Quick transition Treatment of gastritis
Gastritis is a general term that combines several pathological conditions characterized by inflammation and degeneration of the gastric mucosa.
The mucous membrane covers the entire surface of the stomach and plays an important role in digestion. Its glands produce gastric juice, the enzyme pepsin, hydrochloric acid, lipase, hormone-like components, mucus and bicarbonate. These substances are responsible for the breakdown of proteins and fats, protect the body from pathogenic bacteria, and activate metabolic processes.
When inflamed, the mucous membrane produces less acid, enzymes, mucus and other substances that are necessary for the proper functioning of the gastrointestinal tract. There is a risk of developing gastritis.
Gastritis can occur in acute and chronic forms. It is important to see a doctor in time to get a diagnosis and treatment, and to prevent complications.
Forms and complications of gastritis
In the absence of adequate and timely treatment, gastritis can cause complications. These include:
- Stomach ulcer. Peptic ulcers affecting the mucous membrane of the stomach or duodenum. Peptic ulcer disease is provoked by excessive use of painkillers (NSAIDs), and gastritis caused by H. pylori. It is difficult to say where gastritis ends, especially with erosions, and peptic ulcer disease begins. Apparently these are different forms of the same process.
- Atrophy of the gastric mucosa - atrophic gastritis. It occurs due to thinning of the mucous membrane, the formation of fibrosis (microscars) of the membrane during chronic gastritis. With atrophy, the number of active cells in the gastric mucosa that produce enzymes and acid decreases. The absorption of some vitamins is impaired. Atrophic gastritis is a risk factor for oncological transformation and therefore requires special attention.
- Gastric bleeding with erosive gastritis and ulcers. It is characterized by shortness of breath, weakness, dizziness, blood in the vomit and stool, black stools, and pale skin. If these symptoms occur, you should immediately seek medical help.
- Anemia. Most often it occurs due to acute (as described above) or chronic blood loss, for example, with multiple repeated erosions of the stomach. Research suggests that H. pylori-associated gastritis and autoimmune gastritis can affect the body's absorption of iron and vitamin B12 from food, which can also cause anemia.
- Vitamin B12 deficiency and pernicious anemia (pernicious anemia). Autoimmune gastritis does not produce a certain protein that helps absorb vitamin B12, which is necessary for the production of red blood cells and nerve cells. Insufficient absorption of vitamin B12 can lead to the development of pernicious anemia. The same changes occur in the advanced stage of atrophic gastritis of any origin.
- Stomach cancer. Chronic gastritis increases the likelihood of developing benign or malignant neoplasms in the gastric mucosa. For example, gastritis associated with H. pylory increases the risk of adenocarcinoma and lymphoma of the gastric mucosa.
Why are gastroprotectors needed?
To prevent complications such as peptic ulcers and malignant tumors, it is important to keep the structure of the mucous membrane intact. Gastroprotectors are used for these purposes:
They should be taken when signs of gastritis appear. The doctor will determine which medications will fit into the selected treatment package. For prevention purposes, you do not need to drink them.
The stomach contains natural gastroprotectors - prostaglandins. They stimulate the formation of mucus, improve microcirculation and protect cells from destruction. If they are not produced enough, the gastroenterologist may prescribe their synthetic analogues. If the patient is being treated with non-steroidal anti-inflammatory drugs, drugs with prostaglandins prevent ulcerative lesions of the mucous membrane.
Causes and risk factors of gastritis
- Bacterial infection Helicobacter pylori. It is one of the most common types of infections and is transmitted through the fecal-oral route, for example through contaminated food and water. For the development of gastritis, the presence of Helicobacter pylori infection alone is not enough. It is believed that vulnerability to the bacterium is inherited or occurs due to an unhealthy lifestyle (smoking, poor diet), medications.
- Painkillers (non-steroidal anti-inflammatory drugs, NSAIDs). Regular and excessive use of aspirin, ibuprofen or naproxen can cause both acute and chronic gastritis, their toxic effects reduce the production of the main protectors of the gastric mucosa. To distinguish this situation from other types of gastritis, it is called NSAID gastropathy.
