What is thrombophlebitis
Thrombophlebitis
(acute thrombophlebitis, superficial vein thrombosis, TPV) is an inflammation of the venous walls with further formation of blood clots. The thrombus is tightly attached to the inflamed vessel. If treatment is started in time, the blood clot will resolve, the inflammation will go away, and the venous lumen will be restored and will not affect blood flow.
The incidence of thrombophlebitis is determined by many factors, one of which is age. Thus, superficial vein thrombosis debuts annually in 0.3-0.6 per 1000 people under 30 years of age and in 0.7-1.8 per 1000 elderly patients. There are also gender differences. In men under 30 years of age, acute thrombophlebitis occurs in 0.05 cases per 1000 patients annually. For women, these figures are significantly higher. Thus, in the first 30 years of life, the onset of TPV is detected in 0.31 per 1000 women, but with age the detection frequency increases to 2.2 per 1000 patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
In 3-11% of patients, thrombophlebitis is localized on the lower extremities. The system of the great saphenous vein is affected in 60-80% of cases, the small saphenous vein - in 10-20%, and bilateral TPV occurs in 5-10% of cases i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
Against the background of varicose veins, thrombophlebitis occurs in 4-62% of patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
Folk remedies
Along with drug treatment, traditional methods can give good results. However, you should not blindly believe and thoughtlessly try everything on yourself. The doctor should control the treatment regimen, the admissibility and effectiveness of folk remedies.
- White cabbage. Cabbage leaves need to be softened, one side greased with oil and secured with a bandage on the painful area. Leave the compress on all night.
- Kalanchoe pinnate. Grind the leaves and fill the jar halfway with them. Fill the rest of the jar with vodka. Next, leave for 7 days in a dark place, shaking the contents periodically. Strain the finished tincture. Rub the sore leg from the foot to the groin in the direction of the vein. So for a month 2 rubles/day.
- Apple vinegar. Mix 2 teaspoons of vinegar and honey in a glass of water. Drink half a glass before meals 2 times a day.
- Mumiyo. You can make a tincture for internal use and ointment:
- for the tincture you need to mix 10g of mumiyo with 0.5l of water - drink 1 tablespoon/1 ruble per day, 10 days
- For the ointment, you need to mix mumiyo with Vaseline (or peach oil) in a ratio of 1 to 5 - smear 3 times a day, leave for 1 hour, 10 days.
Types (classification) of disease
Thrombophlebitis is divided into several types, taking into account the origin and origin of the disease, the localization of the lesion, and the extent of the lesion.
Venous thrombophlebitis is divided according to the affected area into:
- Migratory
. A blood clot appears in one place. Over time, it disappears and appears in another area. The condition is dangerous and requires prompt medical attention. - Local
. A blood clot forms in a specific area. It doesn't have to be the shins. For example, thrombophlebitis of the hand is diagnosed.
Depending on the presence or absence of pathogens, subcutaneous thrombophlebitis occurs:
- Septic
. The infection spreads quickly through the bloodstream, so there is a risk of developing sepsis. Diagnosed after childbirth, surgery and erysipelas. Treated with antibiotics. - Aseptic
. There is no infection, the disease occurs after injury. Most often, varicose thrombophlebitis is diagnosed due to improper or absent treatment.
Depending on the size of the blood clot, the disease can be:
- Occlusive
. The lumen of the vein is completely blocked, so the outflow of blood is impaired. There is a risk of necrosis (tissue death), so immediate surgery is required. - Non-occlusive
. An attached blood clot partially blocks the venous lumen. Blood circulates.
Based on the extent of the pathological process, the following is revealed:
- Thrombophlebitis of the superficial veins
. Symptoms appear immediately. The patient complains of pain along the vein. The surrounding skin turns red and thickens. Over time, swelling forms, which is difficult to eliminate. The temperature is kept within 39 °C. Treated with medication. - Deep vein thrombosis
. This form is detected less frequently and is more severe. The symptoms are the same, but their severity is stronger. The limbs become very swollen and turn blue. If there is a high risk of developing pulmonary embolism, surgery is performed.
First, thrombophlebitis of the superficial veins of the lower extremities develops. If left untreated, the disease develops into deep vein thrombosis, thrombophlebitis of the great saphenous vein.
