The tricuspid valve is a movable septum between the right ventricle of the heart and the right atrium. The valve is involved in blood circulation, through it blood flows from one part of the heart to another. Violations in this part lead to overload of the right side of the heart, provoke a circulatory failure, worsen the patient’s quality of life, and even threaten death. An effective treatment method is valve surgery, during which its structure and mobility are restored.
Description of the procedure
The heart is divided into chambers, and blood circulates between them through valves. There are four valves in total in the heart, and failure of even one causes severe damage to health. The tricuspid or tricuspid consists of three leaflets that open and close during the heartbeat. When the valves open, blood passes through them and enters the right atrium from the right ventricle. The flaps close tightly to prevent blood from flowing back.
Content:
- Description of the procedure
- When is plastic surgery indicated?
- Preparation for valve repair
- Carrying out the operation
- Postoperative period
- Plastic results
- Where is tricuspid valve repair performed?
If the valve does not open completely, it is called stenosis. In this case, the blood flow is disrupted and the ventricle is overloaded. If the leaflets do not close completely, this is called tricuspid insufficiency.
Tricuspid valve repair is intended to restore its function.
This is a rather complex surgical intervention, which is always performed under general anesthesia, most often using a cardiopulmonary bypass machine (ACB). Depending on the problem (stenosis or insufficiency), the appropriate tactics are chosen.
With stenosis, the valves may fuse or thicken; during surgery, they are manually separated and sutured in the right places. If insufficiency is diagnosed, sutures are placed around the circumference of the valve to restore the valve.
As a result of such actions, normal blood circulation is restored and the load on the heart is reduced.
Often, for effective treatment, special rings and half-rings are installed at the time of surgery. These structures can be artificial or biological; the latter are preferable, as they are more easily accepted by the body and do not require lifelong medication. The rings are sewn along the perimeter of the valve apparatus, they restore the required lumen and ensure normal closure of the valves.
Moreover, such reconstruction provides a long-lasting result, since it does not allow the fibrous ring to re-expand. Also, plastic surgery of the tricuspid valve may involve complete excision of its leaflets and replacement with an implant. Such measures are resorted to when it is impossible to rehabilitate the original valves.
Annuloplasty on support rings
Severe dilatation of the right atrioventricular orifice requires implantation of rigid (Carpentier-Edwards), flexible (Duran) corrective rings or tape (Cosgrove annuloplasty system). The length of the base of the septal leaflet of the tricuspid valve (intertriangular distance) determines the size of the ring or band. To fix the corrective rings, 3/0 mattress sutures are used around the circumference of the tricuspid valve ring, avoiding their placement in the area of the atrioventricular node (apex of Koch’s triangle) to prevent the development of atrioventricular block.
Tricuspid valve annuloplasty on a rigid Carpentier-Edwards ring. The result is competent closure of the valve due to the anterior and septal leaflets. The tightness of the tricuspid valve must be checked at the end of the operation. Identified residual regurgitation can be eliminated by applying an O.Alfiery suture. We have developed a method of ring plastic surgery using a soft xenodiaphragm ring. The latter is cut out immediately before implantation. The size of the ring is selected based on a template along the length of the base of the septal valve. The deformability of the soft ring allows the tricuspid valve to change shape during the cardiac cycle, reducing stress on the sutures. In addition, it is possible to dose-out eliminate residual regurgitation by further reducing the diameter of the ring by tying the sutures together.
Tricuspid valve annuloplasty on a soft xenodiaphragm ring
When is plastic surgery indicated?
Such manipulations are carried out in two cases: when the doors open poorly and when they do not close completely. This can happen due to acquired diseases or congenital anomalies. Congenital pathologies of the tricuspid valve are very rare. Typically, valvular disorders are caused by acquired ailments:
- heart injuries;
- infectious diseases;
- systemic lupus erythematosus;
- rheumatism of the heart muscle;
- carcinoid syndrome.
Stenosis and insufficiency in the tricuspid septum are very rarely independent diseases. As a rule, these are consequences of other pathologies. Problems with the mitral valve, located on the left side of the heart, place stress on the right side.
As a result, the right atrium and ventricle cannot cope with the load, and the valve is deformed. Disturbances in the functioning of the valve apparatus may not manifest themselves at first, but over time the patient feels:
- strong heartbeat;
- shortness of breath;
- swelling of the lower extremities;
- chest pain;
- bloating;
- weakness, frequent fatigue.
