The largest arterial vessel in the human body is the aorta. It originates from the left ventricle of the heart, runs along the spine and supplies oxygenated blood to all organs and tissues.
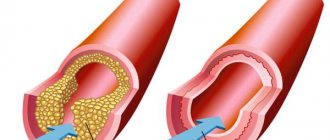
Damage to the aorta occurs as a result of a violation of cholesterol metabolism in the body. At the same time, low and very low density cholesterol accumulates in the endothelium of the vessel, which leads to the proliferation of connective tissue in its wall and a decrease in elasticity. Further development of the pathology causes the formation of an atherosclerotic plaque, which constantly increases in size and reduces the patency of the artery. Violation of the integrity of the plaque leads to its instability, accumulation of platelets on the surface of the formation, which significantly reduces the lumen of the vessel and slows down blood circulation.
Aortic sclerosis can develop anywhere and occurs as a result of the formation of an atherosclerotic plaque consisting of cholesterol, fats and calcium in the vessel wall. The disease develops after the age of 40, and the male population is affected more often than the female population.
Why is atherosclerosis of the aorta really dangerous?
The aorta is a vessel on which the blood supply and nutrition of almost all vital organs depends. From the thoracic region, where the aorta begins, leaving the heart, its branches go to the organs of the chest and the brain. From the abdominal region, where the aorta descends, branches supply all the abdominal organs, kidneys, pelvis and lower limbs. If the lumen of the aorta in the thoracic or abdominal region narrows or, worse, becomes clogged, a deficiency of blood supply develops in certain organs associated with the aorta, which can lead to life-threatening complications in all organs and systems. Did you know that...
- Most often, people over 60 years of age suffer from atherosclerosis of the aorta and its branches, but you can also get sick at a young age
- Sometimes the initial signs of aortic atherosclerosis are detected even in children 10-12 years old: this suggests that this disease can develop for decades without showing itself in any way
- The risk of developing aortic atherosclerosis is approximately twice as high if you are over 40, smoke, drink alcohol, are sedentary, and consume unhealthy foods such as fast food
- No one is immune from atherosclerosis: even if you have been taking care of your health since childhood and feel great, it is not a fact that you do not have this disease
Remember: to find out for sure how healthy your blood vessels are, contact our specialists who will conduct an accurate diagnosis and assess your risks. Sign up now.
Clinical picture
Symptoms of the disease depend on the level of damage to the aorta, which is divided into the thoracic and abdominal parts. The thoracic section of a large artery supplies blood to the brain, heart, lungs, and upper limbs. Vascular branches from the abdominal part supply blood to the kidneys, abdominal and pelvic organs, and lower extremities. In severe cases of sclerosis, the entire length of the aorta may be affected, which is manifested by the diversity of the clinical course of the disease.
The disease includes several stages:
- Preclinical period – changes are observed with laboratory and instrumental research methods.
- Period of clinical manifestations – symptoms of the disease are revealed, depending on the level of vascular pathology.
Stages of development of aortic atherosclerosis
- Ischemic – manifested by attacks of angina, claudication, abdominal pain, increased blood pressure
- Thrombonecrotic – stage of life-threatening complications, including myocardial infarction, stroke, gangrene, renal failure and others
- Fibrous - when the disease develops over a long period of time, fibrous tissue replaces other types of tissue and disrupts the normal functioning of the relevant organs
Please note: symptoms of aortic atherosclerosis begin to appear when the disease progresses and ischemia (lack of blood supply) develops in one of the areas of the blood supply to the organ.
Classification of forms of the disease:
Celiac stenosis (supplies blood to the liver, spleen, stomach, pancreas)
This is a condition in which the lumen of the celiac trunk narrows, can be acquired - develops when the vessel is damaged by atherosclerosis, or congenital - when compressed from the outside by the arcuate ligament of the diaphragm (much less often - with inflammatory diseases, aortic aneurysms, congenital malformations, compression by neoplasms of the abdominal cavity). The first reason is often combined with damage to other arteries (coronary - intracardiac arteries, carotid, arteries of the lower extremities), the second reason is a congenital condition, the manifestations of which develop at a young age. The main organs experiencing a lack of blood supply are the stomach, liver and pancreas, but the intestines also suffer due to the “steal syndrome”. Significant narrowing of the lumen of the artery is currently considered to be more than 50% of the original diameter. Symptoms of the disease - abdominal pain, bloating, stool disorders in the form of alternating diarrhea and constipation, nausea, weight loss - are combined into a single syndrome - the syndrome of “chronic abdominal ischemia” (chronic ischemic disease of the digestive organs, abdominal ischemic disease).