- Alcohol. Irritates and gradually destroys the gastric mucosa, exposing it to the aggressive effects of gastric juice. Alcohol most often provokes acute gastritis.
- Age. Older people are at increased risk of developing gastritis because the lining of the stomach thins with age. Older people are also most vulnerable to infections (H. pylori) or autoimmune disorders.
- Stress. Severe stress associated with injuries, burns, severe operations and infections can trigger acute gastritis.
- Exposure to radiation or radiation therapy (due to another medical condition).
- Bile reflux after gastric resection.
- Allergies to foods such as cow's milk and soy (especially in children).
- Autoimmune diseases. As a result of autoimmune processes, the body produces antibodies that attack the cells that form the gastric mucosa. Autoimmune inflammation occurs, and the functions of the protective barrier of the mucous membrane decrease. Gastritis associated with autoimmune disorders is called autoimmune gastritis. It is more common in people with other autoimmune disorders, including Hashimoto's disease and type 1 diabetes. Autoimmune gastritis may also be associated with vitamin B12 deficiency.
- Other diseases. The risk of gastritis may be increased by other medical conditions, including Crohn's disease, sarcoidosis, parasitic infections, and HIV/AIDS.
Syphilis of the oral mucosa
Syphilis of the oral mucosa is a manifestation of a general chronic disease that affects the entire body. In principle, all doctors, both general practitioners and dentists, know: the idea that syphilis can only manifest itself on the genitals is a misconception.
Etiology of syphilis
The etiology of syphilis is associated with a bacteria called Treponema pallidum. The route of infection is sexual, but it can also occur oral. In general, in order for the disease to develop, it is only necessary for Treponema pallidum to penetrate through the damaged mucous membrane or skin. Cases of penetration through intact skin and mucous membranes have been recorded. Syphilis is quite common; about 40% of children have manifestations of primary syphilis in the oral cavity. Secondary recurrent syphilis is less common, occurring in about 10% of cases in adolescents.
Syphilis in the 21st century is a medical and social problem.
Clinical picture of syphilis
The clinical picture of syphilis primarily depends and differs, of course, from the period of syphilis. There are 3 periods in the development of syphilis. Each period has its own characteristics in the manifestation and treatment of the disease. It must be remembered that congenital syphilis is also included in a separate group of syphilitic diseases.
For the clinical picture of syphilis to develop, it is necessary for about 3 to 4 weeks to pass, which is the incubation period of syphilis. But it is possible to shorten it to 1 - 1.5 weeks, or lengthen it to six months.
So.
Clinical picture of syphilis - First period of syphilis
The clinical picture of the primary period of syphilis is associated with the appearance at the site where treponema has invaded, the appearance of hard chancre - primary syphiloma.
Primary syphiloma will be clinically noticeable within 1.5 - 2 months, that is, about 6 - 8 weeks. What does chancre look like? In principle, a hard chakra can be either in the form of an ulcer or in the form of erosion. Often oval or round in shape, may be saucer-shaped. The edges are always smooth and crisp. Syphilitic chancre is always at the same level with the mucous membrane of the oral cavity.
In rare cases, the edges of the ulcer may be raised. The bottom of the chancre is smooth, shiny, bright red. The literature specifies that the bottom may be “greasy”, that is, slightly colored with a dull white coating. The main sign by which a tuberculous ulcer can be distinguished from a chancre is complete painlessness on palpation of a chancre. There have been cases when the size of the chancre was almost equal to the area of the entire mucous membrane of the hard and soft palate, but it did not cause any subjective sensations in the patient. Also, in the presence of hard chancre, there are no acute inflammatory processes in the surrounding mucous membrane.
Chancre is painless upon palpation, we have sorted this out, but in its consistency it is dense and “cartilage-like”.