Also, disruptions in this area are accompanied by enlargement of the jugular veins. Even the patient himself can distinguish swollen veins in the neck. The skin becomes an earthy yellow color, as the liver often also suffers due to impaired blood circulation.
Nausea, belching, and heaviness in the abdomen may occur periodically. The need for plastic surgery is determined only after a thorough examination and clarification of the diagnosis.
And Ebstein's anomaly is a rare heart defect, which is characterized by displacement of the septal and posterior leaflets of the tricuspid valve into the cavity of the right ventricle (RV), dilatation of the fibrous ring, limited mobility of the anterior leaflet of the tricuspid valve, as well as changes in the wall of the RV itself. The degree of displacement and other anatomical features vary (Fig. 1).
Rice. 1. Anatomy of Ebstein’s anomaly: 1 – right atrium; 2 – left atrium; 3 – fibrous ring of the tricuspid valve (TV); 4 – atrialized part of the right ventricle; 5 – septal valve of the TC; 6 – front flap of the TC; 7 – right ventricle; 8 – mitral valve; 9 – left ventricle
These patients often suffer from various arrhythmias - paroxysmal supraventricular tachycardia, atrial fibrillation and flutter, which, in turn, adversely affects the prognosis of these patients. Even after radical correction of the defect, including the elimination of arrhythmias, there are frequent cases of recurrence of the original types of arrhythmia, as well as the appearance of new, sometimes more dangerous, even life-threatening forms, such as sustained ventricular tachycardia and ventricular fibrillation. Therefore, timely detection, recognition and treatment of cardiac arrhythmias in patients with Ebstein’s anomaly can not only improve their quality of life, but also prevent severe complications, and also reduce the risk of sudden cardiac death [1]. The purpose of this report is to present a case of successful re-replacement of the tricuspid valve with a biological prosthesis 26 years after the first operation and immediate elimination of atrial flutter using cryoisolation of the base of the right atrial appendage and the area of the right isthmus of the heart using Atri Cure in a patient with Ebstein's anomaly. Patient V., 34 years old, was admitted to the department of surgical treatment of interactive pathology at the Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev RAMS. At the age of 13 years (in 1987) at the Institute of Surgery. A.V. Vishnevsky, the patient successfully underwent a relatively rare operation for that time - replacement of the tricuspid valve with a biological prosthesis made from the aortic valve of a pig. Over the subsequent period, the patient was regularly examined by a cardiologist. Only 10 years after prosthetics, calcification of the prosthetic valves with insufficiency of I–II degrees was diagnosed. Due to the fact that there were no clinical manifestations of the identified prosthesis dysfunction, dynamic observation was recommended. Since his health remained satisfactory, the patient stopped seeing a cardiologist and did not comply with the prescribed therapy. The first complaints appeared in the early autumn of 2011. Shortness of breath appeared and worsened with moderate physical activity; in the evening, swelling in the legs began to appear, and a feeling of heaviness in the right hypochondrium when walking quickly. In July 2012, a patient with the above complaints and signs of anasarca was hospitalized in a hospital, where after treatment his condition improved, but subsequently the symptoms of heart failure recurred and progressed: his health worsened, shortness of breath increased, swelling appeared in the legs and on the anterior surface of the abdominal wall . There were also complaints about interruptions in heart function. In serious condition, with symptoms of stagnation in the systemic and pulmonary circulation, the patient was admitted to the Scientific Center for Cardiovascular Surgery named after. A. N. Bakuleva RAMS. Upon admission, moderate cyanosis of the skin, cyanosis of the mucous membranes, pastosity of the legs, and a respiratory rate of 18–22 per minute were noted. Heart sounds are muffled, pulse is arrhythmic (during auscultation). A systolic-diastolic murmur is heard in the area of the xiphoid process and to the right of the sternum. Heart rate and blood pressure remained within normal limits – 60 beats/min and 125/90 mmHg. Art. respectively. The liver protruded from under the edge of the costal arch by 4 cm. Electrocardiography determined the irregular shape of atrial flutter, with a conductivity of 4:1. According to the results of Holter monitoring, atrial flutter was recorded with various delay intervals in the AV node, with a ventricular rate from 60 to 180 beats per