The cause of the narrowing of the vessel can be determined using:
- duplex scanning of abdominal vessels,
- performing angiography or multislice computed tomography angiography (MSCT angiography).
When establishing indications and choosing a method of surgical treatment, the patient’s age, the severity of complaints, the effectiveness of conservative treatment (without surgery), and the degree of compensation for the functions of the involved organs are taken into account. Indications for surgical treatment, according to modern standards, should be established jointly by a gastroenterologist and a vascular surgeon.
There are the following types of operations:
- Endovascular balloon angioplasty with celiac axis stenting.
This intervention is performed through a puncture in the femoral, and less commonly, in other arteries. Using special thin instruments, the narrowed section of the celiac trunk is expanded from the inside until the normal diameter of the lumen is restored, and a stent is installed - a thin “frame” made of inert alloys, which subsequently prevents re-narrowing of the artery. It is most often used when the celiac trunk is damaged by atherosclerosis. - Laparoscopic decompression of the celiac trunk.
The operation is performed minimally invasively using separate punctures. This method allows you to incise the ligament of the diaphragm, “releasing” the celiac trunk from its pressure. In this case, the artery straightens, eventually restoring its normal diameter. Previously, such operations were performed on the open abdominal cavity, which was sometimes accompanied by a difficult postoperative period, characteristic of open operations, so their prevalence was limited. The development of laparoscopic surgery has made it possible to perform these interventions with good postoperative and cosmetic results. - Shunt operations for narrowing/blockage of the celiac trunk or its prosthetics.
They are performed in advanced stages of atherosclerosis, when it is not possible to install a stent or remove an atherosclerotic plaque from a vessel. The essence of the operations is to create a bypass blood flow in addition to the affected celiac trunk, or to replace it with an artificial prosthesis. These interventions are technically complex, are performed only in the open abdominal cavity and require highly qualified vascular surgeons.
Stenosis of the superior mesenteric artery
It is much less common than celiac stenosis. The most common causes of the disease are atherosclerotic narrowing of the lumen of the superior mesenteric artery (against the background of systemic atherosclerosis) and a congenital disorder of the structure of the artery wall - fibromuscular dysplasia. The superior mesenteric artery branches into many smaller vessels that supply the small intestine and part of the colon. The disease often occurs without any symptoms and is difficult to diagnose until serious complications occur—complete blockage of the superior mesenteric artery or its branches. In this condition, patients are admitted to a surgical hospital with signs of transient necrosis of a section of the intestine deprived of blood supply, which is sometimes very difficult to distinguish from other acute surgical diseases of the abdomen. In this case, an emergency operation is required - resection of a non-viable section of the intestine.
You can make a diagnosis in the early stages using:
- Doppler ultrasound of the abdominal aorta and its branches (diagnostic efficiency is about 50%),
- magnetic resonance imaging (diagnostic efficiency is about 80%),
- angiography of the abdominal aorta and its branches (allows us to determine the presence of vessel narrowing in 90% of cases).
Treatment for early detection of stenosis of the superior mesenteric artery is similar to the treatment of systemic atherosclerosis, however, with significant narrowing of the artery, surgical intervention - endovascular angioplasty - is possible.