This means the patient walks like this for 3 or 4 days. Then a week passes. And nothing seems to bother him: “Well, there’s something red in the mouth, but it doesn’t hurt.” So after a week, maximum 10 days, the lymph nodes are involved in the process. Lymph nodes in the primary period of syphilis increase in size, are dense, elastic, and painless on palpation. The lymph nodes do not merge with the skin, and the color of the skin does not change.
In addition, primary syphilis can manifest itself not only in the form of erosion or ulcers, but can also be a regular abrasion. The favorite places when primary syphilis appears in the form of an abrasion are the corners of the mouth - identical to jams, only unlike them, the abrasion will be dense at the base. On the transitional fold - elongated, on the tongue - this is the middle third, one abrasion, maximum two. If primary syphilis appears on the gums, then it will be an ulcer, bright red in color, its length corresponding to the width of 1 - 2 teeth.
Very rare cases of manifestation of primary syphilis on the tonsil. However! Primary syphilis on the tonsil is characterized by its unilateral enlargement, painlessness, with the presence of purulent plugs.
With primary syphiloma, hard chancres can be located close to each other and merge, forming a herpetiform chancre. This manifestation of primary syphilis is the most rare of all the manifestations in the oral cavity that have previously occurred.
To summarize, this is what you should remember: primary syphilis occurs 6-8 weeks after infection. Its first manifestation is chancre (here you need to read the description of chancre again), which can be located on the mucous membrane of the cheeks, palate, lips, transitional fold, tongue, and in rare cases on the tonsil. Lymph nodes enlarge a week after the onset of chancroid. The diagnosis will be established only after identifying chancre in the punctate and lymph nodes - treponema pallidum. Serological reactions are positive 4-5 weeks after infection.
Clinical picture of syphilis - Secondary period of syphilis
The secondary period of syphilis is characterized by a long course, namely from 3 to 5 years. The secondary period of syphilis will begin 1.5 - 2 months after the appearance of chancre. An important difference between the secondary period of syphilis and the primary period is not only the elements of the lesion, but also the peculiarity of the course. Since the secondary period of syphilis occurs in waves. What this means is that in the second period of syphilis there is both an active period, when there are elements of the lesion, and a latent period, when there are no elements visible to the eye.
During the active secondary period of syphilis, the clinical picture will be characterized by the presence of elements such as roseola, papules, pustules - secondary syphilides. These are elements that occur both on the skin and on the mucous membrane. The outlines of the elements in the secondary period of syphilis are rounded, smooth, the boundaries are clear and sharp. The color ranges from bright pink to scarlet and red. These elements do not have the ability to merge with each other. Secondary syphilides pass quickly, do not cause itching, and do not leave scars.
Secondary syphilides can occur in addition to the skin and mucous membranes of the lips and cheeks on the tongue, soft palate and tonsils. The main feature of the occurrence of secondary syphilides in these places is their constant tendency to merge, forming large lesions. The mucous membrane in these places is hyperemic, swollen, and pain may occur when swallowing.
However, the most common lesions on the mucous membrane are papules. Papules in secondary syphilis are round, dense, painless on palpation, surrounded by a halo of hyperemia. The size of papules can vary from 3 – 10 mm. Localization varies.
Papules can appear on the tongue; there are some peculiarities here:
- With atrophy of the filiform papillae, smooth, shiny, oval-shaped surfaces may form just below the level of the mucosa. This clinical picture is called “Mowed meadow”
- Papules on the tongue can increase in size, that is, hypertrophy, change in color, and become pale red. This type of secondary syphilis on the tongue is called hypertrophied papules;
- “Opal papules on the tongue” - trauma to the papules occurs, the surface becomes wrinkled, the papules will be loose, pale with a whitish tint.
Clinical picture of syphilis - Tertiary period of syphilis
The clinical picture of the tertiary period of syphilis is the most complex, characterized by the appearance of syphilitic gummas or tubercles, sclerosing glossitis. At the same time, syphilitic gummas differ from secondary syphilides by deeper penetration into the skin and mucous membranes and involvement in the pathological process of the central nervous system and other body systems. Tertiary syphilis can cause paralysis due to irreversible destructive processes.