minute, complete blockade of the right bundle branch. Ectopic activity from the area of the outflow tract of the pancreas, represented by 790 monomorphic ventricular extrasystoles, was also recorded. X-ray examination revealed a sharp increase in the pulmonary pattern, venous congestion in the pulmonary circulation, bulging of the pulmonary artery arch, expansion of the superior vena cava, a sharp increase in the right parts of the heart, and a cardiothoracic index (CTI) of more than 65%. A transthoracic echocardiographic study revealed that the left ventricle is pushed aside by the right parts, RV EDV 130 ml, RV ESV 80 ml, LVEF 61%; LV EDV 96 ml, LV ESV 38 ml, RV EF 40%. The dimensions of the right atrium are 6.3x6.6 cm. In the tricuspid position, the prosthesis has pronounced calcification of the leaflets, the leaflets are motionless, the opening between the leaflets is 0.7–0.9 cm. Second degree regurgitation. Taking into account the patient’s complaints, medical history and data from laboratory and instrumental research methods, the following diagnosis was established: “Congenital heart disease: Ebstein’s anomaly. Condition after replacement of the tricuspid valve with a biological prosthesis in 1987. Dysfunction of the prosthesis: stenosis and insufficiency. Persistent form of atrial flutter." Surgical treatment is indicated. The patient's consent was obtained. On October 19, 2012, a tricuspid valve reprosthetic operation was performed using a biological prosthesis “Bioglis” No. 28 and cryoisolation of the right atrium appendage and the area of the right isthmus using the Atri Cure system (surgeon - Academician of the Russian Academy of Sciences and Russian Academy of Medical Sciences L.A. Bockeria). Progress of the operation: a median resternotomy was performed along the old scar. Total adhesive pericarditis is noted. Due to the fact that during the first operation the pericardium was not reduced, the right sections and the aorta were soldered to the sternum, which made cardiolysis extremely difficult. After the right heart and aorta are isolated from the adhesions, cannulation of the aorta and separate cannulation of the vena cava are performed. CPB was started with hypothermia at 24 C°. After clamping the aorta, cardioplegia was started into the aortic root with Custodiol solution. The right atrium is opened. A biological prosthesis implanted above the coronary sinus is visualized (Fig. 2).
Rice. 2. Xenoprosthesis in the tricuspid valve position 21 years after implantation of the bioprosthesis
The valves of the prosthesis are calcified and immobile. Hole 7 mm. The prosthesis has been removed. Cryoisolation of the base of the right atrial appendage and the area of the right isthmus was performed using the Atri Cure system. A biological prosthesis “Bioglis” No. 28 was implanted in the tricuspid position. The coronary sinus did not move. Warming of the patient has begun. The right atrium is sutured. The vena cava is released, filling the chambers of the heart with the prevention of air embolism. The aorta, which was clamped for 90 minutes, was released. When cardiac activity is restored, an atrial rhythm is observed with a frequency of 50 beats/min. The rhythm is imposed from an external pacemaker with a frequency of 100 beats/min. Stabilization of hemodynamics. The artificial circulation was completed, which lasted 118 minutes. After neutralization of heparin with a calculated dose of protamine, the aorta and vena cava were decannulated. Hemostasis has been completed. The wound is sutured in layers. Drains were installed in the pericardial cavity and in the anterior mediastinum. The postoperative wound is treated with an antiseptic and an aseptic bandage is applied. The patient was transferred to the intensive care unit on minimal cardiotonic support: dopamine 6 mcg/kg/min. He was extubated after 10 hours and transferred to the department on the 2nd day after surgery. The postoperative period proceeded without complications. The patient was discharged home on the 12th day after surgery in satisfactory condition under the supervision of a cardiologist at the place of residence with recommendations. There are no complaints upon discharge. The skin and visible mucous membranes are pale pink. There is no swelling. The respiratory rate is 14 per minute. Breathing is vesicular, no wheezing. Heart sounds are muffled, atrial rhythm with a frequency of 80 beats/min. Blood pressure 115/80 mm Hg. Art. The liver does not protrude from under the edge of the costal arch. According to echocardiography: RV EDV 105 ml, RV ESV 60 ml. The pressure gradient on the TC prosthesis is 4 mm Hg. Art. According to radiography: the pulmonary fields are airy, without fresh infiltrative changes. Discussion The greatest experience in surgical treatment of Ebstein's anomaly has been