Renal artery stenosis
Narrowing of the renal arteries develops as a result of atherosclerotic lesions, as well as with a more rare disease - fibromuscular dysplasia. Violation of blood flow to one or both kidneys is accompanied by a general negative reaction of the body. A kidney experiencing a blood deficiency receives false “information” about the total blood volume, and begins to react as if the total amount of blood in the body has decreased. The processes of hormone synthesis are intensified, aimed at retaining water in the body to maintain a constant volume of fluid in the general bloodstream. This mechanism is pathological, since the amount of blood remains the same, and, due to the production of renal hormones, an additional volume of water from the cells enters the bloodstream. As a result, persistent renal arterial hypertension develops - an increase in blood pressure above normal levels, which is difficult to reduce with medications. Swelling and cardiac dysfunction appear. This type of arterial hypertension is usually recognized in time by attending physicians, and ultrasound examination can often detect damage to the renal arteries. Open surgery to restore blood flow through the renal artery - bypass, prosthetics (replacement) of the affected area is now being performed less and less often, they are being replaced by minimally invasive endovascular methods - angioplasty and stenting.
Signs of atherosclerosis of the aorta: thoracic region
- Severe chest pain (aortalgia) - lasts several hours and even days, the pain is burning, pressing, radiates to the left and right arm, shoulder, neck, spine, interscapular area, while nitroglycerin does not help
- Heart failure with attacks of suffocation - occurs because the affected aorta increases the load on the heart
- Increased blood pressure
- Difficulty swallowing, hoarseness of voice
- Retrosternal attacks of angina - pain radiates to the left arm and left half of the chest
- Shortness of breath and palpitations
- Dizziness, short-term fainting, pallor of the face, headaches with high blood pressure, memory impairment, increased fatigue, pulsation between the ribs to the right of the sternum, convulsions when turning the head - all these symptoms are caused by a lack of blood supply to the brain
Damage to the thoracic artery
The aortic root is located at the exit of the left ventricle in close proximity to the semilunar valve. Its atherosclerotic changes cause vasoconstriction, which leads to increased pressure in the left side of the heart and pulmonary circulation. The semilunar valve changes as a result of changes in hemodynamics (blood movement), and its insufficiency develops.
Damage to the aortic root leads to semilunar (aortic) valve insufficiency
When the pathological process is advanced, an insufficient amount of blood enters the systemic circulation, which stagnates in the lungs. This leads to pneumosclerosis (replacement of lung tissue with fibrous tissue), impairs the enrichment of blood with oxygen, and causes the development of organ hypoxia (insufficient oxygen supply). Increasing hypertrophy of the left ventricle compresses the coronary arteries and leads to ischemic damage to the heart, leading to myocardial infarction.
Three large arterial vessels branch from the aortic arch: the brachiocephalic trunk, the left common carotid and the subclavian artery. They supply blood to the neck, upper limbs, head, including the brain. The most severe is damage to the blood vessels of the brain, which can result in the development of hemorrhagic and ischemic strokes.
Clinical manifestations of aortic sclerosis in the thoracic part:
- pressing pain behind the sternum, spreading to the neck, arms, epigastrium, interscapular area;
- hoarseness of voice, difficulty swallowing (with damage to the arterial arch);
- an increase in systolic (upper) blood pressure, while diastolic (lower) remains within normal limits;
- headaches and dizziness, fainting;
- convulsions with a sudden change in body position;
- pulsation in the intercostal area of the right half of the chest;
- formation of wen on the face and neck, change in the color of the iris (trophic disorders).
The disease is characterized by a long asymptomatic course and is often diagnosed at the stage of development of severe complications such as myocardial infarction and cerebral stroke.
Atherosclerosis of the abdominal aorta: symptoms
Atherosclerosis of the abdominal aorta disrupts the blood supply to the internal organs and lower extremities, which is why the symptoms can be very diverse:
- Pain in the navel area is an intermittent “wandering” character, accompanied by bloating and constipation
- Increased blood pressure as a result of renal ischemia
- Weight loss – occurs due to disturbances in the digestive system
- No pulsation in the navel area, under the knees and on the back of the feet
- Problems with sexual life in men, infertility
- Pain in calves when walking that goes away when you stop
- Intermittent lameness
- Numb feet
- Cold feet
- Swelling and redness of the legs and feet
- Necrotic ulcers on the skin of the legs - occur in the last stages of the disease
Remember: aortic atherosclerosis is a dangerous disease that can develop for years without symptoms. If symptoms appear, it means that the disease is progressing and can at any time lead to complications that could cost you your life.
Therefore, do not delay your visit to the doctor. Make an appointment now.
