Predisposing factors
In addition to the age factor, the appearance of atherosclerosis of the stenosing type is also influenced by:
- Hypertensive and ischemic diseases;
- Eating large amounts of fatty foods of animal origin;
- Presence of bad habits (alcohol addiction, smoking, unhealthy lifestyle, etc.);
- Frequent nervous overload, restless state.
Among these factors, bad habits are considered the most important. They provoke the development of atherosclerotic changes in blood vessels. The second predisposing factor is an unhealthy diet, which contains large amounts of cholesterol that is harmful to the body. Harmful cholesterol does not completely dissolve in the blood plasma; it leaves a sediment, which settles on the walls of blood vessels, forming atherosclerotic plaques.
The vessels of the lower extremities are most susceptible to atherosclerotic changes. Of course, other vascular systems also suffer from stenosing atherosclerosis, but it is the vessels of the lower extremities that are most susceptible to changes. This is explained by the fact that the arteries in the legs are lower than all the others, no matter how strange it all sounds.
Intoxication with alcohol and nicotine has the most detrimental effect on blood vessels. Nicotine contained in cigarettes can cause spasms in blood vessels. Alcohol has a bad effect on the human nervous system and causes an increase in cholesterol.
In addition, a person’s lifestyle and working conditions also influence. If a person leads a sedentary lifestyle and works in a warm, cozy office, then after 10 years of such a life, atherosclerosis is guaranteed in almost one hundred percent of cases. In order for the blood vessels to be in good shape, a person must walk at least 10 kilometers every day, and with such a lifestyle, this is almost impossible.
Also, local factors can influence atherosclerotic diseases of the lower extremities:
- Various injuries;
- Hypothermia;
- Impacts and damage to blood vessels.
Treatment methods
If you identify symptoms of the disease, you should first contact a therapist, who will refute or confirm the diagnosis and refer you to the right specialist.
For example, stenosing atherosclerosis of the MAG/vessels of the lower extremities is treated by an angiologist, atherosclerosis of the cerebral arteries, BCA - by a neurologist. To treat the disease, it is better to give preference to a conservative approach. It includes forming a strict diet and taking special medications aimed at inhibiting the destructive effects of the disease.
The essence of the therapeutic diet is to eliminate from the diet foods rich in cholesterol and animal fats (fast food, sweets, fatty meats, fatty dairy products, offal, etc.). But the amount of foods containing vitamin E and antioxidants, on the contrary, should be increased. The diet also includes eating plenty of fruits and vegetables (without any restrictions).
Attention! A good effect can be achieved by limiting salt intake, since this product tends to delay the removal of fluid from the body, which, in case of circulatory problems, can be fraught with a persistent increase in pressure (additional load on the walls of blood vessels).
If the diet does not give the desired results, over time you have to resort to a number of medications that can correct the lipid profile.
Drugs used for treatment:
- Inhibitors (Sinopril, Lisinopril). Absorb cholesterol, preventing its absorption into the blood.
- Statins (Atoris, Zator). They reduce the body's production of cholesterol and accelerate the removal of fats and similar substances from the body.
- Fibrates (Gemfibrozil, Tycolor). They increase the density of lipoproteins, whose task is to protect the walls of blood vessels from cholesterol.
- Sequestrants (cholestipol, cholestyramine). Effectively and quickly remove cholesterol from the body.
For the treatment of atherosclerosis of the main arteries of the head with stenosis, blood pressure stabilizers (qualitatively reduce the load on the vascular system) and anticoagulants (thin the blood, facilitating its movement even through stenotic arteries “clogged” with cholesterol plaques) are also prescribed.
Stenosing atherosclerosis of the brachiocephalic trunk and its branches
A method of treating stenosing atherosclerosis of the carotid arteries by straightening the stent.
Stenosing atherosclerosis of the brachiocephalic arteries occurs when the lumen of the brachiocephalic trunk is blocked by a plaque. To understand the principle of symptom development, you need to know the topographic location of the arteries. The brachiocephalic artery is the first to emerge from the aortic arch, is about 4 cm long, heads to the right and passes behind the sternoclavicular joint, where it divides into its terminal branches: The right common carotid artery. Right subclavian artery. The right vertebral artery, which is a branch of the subclavian artery.
