Thrombocytopenia
Thrombocytopenia - what is it?
We will talk about a violation of hemostasis, more precisely, its platelet component, which is characterized by the fact that the number of platelets per unit volume of blood decreases.
Occurs:
- High bleeding from the skin and mucous membranes;
- Bruises and hemorrhagic rashes form;
- Bleeding.
In order to eliminate the problem, it is necessary to resort to drug therapy, splenectomy, and extracorporeal blood purification.
Why do pathologies appear?
All causes of pathologies are divided into two groups:
- Congenital;
- Purchased.
If the pathology is congenital, then it is part of hereditary syndromes, for example, Wiskot-Aldrich syndrome.
With the development of pathology in these cases, as a rule, qualitative changes in platelets also occur.
The causes of acquired pathology are quite diverse: lymphomas, sarcoidosis, portal hypertension, splenic tuberculosis, alcoholism, etc.
The most significant group includes pathologies caused by increased platelet destruction. Moreover, they develop both as a result of the mechanical destruction of platelets and the immune component.
- Alloimmune pathology is provoked by transfusion of blood of a different group;
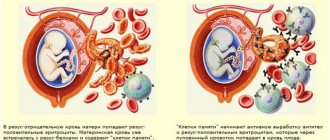
- Transimmune pathology occurs due to the fact that maternal antibodies penetrate to the fetus through the placenta;
- Autoimmune pathology is a consequence of the production of antibodies to one’s own unchanged antigens;
- Heteroimmune pathology occurs due to the fact that antibodies act against foreign antigens that are fixed on the surface of platelets.
- Drug-induced pathology is a consequence of taking sedatives, antibacterial or sulfonamide drugs, and some others.
Note that a slight decrease in the number of platelets can be caused by vaccination or viral infections.
Pathologies that arise due to platelet deficiency develop when there is an insufficient number of stem cells, and thrombocytopenia occurs. This condition may be affected by:
- Aplastic anemia;
- Leukemia;
- Myelofibrosis;
- Presence of metastases in the bone marrow;
- Chemotherapy treatment, some other things.
There are indicators of the severity of thrombocytopenia:
- First stage (satisfactory hemostasis). With it, the platelet count is 150-50x109/l;
- Second stage (sharp decrease in indicator - 50-20 x109/l). This may be the result of a minor injury that causes intradermal hemorrhages or prolonged bleeding from wounds;
- Stage three (platelet count is minimal – 20x109/l). Spontaneous internal bleeding is to be expected here.
Below we will talk about thrombocytopenia, which manifests itself moderately, sharply and severely.
Causes of moderate thrombocytopenia
- Excessive alcohol consumption;
- Pregnancy period;
- Liver pathologies;
- Use of a number of medications;
- DIC syndrome;
- Lupus erythematosus and systemic vasculitis;
- Heart failure;
- Consequences of radiation therapy.
Causes of severe thrombocytopenia
- Systemic lupus erythematosus;
- Significant DIC syndrome;
- Acute leukemia;
- Hemolytic disease of the newborn.
Causes of severe thrombocytopenia
- Acute radiation sickness;
- Overdose of cytotoxic drugs;
- Severe course of acute leukemia.
Symptoms
The manifestations of thrombocytopenia depend entirely on the underlying disease, but it is worth talking about the general signs. Among them:
- Bruises appear inexplicably on the skin;
- The blood slowly stops at the cut sites;
- Often the nose bleeds;
- The oral mucosa bleeds;
- Increased risk of internal bleeding;
- There is a risk of cerebral hemorrhage.
As soon as general symptoms appear, you should consult a doctor. Thrombocytopenia is treated in most cases on an outpatient basis.
Stenosis
If the pathology is severe, the patient must be placed in an intensive care unit. The treatment strategy itself is determined by the underlying disease.
Diagnostic measures
Any increased bleeding is a reason to visit a hematologist. The doctor will prescribe the necessary tests. Among which:
- General blood analysis;
- Hemostasiogram;
- Ultrasonography;
- Radiography;
- Enzyme immunoassay blood test.
The latest tests are indicated if necessary, this is already decided by the doctor.
Pathology in cancer
Thrombocytopenia is very common in cancer patients. This is not by chance, of course, chemotherapy and radiation therapy cause its appearance. Some drugs have a detrimental effect on platelets.
On the other hand, the pathology can be caused by some types of cancer, for example, lymphoma.
If a patient develops a pathology in which the platelet level drops, the doctor is obliged to consider all possible causes, even those not related to cancer treatment.
Thrombocytopenia makes the condition of an oncology patient complex, which means that the doctor faces difficulties in treating him. He must keep in mind that:
- If platelet counts are low, chemotherapy and radiation therapy must be carried out very carefully, as the risk of bleeding increases;
- A decrease in the rate of <50x109 per liter leads to an increased risk of heavy bleeding during surgery;
- A decrease <10x109 per liter significantly increases the risk of spontaneous bleeding.
Treatment of thrombocytopenia in cancer patients
There are recognized methods of treating pathology in cancer patients. They boil down to the following:
- It is necessary to adjust the therapeutic program;
- If necessary, transfuse platelet mass to the patient when there is a risk of bleeding or before a course of chemotherapy;
- It is necessary to transfuse platelet mass under the close supervision of a hemotransfusiologist and a nurse.