Thrombosis Clinic
Symptoms of thrombosis can be general, regardless of location, or specific.
Common symptoms include pain with movement and at rest, limited mobility, and decreased function of the affected organ or tissue. Symptoms of arterial obstruction (acute thrombosis, or gradual obstruction of vessel patency):
- asymmetry of blood pressure when measured on both arms [7];
- pallor of the skin, turning into cyanosis [7];
- pain at rest at night [7];
- pain when moving in the thigh, buttock, lower leg, foot, shooting or aching [7];
- sleep disorders [7];
- numbness, coldness of the limb [7];
- absence of peripheral pulsation [7];
- necrosis (necrosis) of affected tissues, trophic ulcers, gangrene [7];
- intermittent claudication [7].
Symptoms of venous thrombosis:
- pain [6];
- swelling, soft and asymmetrical [6];
- blue discoloration of the skin (skin cyanosis) [6];
- increased skin temperature of the extremities [6];
- increased sensitivity and compaction in the projection of the superficial veins [2];
- post-inflammatory hyperpigmentation [2];
- dilated saphenous veins [6];
- erythema [2].
Sometimes the only symptom of venous thrombosis is PE [6].
Stages
The sequence of development of the disease is as follows:
- Acute stage
. Clinical signs of thrombophlebitis are bright and appear unexpectedly. The temperature rises, the skin around the affected area turns red, and the patient shudders. If treatment is started within two weeks, the development of the disease can be avoided. The blood clot will dissolve. The duration of exacerbation is up to one month. - Subacute stage
. Lasts up to two months. Signs of the disease subside, but do not fade away. The skin remains red and the swollen veins turn blue. The swelling goes away, but the seals remain. - Chronic stage
. Diagnosed two to three months after the disease is detected. Symptoms are either absent or worsened. During remission, the limbs remain swollen, quickly become tired and itchy, but there is no pain. Discomfort occurs in the lower extremities when walking for a long time.
Causes of thrombosis in the superior vena cava system
The causes of thrombosis in the superior vena cava system are basically the same as other venous thrombosis. It may also develop as a complication of venous catheterization (cubital, subclavian catheter), sometimes arising as a result of prolonged compression or uncomfortable position of the upper limb (for example, during sleep).
The most common is thrombosis of the axillary or subclavian vein (Paget-Schrötter syndrome). Within 24 hours, swelling of the entire upper limb occurs with cushion-like swelling of the hand. There may be slight bursting pain. The color of the limb is unchanged or slightly cyanotic.
How is thrombophlebitis different from varicose veins?
Varicose veins are increased pressure in thinned and inelastic veins, and thrombophlebitis is an inflammation of the venous walls with subsequent formation of blood clots. Most often, the diagnosis of thrombophlebitis is a consequence of varicose veins.
Thrombophlebitis differs from varicose veins in the following symptoms:
| Sign | Varicose veins | Thrombophlebitis |
| Pain | pulling | bursting and stabbing |
| Convulsions | Yes | No |
| Changing the appearance of your legs | noticeable tortuosity and bulging of veins | compactions and lumps when palpated |
| Change in skin color | pale skin, blue veins | red skin |
| Burning feeling | Yes | No |
Both pathologies develop as a result of impaired hemostasis, but inflammation of the venous walls is more often associated with the entry of an infectious agent. The difference is the absence of local inflammation. With varicose veins, the veins do not become inflamed. In this case, only the blood circulation is disrupted.
Complications and prognosis
Complications of superficial thrombophlebitis occur extremely rarely. It is dangerous when a blood clot breaks off and leads to thromboembolism.
However, unlike deep vein thrombosis, which is rarely accompanied by inflammation, superficial thrombophlebitis is usually accompanied by an acute inflammatory reaction, causing the clot to adhere to the vessel wall. The likelihood of it breaking off and entering the bloodstream is very low. In addition, superficial veins, unlike deep veins, are not surrounded by muscles, the contractions of which contribute to compression and displacement of the blood clot, which can lead to its separation. For these reasons, superficial thrombophlebitis is rarely complicated by thromboembolism. However, the possible complications of superficial thrombophlebitis are as follows.