Circulatory disorder of the upper limb
Atherosclerosis of the brachiocephalic vessels is accompanied by circulatory disorders in the right upper limb. The blood supply to the arm is designed in such a way that it is not deprived of collateral (bypass) circulation. The right subclavian artery is the main blood supply to the arm, but due to compensation with blood from other branches of the trunk, the process of ischemia develops slowly.
Initially, due to atherosclerosis of the brachiocephalic arteries, the arm becomes pale, sensitivity is impaired, paresthesia appears, then the pulse disappears on the right radial artery, hair disappears, the muscles of the forearm weaken, but the symptoms are transient and more often occur during physical activity. Further, stenosing atherosclerosis of the extracranial region is accompanied by the formation of trophic ulcers on the hands, necrosis of the fingers and the entire limb. When the right subclavian artery is damaged, fainting and dizziness, decreased vision, and headaches occur due to the symptom of cerebral steal, which occurs in response to ischemia of the upper limb.
Circulatory disorder in the vessels of the neck and head
Atherosclerosis of the main arteries of the neck occurs when the common carotid artery and its internal and external branches are damaged. Considering that with such localization of cholesterol plaques, the blood supply to the face and brain is disrupted, the symptoms will be appropriate. The sensitivity of the right half of the face disappears, and sensations of “crawling goosebumps” appear.
Atherosclerosis of the extracranial segments of the main arteries of the head and neck does not lead to severe cerebral complications; only transient ischemic attacks occur, accompanied by headache and dizziness. Due to the fact that blood circulation in the above segments is replenished by the left common carotid artery, which does not depend on stenotic atherosclerosis of the brachiocephalic vessels, acute brain failure does not occur.
The left sections, through the circle of Willis, partially compensate for hemodynamic disorders from the right half. A dangerous symptom is a progressive decrease in vision, which leads to blindness; this indicates a violation of circulatory compensation in the carotid artery system.
Circulatory disorders in the vertebral arteries
Atherosclerosis of the extracranial parts of the brachiocephalic arteries with stenosis also applies to vertebral vessels. This segment supplies blood to the posterior sections of the head and neck, while there is an intracranial section of these arteries, which has its own collateral path (Zakharchenko’s circle), which does not communicate with the system of the Circle of Willis.
Atherosclerosis of the main arteries of the brain from the vertebral segments is accompanied by coordination disorders, movements become uncoordinated (cerebellar ataxia), walking becomes uncertain, and the patient may fall out of the blue. When both vertebral vessels are completely closed, the patient begins to experience severe dysfunction of the cerebellum and occipital cortex; the patient will not be able to sit and may completely lose vision. The outcome of the disease will be an ischemic stroke of the occipital zone of the brain.
Cerebrovascular accident
Atherosclerosis of the main vessels of the brain from the internal carotid artery system is the most dangerous segment affected by cholesterol plaques. If the affected segment is located further than the circle of Willis, then when the vessel is obliterated by more than 70%, there is a high probability of ischemic stroke of the blood supply zone.
If blood circulation in the frontal lobe is impaired, which corresponds to the anterior cerebral artery, the patient loses the ability to make conscious movements, speech and emotional functions are disrupted, cognitive abilities completely disappear, and pathological reflexes appear.
If the blood circulation in the parietal lobe, which corresponds to the middle cerebral artery, is impaired, the patient does not perceive the projection of his body, confuses the right and left sides, is unable to recognize and describe objects, and completely loses deep and superficial sensitivity.
If the blood circulation of the temporal lobe from the middle cerebral artery is disrupted, the patient loses the ability to hear and distinguish sounds.
Atherosclerotic lesion of heart vessels
Stenosing atherosclerosis of the coronary arteries is accompanied by attacks of angina pectoris, and there is a high risk of myocardial infarction. Localization of atherosclerotic plaques in the own arteries of the heart is dangerous, since the diameter of their lumen is small and complete occlusion of the vessel develops quickly.
