of a segment of a peripheral artery is performed for short-term acute occlusions of the vessels of the extremities.
Ischemia of degrees IIIA–IIIB is an indication for emergency thrombus or embolectomy, bypass surgery, which must be supplemented with fasciotomy. Restoring blood circulation with limited contractures allows for delayed necrectomy or subsequent amputation at a lower level.
In case of ischemia and IIIB degree, vascular surgery is contraindicated, since restoration of blood flow can lead to the development of post-ischemic syndrome (similar to traumatic toxemia in the long-term crush syndrome) and the death of the patient. At this stage, amputation of the affected limb is performed. In the postoperative period, anticoagulant therapy is continued to prevent rethrombosis and re-embolism.
Causes
Most often, occlusion develops as a result of embolism, blockage of a blood vessel by a dense formation. This process can develop as a result of:
- Infectious disease . In this case, the blood flow is blocked by inflammatory-purulent blood clots or the accumulation of a large number of pathogenic microorganisms.
- Air embolism . It develops as a result of an air bubble entering the systemic bloodstream. It is determined after traumatic damage to a vessel or after an incorrectly performed injection.
- Fat embolism . As a result of metabolic , fat particles accumulate and a fat clot forms from them.
- Arterial embolism . Thrombi form on the valve apparatus of the heart and are characterized by instability and mobility, which can lead to separation of thrombotic masses and blockage.
Occlusion of the vessels of the neck and coronary arteries is formed in the area of their branching or narrowing.
Causes of thrombosis:
- malignant neoplasms;
- atherosclerosis;
- traumatic injuries;
- aneurysms;
- thromboembolism.
As a result of traumatic damage to muscle tissue and the skeletal system, compression occurs and blood flow is blocked.
Prognosis and prevention
The most important prognostic criterion for acute occlusion of the vessels of the extremities is the time factor. Early surgery and intensive therapy can restore blood flow in 90% of cases. If treatment is started late or is absent, disability occurs due to the loss of a limb or death. With the development of reperfusion syndrome, death can occur from sepsis, renal failure, or multiple organ failure.
Prevention of acute vascular occlusion of the extremities involves timely elimination of potential sources of thromboembolism and prophylactic administration of antiplatelet agents.
General information
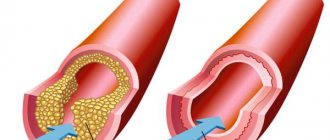
Vascular occlusion is a blockage (more often of arteries than veins), which is characterized by a pronounced decrease in the speed and quality of blood flow. Occlusion can cause necrosis and, as a result, lead to death.
The pathology is quite common and can affect the organs of visual perception, the central nervous system, limbs and great vessels. sepsis and peritonitis develop . Abdominal ischemic syndrome develops against the background of a lack of adequate blood circulation in the digestive tract. The pathology is associated with occlusion of the unpaired visceral branches of the abdominal aorta - the celiac trunk and mesenteric arteries (superior, inferior). Abdominal toad can develop under the influence of both internal ( thrombosis ) and external factors (traumatic occlusion).
What is an occlusive dressing?
This method of sealing the lesion is used for wounds that require maintaining sterile conditions and protection from the external environment.
Applying an occlusive dressing to the knee joint requires certain skills and technique:
- cover the wound surface with sterile gauze;
- Place the top of the scarf on the thigh area and wrap it around the waist;
- bend the bandage at the base by 2 cm;
- cross the ends under the thigh, tie knots on the thigh;
- Throw the top over the knot formed and then pass it under the knot.