Be sure to tell your doctor that despite treatment for superficial thrombophlebitis, the symptoms do not decrease or increase. Also report any new symptoms such as fever, chills, paleness, or swelling of the extremity. A change in skin color at the site of thrombophlebitis may remain noticeable for a long time after treatment; this is not a pathological symptom.
Causes and risk factors for the development of thrombophlebitis
Thrombophlebitis of the lower extremities rarely begins spontaneously. Most often, the disease becomes a complication of leg diseases. The development mechanism is associated with improper outflow of lymph and blood through the veins and vessels. After injury to the inner layer of the vein, bleeding begins. In response to this, a blood clot forms. It prevents blood loss, but over time it grows and completely blocks the lumen of the vessel, preventing blood from circulating.
The following factors precede this process:
- Damage to the vascular wall. This group includes mechanical injury to veins due to trauma and compression of the limbs. Venous walls are damaged when injections are performed incorrectly, frequent and long IVs, or operations.
- Deterioration of blood supply to certain areas of the body. The blood flows poorly due to wearing a cast for a long time, bed rest and physical inactivity. Less commonly, slowing of blood flow occurs as a result of heart failure.
- Improper flow of blood in the veins due to venous insufficiency. The complication develops against the background of pregnancy and diseases of the pelvic organs.
- Increased blood clotting. The viscosity and homogeneity of blood and plasma change with long-term use of hormonal drugs, discrepancies in the levels of estrogen and progesterone, and infections.
Other causes of thrombophlebitis may be:
- obesity;
- allergic reactions and sensitization;
- a history of venous thromboembolic complications (VTEC);
- taking a number of medications (diazepam, amiodarone, vancomycin, chemotherapy drugs, heroin addiction).
Acute thrombophlebitis often develops against the background of some autoimmune diseases, such as systemic lupus erythematosus, vasculitis, Behcet's and Buerger's diseases. In particular, in Behçet’s disease, TPV is detected in 53.3%, and DVT in 29.8% of patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
The risk group includes:
- Patients with heart disease - chronic heart failure, ischemic stroke. Limbs swell, motor activity decreases, and after a stroke there may be paralysis, which impedes the flow of blood through the veins.
- Patients with concomitant phlebological diseases - varicose veins, venous thrombosis. The speed of blood movement in the veins decreases, the blood stagnates, forming a blood clot.
- Bedridden patients, people with complex fractures. Their mobility is impaired and the likelihood of blood clot formation increases.
- People with a hereditary predisposition. Hemostasis disorders are transmitted genetically. The likelihood of the disease is increased if blood flow pathologies are detected in first-degree relatives.
Who is at risk?
The risk group for developing the disease includes the following categories:
- Pregnant women, women after childbirth and on hormone replacement therapy.
- Patients with a malignant tumor.
- Women who have been using contraceptives for a long time.
- Patients with excessively limited physical activity.
- Patients with pathologies of the venous system.
The likelihood of developing the disease is also high for people:
- Over the age of 60.
- With a previous stroke and episodes of TF.
- Smoking abusers.
- Suffering from obesity.
It is worth remembering that regular physical activity and giving up bad habits stimulate normal blood circulation, which will avoid the formation of blood clots. People who are included in one of the above risk groups should contact a phlebologist for an examination and recommendations for preventive measures.
Symptoms
Signs of thrombophlebitis appear immediately. The disease can be suspected based on the following clinical picture:
- the limb swells;
- the skin over the inflamed vein turns red, and the vessel itself darkens and is clearly visible under the skin;
- a compaction is felt to the touch along the course of the vessel;
- there is a feeling of heaviness in the legs and bloating of the veins;
- in a supine position, the patient cannot lift his leg and rotate his foot;
- The leg is cold to the touch.
At the initial stage, the symptoms are local, that is, the general condition does not change. As the disease progresses, mobility becomes impaired. The patient notes weakness in the legs and cannot stand for a long time. When bending the foot, he feels tension in the lower leg and thigh. Temperatures range from 37°C to 39°C.
Distinctive signs of thrombophlebitis of the lower leg are that the calf muscle turns blue and the veins on it swell. The pain is so severe that the patient cannot step on his foot.