In recent years, interest in the problem of cerebral circulatory disorders caused by atherosclerosis with predominant damage to intracranial arteries has increased significantly. On the one hand, this is due to epidemiological factors: the high prevalence of both clinically asymptomatic atherosclerosis of intracranial arteries and repeated ischemic cerebrovascular accidents (ICDs) developing as a result of intracranial atherosclerosis (IA). On the other hand, the detection of IA has improved significantly in recent years due to the intensive development of neuroimaging techniques.
Intracranial atherosclerosis can be asymptomatic and lead to the development of both acute cerebrovascular accidents and chronic forms of cerebral vascular disease (atherosclerotic angioencephalopathy). Considering the epidemiology of IA, we should dwell separately on the so-called. asymptomatic intracranial atherosclerosis, which is understood as atherosclerotic lesions of intracranial arteries identified by neuroimaging in patients without anamnestic indications of transient ischemic attack (TIA) or ischemic stroke (IS). According to JF Arenillas (2014), the frequency of “asymptomatic intracranial atherosclerosis” ranges from 5.9 to 24.5% in people at high risk of stroke [1]. At the same time, international experts emphasize the significantly more frequent detection of IA in people of Asian origin: the frequency of “asymptomatic intracranial atherosclerosis” in representatives of the Asian race reaches 54%, several times higher than that in representatives of other races [2–4].
Among the specified causes of ischemic cerebrovascular accidents, IA remains one of the most common causes worldwide [5]. Moreover, as with “asymptomatic intracranial atherosclerosis,” the frequency of TIA and IS caused by atherosclerotic lesions of intracranial arteries is significantly higher in patients of the Asian race, reaching 50%; among representatives of the Caucasian and Negroid races, this figure is estimated at 10 and 30%, respectively [3, 5–10].
According to researchers, this is due to both a genetic predisposition to developing the disease in different ethnic groups, as well as differences in lifestyle and typical risk factors [3].
The significance of atherosclerotic lesions of intracranial arteries is also determined by the high frequency of recurrent TIAs and strokes, which are 11 and 13%, respectively, in patients undergoing therapy with oral anticoagulants one and two years after suffering a stroke, and 12 and 15%, respectively, in patients undergoing therapy with platelet antiplatelet agents [11] . Moreover, in patients with middle cerebral artery (MCA) stenosis of more than 70%, the annual incidence of stroke during antithrombotic therapy increases to 18% per year [12]. According to other data, the frequency of recurrent IS in patients who had MCA stenosis of more than 70% and were on antiplatelet therapy was even higher - it was 23.7% at the end of follow-up for 56 months. In patients with stenosis of the intracranial internal carotid artery (ICA), this figure reached 36.1% [12].
The likelihood of clinical symptoms in patients with “asymptomatic intracranial atherosclerosis” is determined by a number of factors, the most important of which are the location and degree of stenosis, as well as the structural features of collateral vessels [14]. Thus, for atherosclerotic changes in the anterior cerebral (ACA) and posterior cerebral (PCA) arteries, an asymptomatic course is characteristic in a greater number of cases than for lesions of the MCA, the intracranial part of the ICA and the vertebral artery, as well as the basilar artery [8]. At the same time, it is atherosclerotic lesions of the MCA and the intracranial part of the ICA that are more frequent [15], atherosclerotic changes in the basilar artery and the intracranial part of the vertebral artery are diagnosed less frequently, and even less often in the arteries of the convexital surface of the brain - the ACA and PCA [16].
The most serious clinical manifestations of IA include acute cerebrovascular accidents, the symptoms of which correspond to the location of the atherosclerotic lesion of the intracranial artery and the extent of brain damage.
There are three mechanisms for the development of cerebral infarctions in patients with intracranial atherosclerosis [17]:
- hypoperfusion of the brain with the development of infarction in areas of adjacent blood supply associated with decompensation of autoregulation processes
- cerebral blood flow (especially in conditions of impaired systemic hemodynamics);
- arterio-arterial embolism;
- atherostenosis at the mouth of perforating arteries, causing the development of small infarctions.
In this case, MCA stenosis, as a rule, leads to the development of small deep infarctions or infarctions in the area of adjacent blood supply; stenosis of the intracranial ICA is accompanied by the development of large or extensive lesions involving the gray matter, which is reflected in more severe neurological symptoms compared to infarctions due to MCA stenosis [18].
