Combined phlebectomy is a surgical method for the treatment of varicose veins of the saphenous veins of the lower extremities, aimed at removing pathologically altered veins. In this case, several surgical techniques are used simultaneously. When the pathological main vein is removed, the problem of its recanalization and restoration of pathological reflux in it disappears. As a rule, combined phlebectomy is used in situations where one surgical technique or other methods of treatment (isolated RFO, EVLT) for varicose veins may be ineffective, in some cases can lead to recurrence of varicose veins, complications, or there are initially contraindications to them execution.
The purpose of combined phlebectomy
at the present stage is to normalize or reduce disturbances in venous outflow from the lower limb by solving the following problems: eliminating reflux (vertical and horizontal) - pathological reverse flow in the venous system resulting from pathological changes in the vascular wall and valve apparatus; removal or elimination of varicose veins, as a pathological container with the possible formation of blood clots. In addition to the medical result, a good cosmetic result is achieved.
Despite the emergence of high-tech treatment methods (RFO, EVLT), combined phlebectomy is still considered the “gold standard” in surgical phlebology, the effectiveness of which has been confirmed by decades of practice. At the first stage, the so-called crossectomy, the main saphenous vein is isolated at the place where it flows into the deep vein, after which the vessel is crossed and ligated, the tributaries are crossed and ligated in this place. The second stage is the phlebectomy itself, during which the severed vein is removed using various techniques. The third stage - miniphlebectomy - removal of the tributaries of the main saphenous vein, incompetent perforating veins. In our clinic, combined phlebectomy is used in combination with RFO and sclerosis of tributaries, which eliminates the need for additional incisions. The technical and tactical features of this surgical intervention, developed by specialists at our clinic based on an analysis of 10-15-20 year long-term results in 2.5 thousand patients, allow us to minimize surgical trauma, accelerate healing, shorten the rehabilitation period and achieve good long-term results.
Find out the cost by phone: +7
Duration about 120-150 minutes
Time in hospital 1-2 days
Indications and contraindications
Indications
- varicose veins, including with edema and trophic disorders, thrombophlebitis;
- indurative (ulcerative) form of postthrombotic disease;
- venous malformation of the lower extremities.
Contraindications
- pregnancy;
- severe somatic diseases in the acute period;
- atherosclerosis of the arteries of the lower extremities;
- acute deep vein thrombosis of the lower extremities;
- infectious skin diseases in the surgical area.
Endovascular laser ablation
EVLT is a modern method of combating varicose veins using a laser. The operation is low-traumatic and therefore absolutely painless. EVLT is prescribed for:
- elimination of cosmetic defects in the form of varicose veins;
- elimination of pathological symptoms;
- preventing lymphovenous stagnation;
- prevention of complications (thrombosis, trophic skin defects, ulcers, pigmentation, etc.).
Contraindications to EVLT are:
- inflammation of the skin at the site of the planned operation;
- ischemia, heart attack, stroke;
- pulmonary failure;
- infectious diseases;
- pregnancy and lactation.
Endovascular ablation in the ACMD clinic is carried out using a radial high-tech laser under continuous ultrasound control. A probe with a laser emitter is inserted into the lumen of the affected vessel through a small puncture, which seals the walls of the vessel.
EVLT can be combined with miniphlebectomy, which allows you to achieve the desired therapeutic result without significant tissue trauma. The procedure takes place quite quickly (from 40 minutes to 1 hour) and is accompanied by a short rehabilitation period without the risk of bleeding, tissue scarring and the appearance of scars.
Doctor's comment
You have been prescribed a combined phlebectomy, and you are experiencing quite natural anxiety about the upcoming operation? Our clinic uses the most modern methods of treatment and diagnosis, including original techniques and their modifications to avoid additional tissue trauma. In addition, thanks to a special technique and tactics of execution (invagination PIN stripping of the large and (or) small saphenous veins with special proprietary probes), making mini-incisions along the bikini line, using absorbable intradermal sutures, we manage to achieve good and excellent cosmetic results - postoperative Scars after healing after 2-3 months are almost invisible. Moreover, the combined phlebectomy techniques used in our clinic minimize hospital stay. This operation is performed under anesthesia, so any painful sensations and the patient’s “presence” at the operation are excluded. We are against a single template for treating patients with chronic venous disease. For each patient, we select a set of surgical intervention techniques based on the individual characteristics of the course of the disease, the presence and severity of concomitant pathology, physical and social activity, attitude towards one’s disease, and motivation for a good long-term result. Make an appointment and you will learn everything about the nature and prognosis of your illness. Together with you, we will draw up not only a detailed preoperative examination plan to exclude risk factors and contraindications to treatment and anesthesia, but we will also determine the optimal set of surgical intervention techniques for you, allowing you to minimize the risk of possible complications and relapse of the disease. Based on our experience, the principles of continuity in treatment and family medicine, the “open door” principle, when the patient has the right to contact the operating surgeon if necessary at any time. We will determine the frequency of further follow-up examinations for timely detection and minimally invasive outpatient elimination of disease relapse and correction of conservative treatment. Considering the chronic, multi-cause nature of varicose veins, we have moved away from the impersonal “operate and forget” system to a lifelong monitoring system, including annual ultrasound angioscanning. Together with you, we will try not only to save you from severe manifestations of the disease and its possible relapse, but also to significantly improve the quality of your life in the future.