Thrombosis of the iliofemoral vein is manifested by pain in the lumbosacral spine, pain in the groin and the lower third of the abdomen on one side.
Femoral vein thrombosis is characterized by swelling of the veins in the upper thigh and discomfort in the groin area.
History of the study of phlebothrombosis
The study of deep vein phlebothrombosis dates back more than 400 years.
Occlusion of the great veins as a cause of gangrene was first described by F. Hildanus in 1593. The first mention of ileofemoral phlebothrombosis appeared in the medical literature 300 years ago, it was made by Mauriceau.
The concept of “thrombophlebitis” was first introduced into medicine by the English surgeon John Hunter (1728-1793), who performed many operations on gunshot and other wounds and noted the frequency of inflammatory processes combined with the formation of blood clots in the veins.
Interest in deep vein phlebothrombosis increased significantly after the creation of the theory of venous thromboembolism by the outstanding German pathologist R. Virchow. While autopsying the corpse of a young man in 1844 who had suddenly died after developing pain in his thigh, Virchow discovered a blood clot in the right femoral vein and a twisted blood clot in the pulmonary artery. After that, he introduced the concepts of “thrombus” and “embolus” into medical terminology. In 1845, having discovered venous thrombi in 18 cases from 76 autopsies, and in 11 cases revealing the presence of thromboembolism in the pulmonary artery, he came to the conclusion that blood clots form in the veins and are transported by the bloodstream to the pulmonary artery. He also formulated the classical triad, which is still the most complete reflection of the links in the pathogenesis of local vascular thrombus formation.
The first Russian-language monograph devoted to this problem was the work of I.F. Klein "On thrombosis, embolism and ichorremia", published in 1863.
Despite the fact that acute deep phlebothrombosis in various variants of localization and clinical course differ significantly from each other, they are united by the commonality of basic etiopathogenetic processes. The concept of phlebothrombosis as a nosological group is based on the classical Virchow triad.
More than 150 years ago, Rudolf Virchow described the basic mechanisms of intravascular thrombus formation. Its classic triad includes hypercoagulability, vessel wall damage, and slowing of blood flow. Sometimes, for this pathology to occur, a pathological change in only one of these factors is sufficient.
Despite the fact that the thrombotic process can develop at any level of the main veins, in more than half of the cases the starting point of its development in the centripetal direction is the veins of the leg. In the vast majority of cases, thrombosis is primarily localized in the veins of the leg, and subsequently grows proximally into the popliteal, femoral and iliac veins.
It is this type of development that is very often embologenic, since the growth of a thrombus occurs in the direction of veins with an increasing internal diameter, where thrombus masses are not always fixed along the entire perimeter of the vein. Such blood clots are called floating.
One of the main reasons for slow blood flow is immobilization. Under normal conditions, the outflow of blood from the lower extremities is carried out by contraction of the calf muscles, which act as a peripheral pump, pushing blood in a proximal direction, facilitated by the function of the valves. Limiting physical activity significantly disrupts this mechanism. In this case, blood is retained in the venous sinuses of the leg.
The question of the importance of risk factors and trigger factors for thrombosis has been studied in sufficient detail:
- Congenital thrombophilias (deficiencies of various factors of the hemostatic system or their pathological changes)
- Activation of coagulation factors and fibrinolysis disorders (trauma, surgery, neoplasms, pregnancy, childbirth, etc.).
- Pathology of platelets.
- Slowing and/or disruption of blood flow (age over 40 - 45 years, immobilization, pathology of central circulatory mechanisms, obesity, etc.).
- Changes in the rheological properties of blood.
- Damage to the endothelium and vascular wall (contrast agents, intravascular devices, venous catheters, dilatation of veins, etc.).
- Drug therapy (anaesthetics, muscle relaxants, chemotherapy, contraceptives, contrast agents). For example, the incidence of postoperative thrombosis after various surgical interventions can reach 20-59%.