The course of IA can be stable or progressive [19]. At the same time, in patients with clinically symptomatic IA, progression of atherosclerosis (i.e., an increase in the degree of stenosis of intracranial arteries), according to B. Joon Kim (2014), was observed significantly more often than in patients with “asymptomatic” IA [20]. The chronic course of IA underlies the formation of atherosclerotic angioencephalopathy, characterized by both specific pathomorphological features (a complex of diffuse and focal changes in the brain of an ischemic nature, of varying localization, severity and duration [17]), and the formation of a clinical syndrome complex (cognitive impairment, extrapyramidal and pyramidal symptoms , vestibulo-cerebellar syndrome, etc.).
The “gold” standard for diagnosing IA is digital subtraction angiography [21]. On the one hand, this method makes it possible to most accurately determine the degree of stenosis of the intracranial artery (which is a key prognostic factor for IA); on the other hand, it is invasive and involves the introduction of a contrast agent, which is associated with a certain percentage of complications, incl. the appearance of persistent or transient neurological symptoms in 0.6 and 1.8% of cases, respectively [22]. Non-invasive methods for diagnosing IA include transcranial Doppler ultrasound, magnetic resonance imaging (MRA) and computed tomography (CTA) angiography. There is no clear evidence regarding the accuracy of diagnosing IA using these safer and more accessible non-invasive methods. Thus, transcranial Doppler sonography is largely an operator-dependent technique; its implementation in some cases is impossible due to the lack of the so-called. ultrasound window, while the undoubted advantage of this method is the ability to determine the direction of blood flow, as well as assess collateral blood flow. Due to the physical basis of the method, visualization of intracranial artery stenosis with MRA depends on blood flow, which can lead to a distortion of the severity of the stenosis (for example, critical MCA stenosis with very low blood flow may appear as an occlusion with MRA). In general, it is believed that transcranial Doppler ultrasonography and MRA can be used as screening techniques to exclude IA lesions, but they are not reliable enough to confirm the presence of stenosis and determine its severity [23]. Computed tomographic angiography is superior to MRA in diagnostic accuracy [24, 25] and has the highest sensitivity and specificity for detecting stenosis after digital subtraction angiography, more than 50% [26]. However, this diagnostic method involves the introduction of a contrast agent and additional radiation exposure.
In recent years, CT and MRI perfusion techniques have been increasingly used, making it possible to supplement data on the stenosis of a particular intracranial artery by identifying areas of hypoperfusion. In addition, in addition to the “classical” IA visualization techniques, new technologies can be used that allow not only to judge the degree of stenosis, but also to obtain an idea of the structure of the atherosclerotic plaque. Thus, high-resolution MRI makes it possible to directly visualize a thrombus, hemorrhage into a plaque and determine the composition of the plaque; intravascular ultrasound also makes it possible to detect hemorrhage in the plaque, determine its composition and extent [21, 27]. Taking into account the complexity and high cost of the diagnostic methods described above, a more detailed angioneuroimaging examination may be recommended for patients who have suffered IS or TIA, the genesis of which remains unclear after conducting a complex of instrumental and laboratory examinations and excluding pathology of extracranial arteries (hemodynamically significant stenosis, dissection, etc.), hypertensive small deep (lacunar) infarction, cardiac pathology (atrial fibrillation, post-infarction cardiosclerosis, etc.), coagulopathy.
The main goal of treatment for patients with symptomatic IA is to prevent recurrent cerebrovascular accidents. Measures aimed at this include blood pressure (BP) control, because systolic blood pressure ≥140 mm Hg. significantly increases the risk of stroke in the corresponding arterial basin [28, 29], elimination of dyslipidemia (with achievement of target values of total cholesterol ≤5.1 mmol/l and low-density lipoproteins ≤1.8 mmol/l) [29], “aggressive” correction other risk factors (normalization of body weight, increased physical activity, smoking cessation, maintenance of normoglycemia) in accordance with recommendations for secondary prevention of stroke [30, 31] and antithrombotic therapy.
