What is toxic neutrophil granulation?
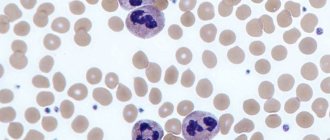
An important morphological abnormality of neutrophils is “toxic granularity.”
Toxic changes in neutrophils are not necessarily associated with “toxemia.” The term comes from the fact that the abnormalities were first noticed in patients with gram-negative sepsis and endotoxemia. However, morphological changes do not indicate a “toxic effect” of bacteria on leukocyte granulocytes. Toxic granulation is an abnormality acquired during the maturation of neutrophil granulocytes. Accelerated maturation occurs in conjunction with stimulation of the release of cytokines that respond to inflammation. Animals recovering from bone marrow injury or receiving hematopoietic cytokines (granulocyte colony-stimulating factor) may have toxic granularity. On a standard hemogram, the presence of toxic changes is indicated in WBC tests and is subjectively graded as mild, moderate, or excessive.
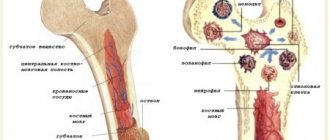
Life of neutrophils
Neutrophil cells are formed in the bone marrow (like other blood cells) from the precursor cells of all leukocytes - myeloblasts. As the latter changes (their division), 16 or 32 neutrophilic granulocytes can form. This period takes an average of 5 days, after which the blood cells enter the main bloodstream, where they perform their functions for 9 hours, constantly moving.
If a foreign agent is not encountered on the way of abs cells, then their life lasts from a week to two, otherwise some neutrophil granulocytes live only 5 days within the bone marrow. What do cells manage to do during their existence?
Toxogenic granularity of neutrophils (TNG)
A qualitative change in leukocytes is dark, large, coarse granules inside a leukocyte, formed as a result of physicochemical changes in the protein structure of the liquid part of the cytoplasm - protein coagulation under the influence of intoxication products and protein agglomeration, around ordinary neutrophil grains. The protein is, as it were, cooked during the process of inflammation.
Importance in the clinic
TZN is characteristic of intoxication of the body during purulent processes, inflammatory processes of coccal etiology, decay of tumor tissue, the action of ionizing radiation, as well as degenerative changes in the bone marrow due to previous prolonged excessive stimulation of granulopoiesis or with primary inhibition of granulopoiesis, without previous stimulation. But it is absent in tuberculosis (used to exclude it in differential diagnostics with pneumonia of another origin), tetanus, encephalitis, and typhus.
Taurus Knyazkova-Dele
Large pale blue lumps of various shapes in the cytoplasm of neutrophils, representing RNA and fragments of rough endoplasmic reticulum. They are observed in scarlet fever, sepsis, measles, pneumonia, burns, etc. It is believed that they have the same origin as TND and occur when TND is not fully expressed or is completely absent.
Amato grains
Small round oval or comma-type formations painted in a pale blue color; they contain red or red-violet grains. Amato grains have been described in scarlet fever, but are also found in other infections. Close to Dele bodies.
Vacuolization of the cytoplasm
It is observed less frequently than TND, but has no less diagnostic value, indicating the severity of the disease and intoxication. Most typical for severe forms of sepsis, abscesses, and acute liver dystrophy. Sometimes there is almost total vacuolization of all leukocytes: “holey”, “shot through” leukocytes. It occurs as a result of the dissolution of fat droplets in a fatty degenerated cell (fatty degeneration) when fixed with alcohol, that is, in prognostic terms, a more formidable symptom than TZN, since TZN indicates protein degeneration of cells, and vacuolization indicates a deep form of cellular degeneration.
Changes in the size and shape of leukocytes
- Anisocytosis of leukocytes
- leukocytes of various shapes are found. A sign of severe toxicosis in sepsis, tuberculosis, pernicious anemia. - Cell shrinkage
- microforms of leukocytes. Clear degenerative sign: - Discrepancy in the development of the nucleus and cytoplasm
- the neutrophil nucleus is mature, the cytoplasm is basophilic, young and vice versa.
Microscopic features
When toxic granularity appears, the appearance of neutrophils changes, which is clearly visible in an electron microscope.