accumulated at the Scientific Center for Cardiovascular Surgery named after. A. N. Bakuleva. By 2013, the Center had operated on more than 350 patients with this defect. According to the literature, the rate of bioprosthesis destruction by the 10th year after surgery is 30%, reaching 39–63% by the 15th year. At the same time, a number of authors provide data on quite satisfactory results from the use of a bioprosthesis in the position of the tricuspid valve both after 10 and 15 years [2, 3]. Due to its anatomical features, Ebstein's anomaly is primarily accompanied by various disturbances in the rhythm and conduction of the cardiac impulse. The most typical are blockade of the right bundle branch, supraventricular tachycardia with the participation of accessory pathways, less often - atrioventricular block, atrioventricular nodal reentrant tachycardia, fibrillation and atrial flutter [4]. Currently, in many cases, a two-stage defect correction method has been adopted. First, arrhythmias associated with Ebstein's anomaly are eliminated using catheter ablation, and later the tricuspid valve is replaced. There are often cases of simultaneous correction, which, however, can lengthen the time of artificial circulation and adversely affect the outcome of the operation. However, ablation is not always successful, which is due to the presence of multiple additional atrioventricular connections, the anatomical features of their location, and difficulties in fixing the catheter due to dysplasticity and unevenness of the fibrous ring of the tricuspid valve. In addition, as already indicated, in repeat patients the range of arrhythmias is much wider and the degree of resistance of these arrhythmias to treatment is extremely high. The ablation process itself in some patients can lead to modification of excitation conduction and the development of new arrhythmias that form under conditions of other electrophysiological parameters and require repeating this procedure [5]. The presented clinical example illustrates a case of simultaneous elimination of arrhythmia and re-replacement of a calcified biological prosthesis of the tricuspid valve. Cryoisolation of the places where arrhythmia circles form (in this case, the base of the right atrial appendage and the area of the right isthmus) can effectively eliminate arrhythmia without increasing the time of artificial circulation, and also does not require the use of endovascular procedures, which in such cases may be ineffective due to the large number of arrhythmogenic tricks, and due to the lack of direct visual control of the procedure being performed. Conflict of interest No conflict of interest declared.
Preparation for valve repair
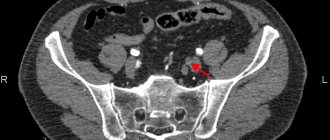
The first step in patient preparation is diagnosis. To clarify the diagnosis, a chest ultrasound, ECG, blood and urine tests are prescribed. In some modern clinics, the heart is examined using a computed tomograph. Angiography of the heart vessels and or CT scans show the heart muscle and blood circulation in detail; during the studies, the radiologist can accurately determine tricuspid stenosis or insufficiency. After the tests, the patient undergoes a consultation with a cardiac surgeon, neurologist, and therapist.
If valve disorders are accompanied by additional heart problems, they try to get rid of them before surgery. For example, in case of arrhythmia, the heart rhythm is first normalized. If the clinical picture is complicated by heart failure, a sodium-excluding diet is prescribed. All patients are prescribed a diet a few days before the procedure; they need to avoid salt, too fatty foods, too spicy foods, and drink less water. You cannot eat 8 hours before plastic surgery. As part of the patient's preparation, the attending doctor explains to his patient how tricuspid valve repair is performed. It is important that the person being operated on does not worry and does not overload the heart and nervous system. If you have concerns or fears, you should talk to your doctor about it.
Diagnosis of tricuspid heart valve disease in Israel
In the presence of cardiovascular pathologies, it is very important to conduct the examination quickly and efficiently, since any delay may worsen the patient’s condition.
- Day 1
- Day 2
- Day 3
First day. From the airport to a doctor's appointment
Immediately upon arrival in the country, the patient, accompanied by a representative of the international department, goes to the clinic. A cardiac surgeon is already waiting for him there. The specialist conducts an examination, studies the data from the studies performed, and, if necessary, prescribes additional ones.
Second day. Comprehensive examination in one day
- Laboratory tests of urine and blood.
- CT, MRI.
- Angiography of blood vessels.
- Chest X-ray.