There are simple recommendations on how to avoid bleeding:
- Using an electric razor instead of a razor;
- Avoiding injury;
- Using a toothbrush with soft bristles;
- Rejection of drugs that reduce blood clotting, etc.
The Onco.Rehab Integrative Oncology Clinic is glad to see its patients who are not burdened by pathologies and their complications. We fight for your health, so that your days are filled with the joy of life.
Thrombocytopenic purpura and pregnancy
Author : Lidiya Olegovna Buzyan , physician-hemostasiologist at the Nova Clinic network of reproductive and genetics centers.
A little less than a hundred years ago, Moshkowitz first described an unusual disease in a sixteen-year-old girl with anemia, small hemorrhages on the skin, which ultimately ended in the development of paralysis and coma. This disease is named after him - thrombotic thrombocytopenic purpura (Moschkowitz disease) .
In recent decades, thanks to active study and search for effective treatment methods, this rather rare (in the USA 3.7 cases per 1 million people) disease is much less likely to lead to death in patients. After plasma therapy was used in treatment, patient mortality decreased from 80% to 10%. However, the outcome directly depends on how quickly the correct diagnosis is made and specific treatment is started. Unfortunately, due to the low specificity of symptoms and rare cases of the disease in the practice of most ordinary doctors, it is not always possible to quickly understand the situation.
Moschkowitz's disease affects vital organs - the brain and kidneys. The damage occurs due to thrombosis of the microvessels feeding these organs. And massive thrombus formation, as a consequence, leads to the fact that the supply of platelets and red blood cells in the blood is depleted - they are retained and accumulate in thrombotic masses; therefore, a general blood test will show a decrease in platelets and hemoglobin (anemia and thrombocytopenia).
The causes of the development of the disease consist of a combination of hereditary predisposition and a triggering provoking factor. Congenital genetic defects lead to a decrease in the activity of a specific enzyme - ADAMTS-13, as a result of which, when exposed to a certain trigger mechanism, thrombus formation in such people is activated to a much greater extent than in others, small vessels become clogged and symptoms of kidney or brain damage appear.
The following factors can provoke the development of thrombotic purpura:
- pregnancy (according to various sources, from 12% to 30% of all cases of the disease occur during pregnancy);
- infectious diseases (activation of blood clots can be caused by viruses, bacterial toxins - in particular, streptococcal toxin for pneumonia, Shigella toxin for intestinal infections in children);
- vaccination;
- taking certain medications (oral contraceptives, antitumor drugs, immunosuppressants after organ and tissue transplantation, the thinning drug clopidogrel);
- surgical interventions;
- the presence of autoimmune diseases (in particular, systemic lupus erythematosus, antiphospholipid syndrome).
During pregnancy, the manifestations of Moschkowitz's disease can easily be confused with preeclampsia or eclampsia. Blood pressure may increase, protein appears in the urine, there may be headaches, convulsions, even the development of coma (in severe cases and without treatment). Brain damage can also manifest as strokes or ischemic attacks. About three-quarters of cases occur in the third trimester. A significant decrease in platelets in a blood test (usually less than 100 and even less than 60) in combination with anemia (hemoglobin below 100 g/l, and in 40% of patients below 65 g/l) is a reason to suspect the presence of Moschkowitz disease and, if appropriate clinical symptoms, immediately carry out additional diagnostics. Since anemia in thrombocytopenic purpura is a consequence of the destruction of red blood cells, the concentration of indirect bilirubin and the enzyme LDH may be increased in the blood. The Coombs test helps in diagnosis, the result of which confirms or excludes the presence of hemolysis (destruction of red blood cells).
A specific and confirmatory diagnostic method is to determine the activity of the ADAMTS-13 enzyme in the blood, but this method is very limited in availability, as is the genetic determination of mutations in the ADAMTS-13 gene.
If the diagnosis is confirmed or most likely, treatment begins immediately. For thrombotic purpura, this is, first of all, plasmapheresis, and if it is impossible, a transfusion of fresh frozen plasma. Usually several procedures are required, since after completion of treatment the pathological process is soon activated again. In 30-60% of patients, relapses of the disease are observed, then to prevent them, plasma transfusion is repeated every 2-3 weeks.
The course of pregnancy and the possibility of maintaining it depend on the severity of the disease. Of course, in case of life-threatening conditions, it is necessary first of all to save the woman’s life; delivery in this case is almost inevitable. In this case, the child can be born quite viable. At the same time, even the appearance of symptoms of the disease at a short stage of pregnancy, provided there is a good response to therapy, is not an absolute indication for its interruption.
For a mild form of the disease, a transfusion of fresh frozen plasma is sufficient; for moderate and severe forms, plasmapheresis is required. If the affected kidneys cannot cope with filtering urine, hemodialysis is added. When blood pressure rises, antihypertensive drugs are used, and for severe anemia, red blood cell transfusions are used. It is also necessary to monitor the condition of the blood coagulation system; if necessary, thinning drugs can be prescribed. Delivery is performed only if there is no effect from all possible therapeutic measures. Also, after childbirth, it may be necessary to remove the spleen to prevent relapses.