Atherosclerosis of the aorta: complications
As a rule, complications with aortic atherosclerosis develop if the disease is left untreated for years or treated incorrectly.
- Intestinal gangrene, which occurs when blood access through the mesenteric artery is cut off: manifests itself as severe abdominal pain, tension in the abdominal muscles, and increasing intoxication
- Thrombosis of the superior mesenteric artery - profuse vomiting and profuse feces
- Thrombosis of the inferior mesenteric artery – intestinal obstruction and rectal bleeding
- Gangrene of the legs due to thrombosis of the femoral artery
- Thoracic or abdominal aneurysm - acute bleeding that can quickly lead to death
And a number of other life-threatening complications that can lead to death.
What changes occur in the vessel when it is compacted?
The aorta is an elastic type vessel, that is, its wall contains a large number of connective tissue fibers. She needs this to perform two main functions. Firstly, it stretches quite well, which allows you to maintain diastolic pressure.
It is because of the distensibility of the aorta that blood flows not in spurts, but in a continuous stream, which allows blood to be supplied to the internal organs. This is especially true for the myocardium, which is 85% supplied in the diastole phase.
Secondly, the high content of elastic fibers allows the aorta to withstand the enormous pressure that the blood ejected from the left ventricle exerts on it.
In various diseases, the vessel becomes denser due to the fact that the balance between elastic and collagen fibers shifts towards the latter. Also, in some pathologies, calcium begins to actively deposit in the aortic wall, making it hard.
When the aorta becomes sclerotic, its distensibility decreases, and therefore its ability to maintain diastolic blood pressure at the proper level. This leads to deterioration of blood circulation in internal organs, especially the heart. To correct this, the body has to compensatoryly increase systolic blood pressure through tachycardia and increased peripheral vascular resistance.
The result of such a chain of pathological reactions is the development of so-called isolated systolic arterial hypertension, or the aggravation of existing hypertension.
Due to the poor elasticity of the aorta, the “water hammer” of the blood is not softened, its gradual expansion (dilatation) occurs, and the risk of an aneurysm increases, which can rupture at any time and lead to death.
Atherosclerosis of the aorta: risk factors
There are many factors influencing the development of atherosclerosis. Let's talk about the main ones.
Factors that cannot be eliminated:
- Age. The older you get, the higher your risk of developing atherosclerosis of the aorta. If you are over 50, diagnosis is vital – even if there are no symptoms
- Floor. Men suffer from atherosclerosis in general and atherosclerosis of the aorta 4 times more often than women. After 55 years, the risk of the disease in both sexes is equalized, since in women the level of sex hormones - estrogens, which, according to scientists, has a beneficial effect on the condition and functioning of blood vessels, decreases
- Heredity. If one of your close relatives has had or is suffering from aortic atherosclerosis, your risk of developing this disease is much higher
Avoidable factors:
- Smoking and alcohol. Nicotine and other harmful substances contained in tobacco smoke, as well as alcohol, provoke vascular spasms, which increases the risk of narrowing the lumen significantly.
- Poor nutrition. If your diet contains too much animal fat, your risk of developing atherosclerosis is higher, as it accelerates atherosclerotic changes in blood vessels.
- Sedentary lifestyle. It provokes fat imbalance, which is one of the main causes of cholesterol deposits on the walls of blood vessels.