Diagnosis of thrombophlebitis
Diagnosis of the condition of the lower extremities includes:
- Vascular ultrasound in Doppler mode
. The blood flow of the superficial and deep veins is analyzed. Areas of narrowing of the vascular lumen and slowing down of blood flow are identified. - CT venography
. The transition of the femoral vein to the iliac vein is poorly visualized on ultrasound, so computed tomography shows a splash of blood after slow passage through a certain area. It is carried out with contrast enhancement, that is, a dye is injected into the vein. - D-dimer assay
. When a blood clot forms, the amount of fibrin breakdown products in the blood increases. The analysis is performed after an ultrasound. - Blood analysis
. The diagnosis is confirmed by high coagulogram (clotting test) values. The presence of C-reactive protein indicates inflammation. Leukocytes also grow, ESR increases, and the number of rods in the blood increases.
Tests for thrombosis
Laboratory indicators play a significant role in the timely diagnosis of thrombosis.
Thus, guidelines for the management of patients with a new coronavirus infection provide for stratification of the risk of coagulopathy in patients with COVID-19 based on simple laboratory tests: D-dimer, prothrombin time, platelet count, fibrinogen level [1,9]. A clinical blood test can detect inflammation. It also determines the level of platelets, that is, the very substrate of thrombosis.
Additionally, the level of inflammation in the blood and the risk of thrombosis is indicated by an increased level of C-reactive protein.
Biochemical analysis primarily demonstrates blood glucose levels. It can be used to judge the presence of diabetes, one of the most serious risk factors for thrombosis.
Also, a biochemical analysis can determine the level of protein C, which also characterizes the severity of the risk of thrombosis.
Elevated levels of homocysteine in the blood are also a currently proven risk of thrombosis, leading to miscarriage and cardiovascular events (heart attacks and strokes).
D-dimer is a laboratory marker of fibrin formation [8]. It also indicates the presence of inflammation, just like C-reactive protein. The level of D-dimer is a control indicator of COVID-19 and its complications, including those associated with thrombosis.
You can take tests under the comprehensive Thrombosis program, which includes determining the levels of Antithrombin-III, D-dimer and genetic factors of cardiac diseases and platelet levels. This program allows you to determine the fact of thrombosis occurring somewhere in the body, as well as determine the genetic predisposition to it. This program, like other tests, is offered by the CITILAB network of clinics.
Additional determination of homocysteine and C-reactive protein levels will help determine the biochemical risk of thrombosis.
Treatment of thrombophlebitis
Therapeutic actions are aimed at suppressing inflammation, resolving blood clots and thinning the blood.
Drug treatment
venous thrombophlebitis involves taking:
- anticoagulants to thin and prevent blood clotting, in the acute phase are prescribed by injection;
- antibiotics for the infectious nature of the disease;
- angioprotectors to increase the tone of the veins, reduce venous stagnation;
- disaggregants for breaking down cells that form a blood clot;
- phlebotonics to strengthen and increase the elasticity of the walls of blood vessels;
- non-steroidal analgesics to relieve acute pain.
Compression therapy
using bandages, elastic stockings or class 2 sleeves accelerates blood flow in the superficial and deep veins, thereby preventing the growth of a blood clot. In addition, compression has an analgesic effect.
Physiotherapy
– an effective method of treating venous thrombophlebitis. After acute symptoms have been relieved, a course of magnetic therapy, infrared radiation, ultraviolet radiation, or darsonvalization of your choice is prescribed. The procedures reduce inflammation, increase blood circulation, and accelerate the regeneration of the internal walls of veins.
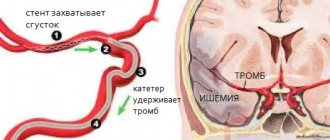
Surgical intervention
is prescribed if the blood clot grows and the threat of blocking the lumen of the vessel increases. There are several types of operations for thrombophlebitis:
- crossectomy – access to the saphenous vein through the groin and an incision in the thigh;
- thrombectomy – access to the thrombus through one incision;
- invagination stripping - with the help of a probe, the vein is everted, the blood clot is removed;
- stenting – the vein is expanded mechanically by installing a special balloon.
Why is it important to undergo treatment in a modern clinic?
Thrombophlebitis can be easily cured without surgery if the patient does not delay going to the doctor and does not self-medicate at home. This is why it is important to see a doctor at the first symptoms. The causes of the disease - inflammation of the vessel wall and blood clotting disorders - can only be eliminated through professional medical care provided by experienced doctors in a modern clinic. Not to mention acute forms of the disease, treatment of which is carried out only on an outpatient basis, since there is a risk of a threat to life.