Morphological signs of a neutrophil when pathological granularity appears:
- 2-3 times more than a mature red blood cell
- Low nucleus to cytoplasm ratio (more cytoplasm than nucleus)
- The nucleus is mature and divided into 3-5 lobes connected by thin threads of chromatin
- Nucleols are absent
- Darker (red/purple) granules are easily visible (similar to primary granules noted in promyelocytes)
Appearance of coarse granularity in the cytoplasm
If you compare a toxically altered cell with a normal one, one significant difference will emerge - next to the usual granules of neutrophils, toxic granularity appears, which looks like larger rounded formations of dark red and purple color. The appearance of additional granules in neutrophils is due to coagulation (gluing) of cytoplasmic protein, which under a microscope looks like the appearance of additional granularity against the background of existing granules.
Why does toxigenic granularity of neutrophils occur?
Normally, neutrophil granulocytes contain inclusions called grains. Toxic granularity of neutrophils appears due to infectious diseases, disorders of hematopoiesis, taking medications or receiving a strong dose of radiation. Under the influence of infection, chemical reactions occur that lead to coagulation of protein compounds. These proteins attach to cell granules, causing toxic granularity of neutrophils.
Common causes of toxigenic granularity of neutrophil granulocytes:
- Chemotherapy.
- Overdose or drug poisoning.
- Inflammatory or infectious processes.
- Scarlet fever.
- Malignant and benign neoplasms.
- Hereditary diseases of the hematopoietic system.
- Inflammation of internal organs.
- Severe purulent processes.
- Bacterial infections of various etiologies.
In mild forms, toxic granularity of neutrophils is a normal variant. It occurs in pregnant women and poses no danger to either the fetus or the woman. Toxogenic granularity of neutrophils is observed in children with a rare hereditary disease - Chediak-Higashi. Cancer tumors affect the morphology of neutrophil granulocytes, so constant monitoring of the condition of cancer patients is necessary. The cause of pathological granulation may be primary immunodeficiencies that affect leukocyte granulocytes and the entire immune system.
Attention! There are many diseases that affect neutrophil granulation. It is necessary to consult with your doctor and undergo additional examinations to determine the cause of the morphological anomaly.
Tests required to detect graininess
The most important study to clarify the diagnosis is the analysis of changes in the leukocyte series. This study is very significant for differentiating diseases. For example, any pathological changes in the lungs cause a neutrophil shift to the left, while changes in the oncological nature do not cause degenerative granulation. Any inflammatory processes, on the contrary, always cause such a state of cells.
To detect toxic granularity of neutrophils in a child and an adult, a special laboratory test of a blood sample is performed using methylene blue and fuchsin. The latter is prepared as follows:
- By heating one gram of dye is dissolved in 15 grams of 96% ethanol.
- After this, a 5% solution of carbolic acid in an amount of 100 grams is added to the resulting mixture.
- Then 7 drops of the resulting staining solution and 1% methylene blue in an amount of 5 drops are added to 20 ml of water. The resulting solution is thoroughly diluted, then the smears are stained with it for one hour. After this, they are washed off and dried. This method allows you to examine granularity (flakes, dust) under a microscope.
- What does it mean to have a decrease in neutrophils and an increase in lymphocytes in the human body?
Changes in leukocyte morphology
In blood granulocytes during severe infections, the following types of changes in leukocyte morphology have serious prognostic significance: toxogenic granularity of neutrophils, vacuolization of the cytoplasm, Knyazkov-Dele bodies. The presence of at least one of the listed changes indicates the development of bacteremia and generalization of the infectious process. Changes are quantified using the degeneration index
, which reflects the percentage of neutrophils that have toxogenic granularity. If this index exceeds 50%, this indicates a high severity of infection and a serious prognosis. It has been reliably established that the presence of vacuoles in the cytoplasm of neutrophils correlates well with impaired granulocyte function and the presence of bacteremia.
Toxogenic granularity of neutrophils
- coarse granularity of a dark red color, which is detected as a result of physicochemical transformations of the cytoplasm under the influence of an infectious agent, which reflects a violation of the processes of neutrophil maturation, or is the result of the absorption of toxins. The causes of toxogenic granularity of neutrophils are purulent-septic diseases, lobar pneumonia, scarlet fever, and disintegration of tumor tissues after radiation therapy.
Vacuolization of the cytoplasm
- detected in sepsis, abscesses, acute liver dystrophy.