Head of the Vascular Surgery Center Girsiashvili Aleko Givievich
Why is it better to perform combined phlebectomy at the Swiss University Hospital?
- In our Center for Vascular Surgery and Phlebology, operations are carried out using proprietary methods (in particular, invagination PIN stripping using special probes), thanks to which it was possible to reduce the trauma of surgical intervention, which leads to faster healing and a reduction in the duration of the rehabilitation period, improving the quality of life.
- We were one of the first in the country to use minimally invasive techniques as part of combined phlebectomy in the treatment of patients with chronic venous diseases; we own more than 40 patents for bloodless operations.
- Vascular surgeons (phlebologists) of our clinic have many years of experience in performing surgical interventions, each of our specialists is fluent in all the techniques used in our clinic. Each surgeon has performed more than 2,500 successful operations for varicose veins with analysis of long-term results.
- Ultrasound diagnosis of diseases of the main veins of the lower extremities and the exclusion of local contraindications before scleroobliteration, ultrasound control of the scleroobliteration procedure is carried out by vascular surgeons (phlebologists) using expert-class equipment at the highest professional level. Doctors of the Center for Vascular Surgery are certified specialists of the highest qualification category with an academic degree.
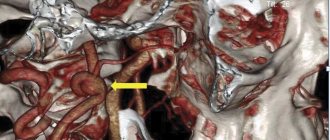
- We have developed and put into practice a protocol for ultrasound duplex scanning of the veins of the lower extremities, which allows not only to map in detail varicose veins and their sizes, but also to accurately determine the variants of pathological reflux with the location of sources of reflux, routes of spread of reflux, channels of blood return to the deep vein system. This protocol allows you to adequately select the method and scope of minimally invasive surgical intervention. Thus, in our practice, the number of tactical errors associated with the choice of method and volume of surgical intervention has significantly decreased, which has a qualitative impact on the results.
- The Vascular Surgery Center is equipped with expert-class equipment from world-famous manufacturers (such as Karl Storz, Covidien, ACUSON-Siemens, Valleylab, etc.). Cooperation with leaders in equipment production makes it possible to be several years ahead of other clinics and be one of the first to apply innovative technologies, scientific and medical developments in practice. To perform combined phlebectomy, we use, in addition to proprietary, low-traumatic surgical instruments, certified disposable surgical instruments.
- We provide treatment in accordance with international standards, the quality of the services provided is assessed by international organizations that regularly visit our clinic to verify compliance with international standards.
- For each patient, we select a set of surgical intervention techniques, based on the individual characteristics of the course and severity of varicose veins, the presence and severity of concomitant pathology, physical and social activity, attitude towards one’s disease, and motivation for a good long-term result.
- We strictly and unswervingly adhere to the principles of continuity of treatment and family medicine, the principle of “open doors”, when the patient has the right to contact the operating surgeon if necessary at any time.
- Considering the chronic nature of the course of chronic venous diseases and the tendency to relapse, we have moved away from the impersonal “operate and forget” system to a lifelong monitoring system, including annual ultrasound examination.
- We will determine the frequency of further follow-up examinations and examinations for timely detection and minimally invasive outpatient elimination of recurrent varicose veins and correction of conservative treatment.
- When determining whether a patient is suitable for combined phlebectomy, we do not follow his wishes, observing, first of all, the principle of “do no harm.”
- Together with you, we will try not only to save you from severe manifestations of chronic venous diseases and possible relapse of varicose veins, but also to significantly improve the quality of your life in the future.
Miniphlebectomy: the essence of the procedure
Miniphlebectomy is the removal of varicose veins through small punctures in the skin under local or general anesthesia. Indications for surgery are:
- phlebeurysm;
- thrombophlebitis and thrombosis;
- varicose nodes.
Miniphlebectomy is not performed during pregnancy, lactation, or in the presence of acute chronic heart disease, pulmonary insufficiency, infectious diseases and hypertension.
The operation is performed through very small (up to 2 mm) punctures in the skin, after which there are no scars. After the procedure, it is recommended to wear compression stockings and be observed by a phlebologist for 1 year.
FAQ
Is special preparation required for combined phlebectomy?
On the eve of the operation, you should take a shower and remove hair from the limb and groin area. The procedure is carried out on an empty stomach, so the last meal is no later than 18:00 the evening before. There may be additional individual recommendations.
How is combined phlebectomy performed?
Before the operation, under the control of ultrasound duplex scanning with the patient in a “standing” position, the affected vessels to be removed are marked: the boundaries of the incompetent valves of the main veins are marked, the confluence of the tributaries is determined, etc. Thus, this makes it possible to determine the individual volume, nature of the surgical intervention and tactics for its implementation. The operation consists of several stages. Crossectomy is the intersection of the pathologically altered main saphenous vein at the point of its confluence with the deep vein, which leads to cessation of blood flow and elimination of reflux. The incision during crossectomy, as a rule, runs along the inguinal fold or along the popliteal fold - the location of the incision depends on the location of the lesion. In some cases, in the absence of contraindications, crossectomy can be replaced by endovasal laser obliteration (EVLK) and radiofrequency obliteration (RFO) without the need for incisions.