Recommendations and contraindications for thrombophlebitis
The doctor advises you to follow a diet and wear low-heeled shoes with a comfortable last.
Forbidden:
- wear stilettos and heels higher than 3 cm;
- massage limbs;
- go to the gym and lift weights;
- remove leg hair with wax or epilator;
- go to the bathhouse and sunbathe;
- wear socks, stockings, and knee socks with a thick elastic band.
It is necessary to exclude the use of hormonal drugs and choose a different method of contraception.
General recommendations
You definitely need to change your usual lifestyle - the final result of treatment for thrombophlebitis will depend on how completely you can do this.
General recommendations from doctors are as follows:
- You can't lift weights.
- It is necessary to avoid prolonged standing or sitting - such statistical monotonous postures can lead to deterioration of health.
- Regular physical education – at a minimum, morning exercises and walking, at a maximum – classes in the gym.
- Patients with the disease in question are strictly prohibited from visiting baths and saunas. However, overheating is just as harmful as hypothermia.
- During rest and night sleep, the legs should be in an elevated position - this will ensure the outflow of blood from the lower extremities and prevent congestion in the vessels of the lower extremities.
If the disease in question is diagnosed at an early stage, the effectiveness of treatment will be very high. But even if experts recommend surgical intervention, you should not refuse - such radical treatment usually leads to a complete restoration of the ability to live and work fully.
Sources
- Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23.
- Kuzmichev D.E. Pathomorphological findings. Thrombophlebitis / D.E. Kuzmichev [et al.] // Health care of Ugra: experience and innovations. - 2020. - No. 1. - P. 53-56.
- Marushchak E.A. Modern methods of ultrasound diagnosis of venous thrombosis of the inferior vena cava system / E.A. Marushchak, A.R. Zubarev // Outpatient surgery. Stationary replacement technologies. - 2014. - No. 3-4 (55-56). — P. 38-47.
Treatment and prevention of thrombosis
Treatment of thrombosis includes anticoagulant and antiplatelet therapy, thrombolytic therapy, installation of an inferior vena cava cava filter, and surgical removal of the thrombus [5].
Complications of anticoagulant therapy must be kept in mind: major bleeding, heparin-induced thrombocytopenia and warfarin-induced skin necrosis [5]. To reduce the risk of continued thrombus formation, NSAIDs are used [2]. For the purpose of secondary prevention, small doses of heparin are prescribed. Non-drug treatment methods are also prescribed - elastic bandaging, compression hosiery, local hypothermia and exercise therapy [2, 4].
Prevention of thrombosis includes a number of measures used in situations of increased risk of thrombosis.
Primary prevention of atherothrombosis:
- systematic physical activity in the form of walking or morning exercises;
- blood pressure control, maintaining working blood pressure below 140/90 mmHg;
- control of blood sugar levels (less than 6 Mmol/l), early detection and treatment of diabetes mellitus;
- weight loss, body mass index less than 25 kg per m2;
- a diet limited in cholesterol and high-density fat (total cholesterol less than 5 mmol/l), fruits and vegetables;
- smoking cessation [3,7].
Primary prevention of venous thrombosis:
- compression underwear;
- bandaging with elastic bandages;
- drinking plenty of fluids, especially after surgery;
- regular exercise, walking, especially when traveling;
- prohibition of taking alcohol and sleeping pills in large doses;
- prohibition of the use of compressive shoes and clothing [2,5,6].
Sometimes, during periods of particular risk, anticoagulants are prescribed several days before the flight. There is no point in taking aspirin in such cases [5].
What is the danger of thrombophlebitis of the upper and lower extremities?
The first signs and symptoms of this disease should alert you. You should not trust traditional methods of treatment or hope that the disease will go away on its own. Its complications are extremely serious, and some are even incompatible with life. That is why it is extremely important to undergo a timely examination and begin treatment as early as possible. Thrombophlebitis is curable, and you can get rid of the unpleasant consequences. Qualified treatment will significantly improve your quality of life and relieve unbearable pain in your limbs.