Taurus Knyazkova-Dele
- are large white-blue areas of cytoplasm of various shapes that do not contain specific granules. Knyazkov-Dele bodies are detected in inflammatory diseases, infections, sepsis, and burns.
Hypersegmentation of neutrophil nuclei
- 5 or more segments in the nuclei of neutrophils. Causes: folate deficiency and B12 deficiency anemia, hereditary constitutional feature.
Pelger anomaly
- a dominantly inherited disorder of granulocyte maturation, which is characterized by a decrease in the segmentation of neutrophil nuclei.
Pseudo-Pelger anomaly
- decreased segmentation of granulocyte nuclei. The abnormality of nuclear maturation is based on a violation of nucleic acid metabolism. Causes: myeloproliferative diseases, agranulocytosis, multiple myeloma, tuberculosis. Pseudo-Pelger anomaly is transient, and after the end of the disease, pseudo-Pelger leukocytes disappear.
Leukolysis cells (Botkin-Gumprecht shadows)
- dilapidated nuclei of lymphocytes with remnants of nucleoli, found in chronic lymphocytic leukemia.
Top of page
Top of page
ATTENTION! The information provided on this site is for reference only. Only a specialist doctor in a specific field can make a diagnosis and prescribe treatment.
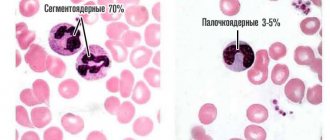
Types of toxic granularity of neutrophil granulocytes
To determine the severity of morphological changes in leukocyte granulocytes, a special classification is used - the plus system. It allows you to assess the nature of degenerative changes, the number of pathological cells as a percentage of the total volume of leukocyte granulocytes. Types of pathological granularity of neutrophil granulocytes:
- Toxic granulation + is characterized by the presence of fine “dust-like” granulation.
- Two pluses mean that granulation has average values, and the number of diseased neutrophils in the blood is more than half.
- Toxic granularity with three pluses is characterized by large, modified granules. About 80% of neutrophils in the disorder have degenerative morphological changes.
- With four pluses, almost all cells are deformed. Often this disorder ends in death, and therefore requires urgent intervention from specialists.
In addition to the above changes in the blood product, five main features of toxic changes in neutrophil granulocytes are observed:
- Cytoplasmic basophilia.
- Cytoplasmic vacuolation.
- Presence of Dele bodies.
- Immaturity of nuclei in cells.
- Toxic granulation.
Toxic granulation of leukocyte granulocytes
Normal neutrophil counts
Normally, toxic granulation is absent in leukocyte granulocytes or is present, but to an insignificant extent. In some normal conditions, degeneration of neutrophil granulocytes occurs. Pregnancy, the postoperative period, the period of recovery after a purulent-septic disease are the reasons why toxic granulation may occur. This condition goes away on its own and does not require drug intervention.
Advice! An increase in the level of neutrophils indicates the presence of pathological processes in various organ systems. Often toxic granulation ends in death. If these morphological changes are detected in blood tests, you must immediately contact your doctor. Timely diagnosis and treatment can prolong the patient's life.
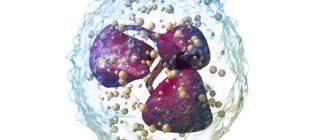
Functions of ABS cells
The entire functioning of neutrophil granulocytes is aimed at fighting bacteria (neutrophils are practically indifferent to other pathogens). This is done in several ways:
- Phagocytosis;
- Stimulation of immunity;
- Netosis.
Principles of phagocytosis
Phagocytosis is the phenomenon of capture, “envelopment” (similar to the action of an amoeba) and digestion of a foreign bacterium by neutrophilic leukocytes. Neutrophil granules contain many lysosomal enzymes, which break down proteins of foreign bodies. After such an intense attack, the protective cell itself dies, but manages to destroy about 7 microorganisms. At its core, this group of blood cells are suicides (kamikazes), who sacrifice themselves for the health of the entire body.
This feature of cells directly indicates the body’s ability to fight infection. In a blood test for the quality of immune function, there is such an indicator - “phagocytic activity of neutrophils”, it indicates how many foreign microorganisms were “eaten” by kamikaze cells contained in 1 ml of blood over a certain period of time in a laboratory. This is an important diagnostic criterion.