Partially avoidable factors:
- Arterial hypertension. High blood pressure increases damage to the vascular wall, followed by the deposition of cholesterol in it and the formation of atherosclerotic plaques
- Dyslipidemia. Impaired fat metabolism is accompanied by an increase in the level of low and very low density lipoproteins (“bad cholesterol”), which accelerates the development of atherosclerosis
- Diabetes and obesity. If you are obese or diabetic, or worse, both, your risk of developing arteriosclerosis is 5-7 times higher
- Intoxication, infections. Toxic substances and infections damage the walls of blood vessels, which accelerates the development of atherosclerotic changes
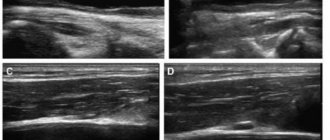
Atherosclerosis of the aorta: diagnosis
Diagnosis begins with a consultation. Our specialist will spend as much time as necessary for you to collect all the necessary information: what exactly are you complaining about, whether you have concomitant diseases, whether any of your close relatives have suffered or are suffering from atherosclerosis or other diseases of the cardiovascular system. A general examination, which the doctor will conduct at the appointment, will help to identify or exclude various signs of atherosclerotic vascular damage, for example, edema, trophic ulcers, weight loss or gain and a number of other signs. Auscultation (listening) of the vessels of the heart and aorta will help to identify or exclude murmurs, disturbances in arterial pulsation and other indicators. A blood test will help determine the level of cholesterol, low-density lipoproteins, and triglycerides. Doppler ultrasound will reveal signs of aortic atherosclerosis: its thickening, expansion in the abdominal or thoracic regions, aneurysms, calcification. Ultrasound scanning of the renal vessels will reveal or exclude the presence of plaques in the renal arteries. Ultrasound scanning of the vessels of the lower extremities, aorta, and carotid arteries will help determine how much the main blood flow in them is reduced, as well as identify atheromatous plaques and blood clots in the lumens of the vessels. If necessary, your doctor will refer you for a coronary angiography, which will help accurately assess the condition of the coronary arteries. Please note: only such a comprehensive diagnosis will help make an accurate diagnosis, assess the extent of vascular damage and select the optimal treatment that will really help you. Make an appointment now.
How to determine pathology
To suspect aortic thickening, it is important to listen carefully to the patient's complaints. To determine the possible cause, I ask in detail when the symptoms appeared, whether the body temperature is rising, whether the joints hurt, whether everything is in order with digestion, with stool, whether the patient has lost weight recently, etc. It is important that the person remembers not whether he suffered from rheumatism in childhood, whether he was registered with a dermatovenerologist for syphilis.
Next I move on to a general inspection. With diseases of the aorta, sometimes I can feel increased pulsation or trembling of the chest. The auscultation method is very helpful. With a stethoscope, I often hear murmurs on the aortic valve or in the jugular fossa (the small depression between the two collarbones). It is imperative to measure blood pressure in both arms: in some pathologies (Takayasu's disease), the readings can be very different.
After this, I schedule an additional examination. First, a blood test is taken to check cholesterol and glucose levels. Then instrumental diagnostic methods are carried out:
- X-ray is often a low-informative method of research. You can only see a pronounced deformation or aneurysm.
- Echocardiography (ultrasound of the heart) is an excellent diagnostic test, especially if the patient has aortic valve (AV) defects. Damage, calcification of the valve leaflets, regurgitation (backflow of blood), narrowing of the openings, expansion of the root and thickening of the walls are detected.
- Computed tomography allows you to make a three-dimensional (3D) reconstruction of the entire aorta and evaluate its condition at any site.
- Aortography is visualization of the largest artery by injecting a contrast agent directly into the vessel, which is very informative. In addition to the structure, it is possible to assess the patency of the aorta, identify aneurysms and mural thrombi along its entire length.
A disability group for aortic atherosclerosis is not established.
An example of aortography. The arrow indicates a saccular protrusion (aneurysm)
Drug treatment of aortic atherosclerosis
Drug treatment of aortic atherosclerosis includes several groups of drugs. Let's discuss the main ones.
- Nicotinic acid and its derivatives Reduce the level of triglycerides and cholesterol in the blood. They increase the level of high-density lipoproteins, which have antiatherogenic properties. Contraindicated for liver disease: if you have any, your doctor will select another medicine.
- Fibrates (miscleron, gevilan, atromide) Reduce the synthesis of your own fats, but can adversely affect liver function and provoke cholelithiasis. Statins (Zocor, Mevacor, Liprimar) Reduce the amount of “bad” cholesterol produced by the liver and, as a result, reduce its level in the blood. Statins are taken at night because cholesterol is synthesized, as a rule, at night.
- Bile acid sequestrants (cholestide, cholestyramine) Bind and remove bile acids, reduce the level of cholesterol and fats in the body. May cause constipation and flatulence.
Treatment methods
I strongly recommend that all patients with atherosclerotic lesions of the aorta quit smoking if such a problem exists. It is important to change your diet by increasing the amount of fish, vegetables and fruits and reducing the amount of fatty meat, lard, and butter. Patients suffering from diabetes need to significantly limit the amount of carbohydrates consumed and control blood glucose levels.