The tertiary period of syphilis, fortunately, is rare, since patients seek help at the first stage of the disease. The tertiary period of syphilis is observed in patients who have undergone either poor quality treatment for syphilis or incomplete treatment. The literature identifies some predisposing factors for the occurrence of the tertiary period of syphilis:
- Childhood or old age;
- Alcoholzym;
- Presence of concomitant difficult-to-treat pathology
The tertiary period of syphilis lasts 8–10 years. For syphilitic gummas to appear, not 1, but at least 3 months must pass. An important feature of the course of the tertiary period is that after the disappearance of the gumma, scars remain.
If a bump appears, it is most often on the lips. The clinical picture of tubercular syphilis: the tubercles are red-blue in color, initially located singly, merge over time, after the collapse of which ulcers appear: painful, deep, small, with undermined edges. The ulcer heals - a scar for life.
Syphilitic gummas will be located in the oral cavity. There are always few of them. Either in a group or alone. The size of syphilistic lips is small, often compared to a nut. After the gumma disintegrates, an ulcer appears, which has undermined, uneven edges, often covered with granulations, and a dense bluish-red ridge at the bottom. Gummas can perforate the hard/soft palate if left untreated.
Most often, syphilitic gummas occur on the tongue, which leads to the development of syphilitic sclerous glossitis. The tongue thickens, becomes dense and less mobile. Permanent deformation of the tongue occurs.
When the syphilitic gum disintegrates on the alveolar process, pathological mobility of the teeth occurs; percussion will be positive.
Congenital syphilis
Congenital syphilis occurs in children when Treponema pallidum penetrates the placenta from a mother who has syphilis. Intrauterine infection occurs at the border between 3 and 4 months of pregnancy.
Congenital syphilis can be early, that is, it appears immediately after birth, within 1 - 2 months; may be late - manifests itself between 5 and 14 years.
Early congenital syphilis - Clinical picture
The clinical picture of early congenital syphilis is entirely variable. The pathological process involves not only the skin and mucous membranes, but also bones, organs, and the central nervous system.
If the manifestation is on the skin, it is syphilitic pemphigus. The bubbles are dense, with a purple rim around them.
The manifestation of early congenital syphilis on the skin of the chin or lips is characterized by Hochsinger infiltration. That is, erythema occurs either in the form of a focus or in the form of diffusion. After which infiltration develops. The skin becomes dense and loses elasticity. Lips swell and increase in size. The lips also change in color, a yellowish tint appears. If a child screams, this leads to injury, as cracks appear. The cracks often bleed and subsequently become covered with crusts. If treatment aimed at epithelization is not effective or is not carried out, then Robinson-Fournier scars appear - radial scars in the area of the corners of the mouth.
Late congenital syphilis - Clinical picture
The clinical picture of late congenital syphilis manifests itself in the period from 5 to 14 years and is characterized by the most severe changes that cause deep damage to tissues and organs.
There are two groups of symptoms by which late congenital syphilis can be diagnosed:
- Reliable signs: Hutchinson's triad: keratitis, Hutchinson's teeth, deafness;
- Probable signs: perioral scars, buttock-shaped skull, saddle nose, saber-shaped shins, purse-shaped first molars and canines.
Treatment of syphilis
Treatment of syphilis should be carried out by a dermatologist in specialized medical institutions. The dentist can only carry out local treatment: oral hygiene, antiseptic rinses, elimination of irritants.
The article was written by N. Shidlovskaya specifically for the OHI-S.COM website. Please, when copying material, do not forget to provide a link to the current page.
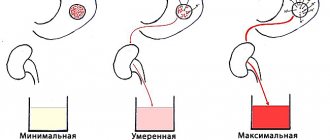
Stages of gastritis
- Hyperemia. At the first stage of gastritis development, hyperemia (redness) of the gastric mucosa is observed. This is a protective vegetative-vascular reaction - dilation of blood vessels and increased blood flow in response to a negative effect on the mucous membrane. Hyperemia is accompanied by edema, this is a sign of the development of inflammation.