The WASID international controlled randomized trial compared the effectiveness and safety of prophylactic use of monotherapy with antiplatelet agents (acetylsalicylic acid [ASA] at a dose of 1300 mg per day) and oral anticoagulants (warfarin maintaining an international normalized ratio of 2–3). The study included more than 500 patients with IS or TIA that developed against the background of stenosis of 50 to 99% of the large intracranial arteries (MCA, intracranial ICA, vertebral artery and basilar artery). Despite the absence of differences in the effectiveness between the groups of antiplatelet and anticoagulant therapy upon achieving the primary endpoint (combined endpoint: assessment of the incidence of ischemic, hemorrhagic stroke, vascular death), the frequency of recurrent IS after one and two years, warfarin therapy was associated with higher the percentage of hemorrhagic complications and deaths, and therefore the WASID study was terminated early [11].
A subsequent WASID subgroup analysis did not demonstrate a benefit of warfarin over ASA in patients with subtotal intracranial artery stenosis, women, or patients who developed IS or TIA on prior ASA therapy [32].
Thus, the main finding of the WASID study was the preference for ASA monotherapy (over warfarin) in patients with symptomatic IA. Nevertheless, taking into account the rather high percentage of repeated ischemic events during ASA monotherapy, further studies were conducted to evaluate the effectiveness and safety of combination antiplatelet therapy for IA. Thus, SU Kwon et al. (2005) demonstrated the advantage of combined antiplatelet therapy (cilostazol 200 mg per day and ASA) over ASA monotherapy (100 mg per day): after 6 months of observation of patients with symptomatic stenosis of the MCA or basilar artery, a lower rate of progression of atherosclerosis was revealed according to MRA [33 ]. In a study by SU Kwon et al. (2011), conducted on 457 patients with symptomatic stenosis of the MCA or basilar artery, comparing the effectiveness and safety of various combination antiplatelet therapy options: cilostazol 200 mg per day + ASA 75–150 mg per day and clopidogrel 75 mg per day + ASA 75– 150 mg per day showed no differences between groups in the rate of progression of stenosis on MRA after 7 months, the incidence of cardiovascular events, the appearance of new ischemic lesions on MRI and the development of hemorrhagic complications [34].
In a small (70 patients) open-label multicenter study (2013) of patients who, 7 days before inclusion, suffered an IS or TIA due to an IA, in whom transcranial Doppler ultrasound revealed microembolic signals (MES), X. Wang et al. a lower incidence of MES was demonstrated during seven-day combination antiplatelet therapy (clopidogrel 75 mg per day + ASA 100 mg per day) compared with ASA monotherapy [35].
For many years, attempts have been made to surgically treat atherosclerotic stenosis of intracranial arteries and its consequences. The earliest and most studied operation was the application of extra-intracranial anastomosis, however, according to the results of studies conducted in the 1980s [13] and in 2011 [36], its effectiveness was not proven and at present this operation is not widespread.
Modern methods of surgical treatment of IA include endovascular interventions using balloon angioplasty, balloon angioplasty with stenting and installation of self-expanding stents. The latter are characterized by a high rate of technical success and relative ease of installation, because do not require the use of a balloon and can be delivered to difficult-to-pass areas of the arterial bed. The international randomized controlled trial SAMMPRIS [37] was devoted to comparing the effectiveness and safety of endovascular and conservative treatment of IA. The study included patients who, 30 days before randomization, suffered an IS or TIA against the background of an IA with the formation of a stenosis of 70–99%. As a so-called aggressive conservative therapy, patients were prescribed combination antiplatelet therapy (clopidogrel 75 mg per day and ASA 325 mg per day), antihypertensive therapy with maintaining systolic blood pressure below 140 mm Hg. (in patients with diabetes mellitus below 130 mm Hg), lipid-lowering therapy with target low-density lipoprotein levels below 70 mg/dl, and strict control of other vascular risk factors (with lifestyle modification). In the endovascular treatment group, the above conservative therapy was supplemented by angioplasty with stenting (Wingspan stent). The study was stopped early at the stage of inclusion of 451 patients due to the lack of evidence of effectiveness and worse safety indicators of stenting: for example, the rate of recurrent stroke within 30 days in the endovascular treatment group reached 14.7% (in a third of cases - intracerebral hemorrhages) compared with 5.8% in the conservative therapy group (p = 0.002), and the incidence of deaths in the surgical and conservative treatment groups was 2.2 and 0.4%, respectively [37, 38]. Despite the fact that among all patients included in the SAMMPRIS study, 63% of IS or TIA developed during previous antiplatelet therapy, in a subgroup analysis of this sample of patients, the effectiveness (rate of recurrent strokes) and safety (percentage of deaths) were also worse when stenting intracranial arteries than when prescribing aggressive conservative therapy [39].