The process of antibody production begins only after the pathogen is “eaten” by neutrophil granulocytes. After splitting into components, information about a foreign microorganism becomes available to each blood cell and the immune system as a whole. It begins to work intensively, activates defense mechanisms, forms antibodies, and directs even more protective cells to the site where the “pest” is detected.
Features of netosis
Netosis is another important mechanism of neutrophil function, discovered only in 2004. When a neutrophil granulocyte detects a pathogenic microorganism, complex processes begin in its nucleus: it is destroyed with the formation of individual strands of chromatin, there is an intensive accumulation of radicals and various toxic substances that interfere with the normal functioning of living cells.
Degenerative changes in neutrophils
The study of the leukocyte formula is given special diagnostic importance, since it clearly demonstrates the characteristic changes that occur in a number of diseases. However, the data obtained must be considered with other data from the blood system, taking into account the general condition of the patient. Toxic granularity of neutrophils is a sign that appears when cells are exposed to an infectious factor (poisoning, sepsis, pneumonia, scarlet fever and other diseases). The severity of the infectious process is indicated by the number of neutrophils containing toxic granules exceeding 50%.
Neutrophils, being one of the many representatives of the forms of leukocytes in the blood, purify the blood, destroying bacteria and viruses, and removing harmful substances. When identifying various diseases based on the results of a blood test, the entire set of defining signs is taken into account:
- total white blood cell count
- nuclear shift of neutrophils, promoting the appearance of immature forms of neutrophils in the blood
- percentage of leukocyte forms
- presence/absence of disorders and changes in cells.
A physiological increase in neutrophils often occurs during physical activity, emotional arousal, and childbirth.
Various pathological conditions (infections, diseases of the hematopoietic apparatus, exposure to chemicals, penetrating radiation, ingestion of radioactive substances, and others) lead to degenerative changes in neutrophils, which can affect the nucleus and cytoplasm. Toxic granules of neutrophils are coarse granules similar to azurophilic granules. The formation of granularity occurs inside the cell due to physicochemical modifications of the protein structure of the cytoplasm under the influence of intoxication products, and is often accompanied by the presence of cytoplasmic vacuoles.
Toxic granularity may appear before the nuclear shift, with a further increase especially in lobar pneumonia, septicopyemia, scarlet fever, peritonitis, purulent-septic diseases and other inflammatory diseases, which clearly indicates the progression of the pathological process. A significant amount of it is observed during the disintegration of tumor tissue under the influence of radiation therapy.
To identify toxic granularity, special staining methods are used, the most common being the Freifeld method. Among the degenerative changes in neutrophils, Dele bodies, cytoplasmic vacuoles, hypersegmentation of neutrophils, ring-shaped nuclei, chromatinolysis, pyknosis, karyolysis, cytolysis and others are also known.
(2 ratings, average 4.5 out of 5)
Diagnostics of toxic and toxogenic granules in laboratory conditions
Usually, in order to identify such pathologies, the leukocyte formula is calculated in the laboratory. In textbooks and manuals you can find a description of the method under the name “Romanovsky staining method.” Intense, pronounced granularity appears in neutrophils and is clearly visible if present. Such granularity is not typical for healthy cells. The graininess in the form of spraying over the entire plane should be especially alarming. A blood test uses a smear. To accurately determine the type of grain, the Freifeld staining method is used. This method uses fuchsin and methylene blue. The result of the analysis should indicate not only the presence or absence of granulation, but also various distinctive features. For example, the massiveness of individual granules, uniformity, dustiness. A percentage is used to display the stage of the disease.
Toxigenic activity in blood tests
August 29, 2020
Hello! On August 27, a 3-year-old child had a nose injury, a fracture was ruled out, and a bruise was diagnosed. On the night of the 28th, the temperature rose to 38.8, it was not going well. On the 28th we saw an ENT specialist and a pediatrician, both said that the temperature was not related to the injury. The throat and ears are calm, saturation is 99 percent, there is no pain when palpating the peritoneum, everything is in its place, its size. The child's stool, appetite, and activity are as usual. We donated blood at the blood clinic and it’s ready today. In the analysis I saw toxigenic activity + ... CRP 30. God, what is this? I am attaching the file.
On the Ask a Doctor service, you can consult a pediatrician online on any problem that concerns you. Expert doctors provide consultations around the clock and free of charge. Ask your question and get an answer immediately!