- Auscultation.
- Electrocardiographic study.
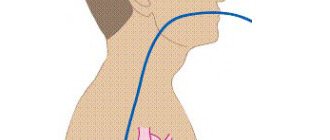
- Echocardiography traditional and transesophageal.
- Bicycle ergometry.
- Cardiac catheterization if necessary, etc.
The third day. Individual treatment plan
Assessing the results of tests and studies, the council of doctors decides which drugs and in what dosage should be chosen for drug therapy and whether surgical intervention is necessary (if so, to what extent). Taking into account the characteristics of the course of the disease, the condition and age of the patient when planning treatment tactics allows us to achieve high efficiency and avoid medical errors.
Carrying out the operation
Reconstruction of the valve apparatus occurs in a hospital setting, in the operating room. Before this, the patient is given premedication: sedatives and hypnotics are administered intravenously. Throughout the entire process, assistants will monitor the patient’s condition using connected equipment. When sleep comes, the surgical team begins manipulations.
- The surgeon makes an incision in the chest. If you get to the heart through the intercostal space, you won’t have to cut the sternum bones. In most cases, the doctor opens the chest, then gets to the valve layer by layer.
- The heart is forcibly stopped and a heart-lung machine is connected. During the process, this device will saturate the blood with oxygen and give it the desired temperature while the heart is “turned off.”
- Then the surgeon’s actions will depend on the pathology itself. To restore the lumen, the valves can be cut and sutured; most often, sutures are placed around the circumference of the valve. There are several suturing techniques; for moderate dilatation, de Vega sutures are usually used. If valve closure is corrected, rings, half rings or tape are most often sewn in. The implantation of such structures is called “annuloplasty”. If it is impossible to restore the function of the tricuspid valve, its leaflets are removed and a prosthesis is placed in their place.
- Before turning off the AVR, the doctor checks the operation of the operated or prosthetic valve. The shortcomings are corrected, the heart-lung machine is turned off.
- The incision site is sutured in layers, the external seams are treated with sterilizing agents. Then apply a tight bandage.
- The patient's condition is assessed again and he is transferred to the intensive care unit. When the anesthesia wears off, the patient is placed in an intensive care unit.
After the operation, the patient remains under the supervision of doctors for another week. This is necessary in order to monitor the results of plastic surgery and prevent complications. In the first days, bed rest, moderate drinking, and diet are indicated. After the final check, the patient is discharged home.
Tricuspid valve replacement
Organic damage to the tricuspid valve and the impossibility of plastic correction requires valve replacement. The algorithm for choosing a prosthesis should take into account the patient’s age, contraindications to anticoagulant therapy, gender and social problems. In order to prevent thrombosis and thromboembolic complications, it is most preferable to use bioprostheses. In the tricuspid position, taking into account less stressful hemodynamic conditions, the degeneration of biological tissue occurs more slowly and, in this regard, their durability is significantly greater than when implanted in other positions. In addition, the use of a bioprosthesis in all cases makes it possible to preserve the subvalvular apparatus of the tricuspid valve, which is especially important in case of reduced contractility of the pancreas (EF<30%). The technique of safe fixation of the prosthesis requires careful attention when placing sutures in the projection of the apex of Koch's triangle. Therefore, it is preferable to perform valve replacement on a beating heart, since the implementation of this stage is monitored by ECG. 2/0 mattress sutures on pads are used to capture the tissue of the fibrous ring. When fixing mechanical prostheses, everting sutures are carried out from the atrium; for implantation of biological prostheses, intraannular sutures can be used. This technique does not require excision of the tricuspid valve leaflets.
Technique for replacing the tricuspid valve with a mechanical prosthesis while preserving the subvalvular structures It is necessary to strive to implant the largest possible diameter of the prosthesis in the tricuspid position, since both bio- and mechanical prostheses with an internal diameter ≥ 27 mm do not have clinically significant gradients. Replacing the tricuspid valve with an allograft (cryopreserved mitral valve) is more complex. After calibration based on intratriangular distance measurements, the papillary muscles of the allograft are fixed to the patient's papillary muscles or directly to the wall of the right ventricle. This requires precise adherence to the chord length of the implanted valve to achieve tight closure of the leaflets. The fibrous ring of the allograft is fixed with a 3/0 continuous suture to the tricuspid valve ring, avoiding damage to the conduction tract. To prevent recurrence of dilatation of the tricuspid valve ring, it is necessary to additionally implant a corrective ring.