Summarizing the above evidence-based medicine data regarding secondary prevention of stroke in IA, the following key points should be noted:
For patients who have had an IS or TIA due to an IA with the formation of a stenosis of 50–99%, antiplatelet therapy (ASA drugs) has advantages over warfarin therapy (primarily in terms of safety) (Class I; level of evidence B in accordance with AHA-ASA recommendations, 2014 [31]).
For patients with more severe stenotic lesions of intracranial arteries (70–99%) during the first 30 days after IS or TIA, the addition of clopidogrel (75 mg per day) to ASA therapy (325 mg per day) for up to 90 days is justified (class IIb ; level of evidence B according to AHA-ASA recommendations, 2014 [31]). In the future, it is advisable to stop taking clopidogrel (in the absence of other indications for its use) and switch to ASA monotherapy (at a dose of 325 mg per day), since, on the one hand, there is no evidence of the effectiveness of clopidogrel monotherapy as a means of secondary prevention of IS or TIA in patients with IA, on the other hand, longer treatment with two antiplatelet drugs is not justified due to the increased risk of hemorrhagic complications.
For patients with moderate stenosis (50–70%) of a large intracranial artery or patients after IS or TIA more than 30 days old (regardless of the degree of stenosis), ASA monotherapy at a dose of 325 mg per day in combination with intensive correction of risk factors is advisable.
Equally important is maintaining systolic blood pressure below 140 mmHg. and “aggressive” statin therapy (Class I; Level of Evidence B according to 2014 AHA-ASA guidelines [31]).
The effectiveness and safety of a combination of adequate antiplatelet, antihypertensive and lipid-lowering therapy in combination with lifestyle modification and careful monitoring of vascular risk factors is significantly higher than with balloon angioplasty with stenting of intracranial arteries (class IIb; level of evidence C in accordance with AHA-ASA recommendations, 2014 [31]).
As mentioned above, the progressive course of IA underlies the development of atherosclerotic angioencephalopathy. In relation to this category of patients, along with the described approaches to the prevention of ischemic stroke, the prescription of pathogenetically based drugs that improve the quality of life remains equally important. Since the development of IA is accompanied by impaired autoregulation of cerebral blood flow and the formation of hypoperfusion zones, it is advisable for such patients to use drugs that have neurotrophic, metabolic and antihypoxic effects.
A number of foreign randomized placebo-controlled studies have shown the effectiveness of Actovegin for elderly patients with signs of mild to moderate vascular dementia [40]. The extensive experience of Russian researchers confirms the effectiveness of the drug for patients with chronic cerebral ischemia, accompanied by cognitive disorders, manifested both in a positive effect on memory and attention (according to a neuropsychological examination), and in improving the psycho-emotional status of patients (decreasing the severity of depressive and asthenic symptoms, improved sleep and general well-being) [41–44]. The proven endothelial protective effect of Actovegin and the positive effect on microcirculation likely provide additional therapeutic benefits to patients with cognitive disorders resulting from chronic cerebral ischemia. Thus, the inclusion of Actovegin in the treatment regimen for patients with IA, along with measures to prevent vascular events, can help level out the manifestations of cerebral circulatory failure and improve the well-being of such patients.
So, IA makes a significant contribution to the development of acute and chronic cerebrovascular accidents and requires a special approach to diagnosis and prescription of personalized therapy. Further progress in the study of this problem will largely be based on the development of new methods of neuro- and angiovisualization, the accumulation of an evidence base on drugs for the secondary prevention of IS, as well as the search and justification for the prescription of other (therapeutic and surgical) approaches to the treatment of NMC.