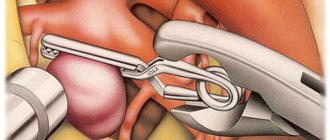
- At the second stage (stripping), the main trunks of the veins are removed using various techniques and instruments; during the intervention, the vein is removed. In our clinic we perform low-traumatic intussusception PIN stripping using special proprietary probes. It should be noted that in some cases alternative techniques are used, their use allows you to do without stripping or crossectomy - endovasal laser obliteration (EVLK) and radiofrequency obliteration (RFO).
- The final stage is miniphlebectomy—removal of tributaries and perforating veins through minimal punctures using special miniphlebextractors. At this stage, deformed veins and nodes that look unaesthetic are removed. The intervention is low-traumatic, there is no need for sutures.
- A prerequisite for phlebectomy is elastic compression of the limb, the duration of which is determined by the operating surgeon, which avoids the appearance of hematomas, bleeding, and swelling after surgery.
Is it possible to perform simultaneous (combined) phlebectomy and surgery for a concomitant independent disease?
Combined (simultaneous) operations
, are considered operations aimed at simultaneous correction of changes in two or more organs due to their independent diseases.
Currently, the extremely low number of simultaneous interventions performed, which does not correspond to the real needs for them, is explained by a number of reasons: incomplete examination of patients in the preoperative period, insufficient exaggeration of the degree of surgical risk when determining the possibility of performing simultaneous operations, the tendency of surgeons to carry out multi-stage surgical treatment of concomitant diseases , increased responsibility of the surgeon in the event of a possible unsuccessful outcome of the operation, psychological unpreparedness of surgeons and anesthesiologists to expand the scope of surgical intervention. In our opinion, this is due to the lack of clear, generally accepted, scientifically based principles of treatment tactics for patients with concomitant diseases. Our clinic's many years of experience allows us to recommend combined (simultaneous) operations for chronic venous diseases, including combined phlebectomy, and concomitant independent non-severe pathology (lipomas, hernias, varicose veins of the spermatic cord, etc.). The decision to perform a simultaneous operation is made collectively after a comprehensive examination, assessment of risk factors and exclusion of contraindications.
How is rehabilitation after combined phlebectomy?
After combined phlebectomy, recommendations mainly concern wearing compression garments and limiting physical activity. A light massage of the limb is possible. These are the main conditions for successful recovery. It is recommended to get up the next day after surgery. Early activation is necessary to prevent postoperative complications. It is better to avoid taking hot baths for two weeks. Showering is allowed after 3-4 days. You should refrain from excessive physical activity and long flights for a period of 3-4 weeks. One of the prerequisites for effective treatment is round-the-clock compression - wearing compression stockings for at least 2 weeks. Then wearing compression garments is recommended only during the daytime. Two months after the operation, an ultrasound examination is required to exclude possible complications, the possibility of early relapse, determine the prognosis of the disease, and correct conservative treatment.
Preparing for surgery
Before the operation, the patient must undergo a standard examination: donate blood for a general analysis, markers of hepatitis C and B, for RW and HIV, and undergo fluorography.
Those over 40 years old must also submit the results of an electrocardiogram and a physician’s report. Sometimes they are supplemented with simple blood clotting tests (to identify disorders of coagulation hemostasis) and Duke bleeding duration (to identify vascular-platelet dysfunctions).
Technique of the procedure
It is aimed at preventing varicose veins and has replaced another technique - excision of varicose tributaries of the main venous vessels according to Narat. During the procedure, special hooks are used, which are inserted through mini-punctures in the skin (with a cross-section of 1-2 millimeters).
- Before the procedure itself, varicose veins are marked on the affected area with their precise positioning.
- Local anesthesia is then performed. Usually, a 0.25 percent solution of novocaine is sufficient for this. Other anesthetics are used if you are allergic to this drug. The substance is injected paravasally. At the same time, you can see how it moves along the bed of the vessel, forming a coupling. Often this approach makes it possible to more accurately identify small branches that were not identified during marking.
- Miniature punctures are made mainly along the lines of force. The distance between the incisions may vary depending on the compliance of the vein, its strength and other factors. It is most convenient to perform punctures in the area where the perforators originate and the veins divide.
- This is followed by the introduction of varixes with hooks, followed by stretching and tearing off the vein from outside the incision. There is no need to ligate (bandage) the veins, since even with active bleeding from the central zone, it is stopped by local compression during the procedure.
- Upon completion of the operation, adhesive stickers are applied to the wounds. The entire area can also be bandaged by placing rollers along the “bed” of the removed veins. A medical knitwear (compression bandage) is put on over everything. The optimal level of compression is the second degree (from 23 mm Hg/st to 32 mm Hg/st).
- After short-term medical observation, the patient is sent home. Staying in the recovery room is not always required.