- Chronic inflammation, metaplasia, dysplasia. The production of hydrochloric acid decreases, the mucous membrane thickens. Hypertrophy is typical for people who abuse alcohol. Inflammation is characterized by the accumulation of leukocytes in the stomach wall; prolonged inflammation can change the structure of the gastric epithelium, it can become similar to intestinal epithelium, this phenomenon is called metaplasia and may be associated with an increased risk of cancer. But the risk is especially high if a biopsy reveals a violation of the structure of the tissue and cells of the stomach - dysplasia.
- Atrophy. Prolonged inflammation causes thinning of the gastric mucosa, recovery processes slow down, atrophic changes in the mucosa are observed - epithelial cells die and are replaced by scar tissue.
- Erosion and ulcers are a frequent companion to gastritis. Focal and profound changes develop due to a decrease in the performance of the mucous glands, thinning of the protective layer, in most cases this is a consequence of exposure to H. pylori.
Clinical manifestations
Patients whose gastric mucosa is severely hyperemic rarely realize this. Some symptoms may not be related to the gastrointestinal tract at all. At the initial stage, the heart rate increases. Drowsiness or problems with urination appear. Depending on where the foci of severe hyperemia are localized, the patient experiences:
- fatigue;
- obesity;
- swelling of the face.
Treatment of gastritis
Treatment for gastritis depends on the cause. Acute gastritis caused by taking NSAIDs or alcohol abuse does not require drug therapy; it is enough to exclude these triggers.
In other cases, your doctor may recommend:
- Antibiotic therapy against H. pylori.
- Drugs that block the production of hydrochloric acid (a component of gastric juice) and promote healing of the mucous membrane (proton pump inhibitors* - omeprazole, lansoprazole, rabeprazole, esomeprazole, dexlanzoprazole, pantoprazole.
- Antacids** (neutralize stomach acid, relieve pain).
* - Long-term use of proton pump inhibitors, especially at high doses, may increase the risk of hip, wrist and spine fractures, and an osteoporosis prevention program may be required. ** - Side effects - constipation, diarrhea.
Features and advantages of the gastritis treatment method at the Rassvet clinic
Diagnosis and treatment of gastritis at the Rassvet clinic is carried out in the gastroenterology department. We use evidence-based methods based on international clinical guidelines. Your primary treatment will begin only after a physical examination and all necessary tests and diagnostic tests have been completed.
Important. The influence of certain foods or dietary systems on the risk of gastritis has not been proven by research.
At the Rassvet Clinic, we first of all distinguish gastritis from functional dyspepsia. Gastritis is often asymptomatic, but it is necessary to treat it, since it is a slow but sure road to stomach cancer. Functional dyspepsia, on the contrary, is accompanied by many complaints, but endoscopic examination and biopsy do not reveal pathology.
How gastritis is treated at the Rassvet clinic
To clarify the diagnosis, we use the most modern and accurate equipment and logistics methods. For example, we have built a system for diagnosing gastritis and determining cancer risk according to the OLGA classification. Our endoscopes allow you to perform gastroscopy with multiple magnification and examine the mucous membrane through light filters, taking a biopsy from the most suspicious areas. The biopsy samples themselves are also assessed by the histologist using the OLGA scale, and as a result we obtain a figure that reflects the risk of oncological transformation in the coming years. Further treatment tactics depend on the value of this figure.
We value the comfort of patients, so in Rassvet you can undergo an examination under anesthesia in the shortest possible time.
Recommendations from a gastroenterologist at the Rassvet clinic for patients with gastritis
Timely consultation with a doctor and proper treatment will help keep the disease under control. A strict diet is not needed. However, the rules of a healthy diet should be followed - do not overeat, avoid foods that irritate the mucous membranes (smoked, fried, fatty), and give up alcohol. If you are forced to take painkillers that increase the risk of gastritis, check whether they can be replaced with a drug that is less aggressive on the gastric mucosa (acetaminophen, paracetamol).