Pediatrician
Good afternoon. The photo is not visible yet. The only complaint is temperature?
Margarita, August 29, 2020
Client
Albina, yes. No cough, no runny nose. And the temperature hit quite suddenly.
Pediatrician
And two weeks ago you didn’t have any purulent diseases?
Pediatrician
The blood shows signs of a bacterial infection. I would prescribe you an antibiotic. We need to look at some more urine. Isn't it cloudy for you?
Pediatrician
Good afternoon. A blood test shows signs of a bacterial infection. Take a urine test and re-visit your pediatrician to decide on antibiotic therapy.
Pediatrician
Hello. According to the analysis, there is a pronounced bacterial process (increased neutrophils, band neutrophils, toxic granularity, SRP). We need to look for the reason. First of all, take a urine test. Liver pathology may not have obvious symptoms. According to the analysis, antibiotics are needed. But we need to determine what to treat. We are treating the child, not performing an analysis. All the best.
Pediatrician
Hello, the blood is bacterial, take an x-ray of the lungs, sinuses, give urine, ultrasound of the abdominal cavity, kidneys
You need to start antibacterial therapy, the treating doctor should select the right antibiotic for you
Get well!
Pediatrician, Psychotherapist
Hello!
Based on the result of a bacterial process in the blood, antibiotic administration is required, it is necessary to find out the cause of this process, rule out pneumonia (by doing a chest x-ray), and urinary tract infection (by passing urine according to all collection rules).
ENT, Pediatric ENT
Hello.
This is a bacterial infection and requires a course of antibiotics
Pediatric ENT, ENT
Hello. The child has an infection caused by bacterial flora. Did the pediatrician listen to your lungs during the examination? Is anyone in the family sick?
Margarita, August 31, 2020
Client
Edward, We listened and the saturation is 99 percent, no one is sick, we regularly test for Covid. Below she answered that it was probably post-traumatic, the urine was ideal, the temperature no longer rose. Now let's repeat the blood. Thanks for the answer.
Pediatrician
The child has a bacterial infection.
Treatment with antibacterial drugs is necessary.
Infectious disease specialist
Hello! The blood is inflammatory. An examination and a course of antibacterial and detoxification therapy are necessary. Start taking the drug Suprax in an age-specific dosage. Take a general urine test.
To remove toxins, give lactofiltrum.
Pediatrician, Therapist, Masseur
The nose injury happened 3 days ago. The body is restored, the blood reflects this process. Regarding antibiotic therapy, so that there are no problems with injury, it is imperative to look inside and outside the nose. If the swelling is hyperemia, you should be prescribed an antibiotic.
Margarita, August 31, 2020
Client
Natalya, Hello! Perhaps you will be right. The temperature lasted for a day and went away on its own and did not rise again. We passed the urine clinic and according to Nechiporenko, the analysis was perfect, I attached it to my profile. This is probably really post-traumatic. On Wednesday, September 2, we will donate blood again. Our pediatrician said that if the picture is much better, it means the consequences of the injury, if not, an ultrasound of the peritoneum, a search for the disease.
Pediatrician, Therapist, Masseur
I wouldn’t say so directly that there is horror, an inflammatory reaction, in case of injury, this is possible. Leukocytes are generally within the normal range of 10.0, granulocytosis is explainable. Do not give any antibiotics prescribed in absentia on the Internet, only a consultation with the surgeon who looked at the nose
Pediatrician
Hello, donate blood for web CMV HSV toxoplasma chlamydia and mycoplasma using the IFA method immunoglobulins gm
Anesthesiologist-resuscitator, Pediatrician
Still, this is not a reaction to trauma. The SRP would not have increased that way.
Anesthesiologist-resuscitator, Pediatrician
The infection is bacterial. Give your urine and once again go to the ENT specialist to check the injury site
Anesthesiologist-resuscitator, Pediatrician
Antibiotics are needed. But we need to find the source of infection
Rate how helpful the doctors' answers were
1 person voted
average rating 4
What should I do if I haven't found the answer to my question?
If you have a similar or similar question, but you haven’t found the answer, ask your question to a doctor online.
If you want to get a more detailed consultation with a doctor and solve the problem quickly and individually, ask a paid question in a private personal message. Be healthy!