Vascular stenosis of the lower extremities
Stenosing atherosclerosis of the arteries of the lower extremities has symptoms similar to those in the upper extremities. In the first stages, a disorder of sensitivity and temperature of the extremities occurs. Then a pathognomic symptom appears for plaques localized on the vessels of the lower extremities, which is intermittent claudication, which is manifested by aching pain in the legs that appears while walking and disappears when stopping and resting. In advanced forms of the disease, fascial swelling of the muscles occurs, which develops into trophic disorders of the limbs, which threatens amputation.
Preventive measures
To prevent the development of the disease and the manifestation of its complications, it is necessary to strictly follow the doctor’s instructions. The following tips should be followed to prevent illness:
- Strict control over blood pressure.
- Carrying out regular (moderate) physical activity (fitness, yoga, swimming, running, walking in the fresh air, etc.).
- Refusal of bad habits (if any are present in life).
- A balanced, healthy diet rich in antioxidants and vitamins.
- Regular preventive examinations by a specialist.
How effective is treatment of the disease with folk remedies (herbs), read here; and how to deal with the disease - follow the link.
Clinical manifestations of stenosing cerebral atherosclerosis
The presence of an atherosclerotic process in the body can be recognized by the following clinical symptoms:
- Painful sensations in different parts of the body. They appear at the first stage and indicate tissue ischemia. Patients begin to experience pain in their legs, head and neck.
- Paresthesia. This is the feeling of goosebumps crawling on the skin. A similar phenomenon occurs when small vessels that feed sensitive skin cells are blocked.
- Flashing of flies before the eyes. It appears when the atherosclerotic process has reached the choroid plexuses of the retina.
- Ringing in the ears and dizziness. Similar symptoms debut when cholesterol plaques appear in the arteries and veins of the head, reaching the vestibular apparatus.
- Ulceration of the skin of the lower extremities. Similar symptoms occur when the disease reaches the second, thromonecrotic stage. Thrombosis appears in the vascular beds of the legs with necrosis of tissue areas in which there is no oxygenation.
- Blueness of the nasolabial triangle and distal parts of the body. This symptom occurs as a result of sequential fibrosis and sclerosis of blood vessels affecting different organs. The blood is simply unable to reach distant areas, which consequently become cyanotic.
Stenosing atherosclerosis MAG - what is it?
Stenotic atherosclerosis is a pathology of blood vessels. Fatty deposits, called cholesterol plaques, form on the inner walls of these vessels.
What is important is that the disease is not sudden. Its development occurs over a long period of time, with the slow formation of plaques.
There is a process with the formation of calcifications and the gradual proliferation of connective tissues. The mechanism of occurrence and spread of the disease in the body comes down to the accumulation of low-density fats in the blood. Over time, they stick to the slightest irregularities inside the vessels and form plaques, which, as the disease progresses, lead to blockage of the arteries. As a result, the clearance for blood flow decreases to such an extent that the blood supply is completely disrupted, leading to ischemia of organs and tissues.
Diagnostics
Stenosing atherosclerosis of the coronary arteries, carotid vessels and other vascular structures is diagnosed using the following physical and instrumental techniques:
- To determine the presence of the disease, auscultation is used, which helps to hear the blood flow.
- Auscultation. It helps to listen to the characteristic noise of turbulent blood flow using a stethoscope.
- Visual inspection. Patients with the described lesions often experience contouring and pulsation of blood vessels in those areas of the body where the latter lie directly under the skin.
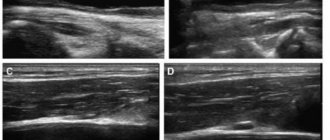
- Dopplerography. Most accurately determines stenosing atherosclerosis. This significant method makes it possible to identify such echo signs as occlusion by a thrombus, plaque or embolus, swirling of blood in stenotic areas, and a decrease in the speed of its flow through the main arteries.
- Angiography of blood vessels using a contrast agent. This is an x-ray method that allows you to determine the location and degree of narrowing.
Diagnosis of the disease
A number of medical devices and procedures are used to diagnose the disease:
- Initially, the doctor collects an anamnesis of the disease, asks the patient about his lifestyle and habits, and then begins a visual examination.
- After receiving the initial data, the patient must undergo a series of tests (general, biochemical and immunological blood tests, urine analysis - to identify a possible inflammatory focus).