Postoperative period
During discharge, the doctor gives his patient instructions on nutrition and lifestyle, and sets a date for the next examination. In the postoperative period, you must follow a prescribed diet, which will exclude:
- fat;
- roast;
- too spicy and salty.
During recovery, stress has a very adverse effect, so it is important to ensure a calm and measured pace of life. If necessary, the attending physician can prescribe medications to support the nervous system if the patient is overly sensitive. Alcohol is completely avoided in the first month after valve reconstruction. It is also important to quit smoking. Visits to the doctor will be scheduled; at first, examinations are scheduled every month, if there are no complaints. It is worth visiting a doctor unscheduled in the following cases:
- bleeding from the wound, swelling, itching in this part;
- constant chest pain (may be at first);
- causeless fever;
- frequent dizziness and nausea.
During the appointment, the cardiologist will listen to your heartbeat, breathing rhythm, and measure your blood pressure. Diagnostics are also periodically indicated: ultrasound, ECG, tests. This is necessary in order to track the rehabilitation process.
Physical activity should be moderate, it is recommended to walk in the fresh air more often, and the step should be leisurely.
Your doctor will tell you when you can return to full activity. Drug treatment is also prescribed to maintain the functioning of the heart and the whole body. If a biological prosthesis was implanted, anticoagulants are indicated in the first three months. If an artificial prosthesis was sewn in, anticoagulants are indicated for life.
Plastic results
Symptoms of stenosis or tricuspid insufficiency disappear immediately after surgery. In the first 1-2 months after it, the patient’s condition will gradually improve if the manipulations went without complications. Negative consequences may include:
- bleeding;
- heart attack;
- formation of blood clots and blockage of blood vessels;
- disturbances of vision, appetite, sleep (this is normal, goes away within a month);
- infection;
- hemolytic anemia.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
To prevent such consequences, scheduled and unscheduled inspections are prescribed. In most cases, the prognosis for tricuspid valve surgery is positive, heart function is restored, and the patient returns to his normal lifestyle.
The postoperative period is complicated by the use of anticoagulants, which reduce blood clotting. Biological implants do not require constant use of anticoagulants, but the lifespan of such prostheses is limited. Observations of patients show that a biological implant lasts an average of 9-10 years.
Mechanical analogues have a long service life; they keep the heart functioning for 20-25 years. But during this entire time you need to take medications that reduce blood clotting. When the life of the implant has passed, it is replaced with the next one. If regular sutures were used during plastic surgery, reoperation may not be necessary. However, long-term patient survival is higher with rings than with conventional suture techniques.
Treatment of tricuspid heart valve disease in Israel: prices
Today, medical care abroad from leading world-famous specialists is becoming available to more patients. At the Top Ichilov Clinic, high quality service, modern diagnostics, innovative methods of therapy and a stay in the comfortable conditions of luxury rooms will cost 30% less than in Europe, and 50% cheaper than in America.
Treatment of tricuspid heart valve disease in Israel, the cost of which is unreasonably inflated in other countries, is chosen by more and more patients, even from developed countries of the world. You can find out prices for the procedures you need from our consultants - leave a request or call the international department of Top Ichilov.
Top Ichilov Medical Center is your best solution
Treatment of tricuspid heart valve disease in Israel, according to reviews from patients at the Top Ichilov clinic, has many advantages. The main ones are highly qualified doctors, advanced equipment and progressive techniques, and affordable prices.
- The authority of our clinic's cardiac surgeons is recognized by the global medical community.
- An individually developed treatment regimen allows one to achieve one of the highest cure rates for cardiovascular diseases.
- Surgical interventions are carried out through low-traumatic, gentle approaches to the beating heart, which reduces the occurrence of risks to zero during or after surgery.
- A comprehensive diagnosis of tricuspid heart valve disease in Israel is performed in just 3 days.
- Loyal pricing policy, convenient payment forms and no prepayment.
- Accompaniment of a representative of the international department throughout the entire stay in the clinic - we are responsible for solving all organizational and everyday nuances.
- 5
- 4
- 3
- 2
- 1
(9 votes, average: 5 out of 5)