- The specialist does an ECG and ultrasound of the heart, MRI.
Important! Ultrasound signs are considered the most accurate confirmation of an unpleasant diagnosis. The Doppler picture is based on signals from an ultrasound machine, which are received during the procedure by reflection from blood elements. - If a questionable result is obtained, the doctor additionally prescribes angiography to determine the level of blood flow in the vessels.
- Echocardiography makes it possible to determine the presence of damage to the heart vessels, and stress echocardiography allows not only to detect the presence of significant atherosclerosis, but also to determine its location.
- If necessary, the doctor consults with other specialists depending on the area affected by stenosing atherosclerosis.
Features of therapy
Treatment can be prescribed after a comprehensive diagnosis and identification of the degree of vasoconstriction. Therapy, depending on the degree of neglect of the pathological process, can be carried out using both conservative and surgical methods.
Medications
In the initial stages of the disease, the use of certain medications can suppress it. Statins are prescribed to reduce the concentration of cholesterol in the blood. In addition, patients are prescribed inhibitors and sequestrants, which contribute to impaired absorption of fats in the intestine and rapid elimination of lipids. To increase the tone of the vascular walls, fibrates are prescribed. A prerequisite for recovery is adherence to a special diet. Physiotherapeutic procedures may be additionally prescribed.
Surgery
Surgical treatment methods are used to treat late stages of the disease, when there is almost no blood flow to the affected area. The most commonly used techniques are: bypass surgery; stenting; balloon angioplasty. In particularly severe cases, open surgical interventions are performed, involving the formation of vein anastomoses and the replacement of damaged areas with prostheses.
Typical signs and symptoms
The symptoms of diseases of the brachiocephalic arteries are specific. If you feel alarming symptoms, but your doctor, after listening to the complaints, limited himself to pointless diagnoses (CFS, VSD, etc.), be sure to insist on an expanded diagnosis.
Symptoms of diseases of the brachiocephalic arteries include:
- General fatigue, weakness, decreased performance and concentration;
- Sharp headaches that occur when moving the head;
- Dizziness and syncope (short-term loss of consciousness);
- Fainting with low blood pressure;
- Noise or ringing in the ears;
- Transient paresis of the head and limbs;
- Visual disturbances (appearance of spots and flies in the field of vision, decrease in visual acuity with sudden recovery);
- Angina pectoris;
- Ischemia (sometimes asymptomatic);
- Itching, numbness, tingling in the left extremities;
- Swaying when walking;
- Nausea;
- Rare or frequent disorders of motor or speech functions (numbness, inability to communicate clearly).
The insidiousness of atherosclerosis of the brachiocephalic arteries lies in its “blurred” early course. The listed signs sometimes do not make themselves felt at all, or are expressed so weakly that the patient does not attach due importance to them. Ignoring diagnosis and treatment leads to death or a vegetative state.
Why is it dangerous?
Stenosis itself is a violation of the anatomical and physiological norm of the structure of organs. Wherever it appears, it always entails increased ischemia of the surrounding tissues. Stenosing cerebral atherosclerosis is dangerous for the development of acute cerebrovascular accident. Stenotic defect of the coronary arteries leads to the onset of myocardial infarction. Atherosclerotic process in the vascular bed often causes rupture of the coronary artery or aortic aneurysm. If it is activated in the peripheral arteries and veins, it ends in gangrene of the upper or lower extremities. Vivid clinical signs of stenosing atherosclerosis indicate the possible occurrence of imminent death
Consequences and complications
Late detection of the disease and lack of proper treatment can lead to irreversible and very serious consequences. For example, damage to the carotid arteries can provoke a stroke, and severe blockage of the main arteries of the head can lead to massive hemorrhages. There are a number of complications provoked by the rapid progression of the disease:
Spicy. The development of the disease can lead to serious disorders of cerebral and cardiac circulation (aortic aneurysm, gangrene, ischemia of the heart muscle, etc.).- Chronic. Insufficient blood circulation in the diseased parts of the body leads over time to functional and then organic (unfortunately, irreversible) changes. So, if atherosclerosis of the BCA was detected untimely or treatment was not prescribed on time, the patient will eventually develop a neurological disorder in the brain. Dementia often develops on this basis.