Medicines: what and for how long
Depending on what caused aortic sclerosis, I use different medications:
- Treatment of atherosclerosis requires reducing the concentration of cholesterol in the blood with the help of statins (Rosuvastatin, Atorvastatin). In order to reduce the risk of thrombosis, I prescribe antiplatelet agents (Acetylsalicylic acid, Clopidogrel).
- Infectious diseases may be a reason to prescribe antibiotics. For syphilis - Penicillin, for brucellosis - Doxycycline. Tuberculosis requires the use of special anti-tuberculosis drugs - Isoniazid, Ethambutol.
- Rheumatological diseases and systemic vasculitis. In the case of autoimmune pathologies, to suppress severe inflammation in the aortic wall, I use glucocorticosteroids (Methylprednisolone) or more powerful immunosuppressants (Cyclophosphamide, Methotrexate).
I would like to note that, regardless of the cause of aortic sclerosis, I prescribe antihypertensive medications for high blood pressure:
- for isolated systolic arterial hypertension (high pulse pressure) - calcium channel blockers (Amlodipine) or diuretics (Indapamide, Hydrochlorothiazide);
- in the presence of CHF - ACE inhibitors (Perindopril, Ramipril) or sartans (Losartan, Valsartan);
- in the presence of coronary heart disease - beta-blockers (Metoprolol, Bisoprolol).
Surgical interventions
Surgical treatment methods are used only when an aneurysm has developed. This is necessary to prevent its further growth and its worst consequence - rupture.
The operation is indicated if the aortic diameter exceeds 55 mm.
There are 2 methods of surgical treatment of aortic aneurysm:
- Installation of a stent graft (a metal wire cylinder), which allows to level blood pressure on the weakened walls of the aneurysm, thereby preventing its rupture. The operation is performed under local or general anesthesia. The device is inserted through the femoral vessel and, under X-ray control, reaches the affected area.
- Prosthetics with a conduit (a special tube made of pericardial tissue or synthetic material). When replacing the root and ascending portion, the aortic valve is often also replaced. The operation is performed under general anesthesia on an open chest.
Are folk remedies effective?
On the Internet, by searching “folk remedies for treatment of atherosclerosis of the aorta of the heart,” you can find a lot of alternative medicine recipes that promise not only an improvement in the patient’s condition, but also a complete cleansing of all the vessels of the body. Unfortunately, none of them has an evidence base. Their use, at best, will be simply useless, and at worst, harmful and even life-threatening.
Many components of herbs can interact with medications prescribed by a doctor (for hypertension, to lower blood cholesterol, etc.). This leads to the fact that either the therapeutic effect of the drug will worsen, or the likelihood of adverse reactions, sometimes very severe, will increase.
Surgical treatment of aortic atherosclerosis
Surgeries are prescribed when drug therapy does not help. Our specialists will determine how much surgery you need and which method of surgical intervention will be effective in your case. Possible methods may include:
- Stenting The surgeon will install a special stent into the lumen of the vessels, which will expand the narrowed area and ensure free blood flow
- Bypass surgery The surgeon will install a shunt to bypass the narrowed area, as a result of which blood flow through the affected vessel will be restored
- Plastic surgery of a segment of the aorta or its branches with an endoprosthesis
Atherosclerosis of the aorta: prevention
Proper prevention is one of the key conditions for successful recovery, which cannot be neglected:
- Stop smoking and drinking alcohol
- Avoid foods and dishes containing animal fats
- Treat concomitant diseases in a timely manner if you have them: diabetes mellitus, arterial hypertension, obesity
- Lead an active lifestyle, move more, play sports, but do not overwork your body
- Don't be nervous about trifles
- Cure infectious diseases in a timely manner
- Get annual checkups and examinations, especially if you are over 40 years old
Diet for atherosclerosis of the aorta
Despite the fact that the proportion of cholesterol that we get from food is not very large (up to 25%), proper nutrition in combination with the right treatment and a healthy lifestyle will significantly increase the effectiveness of treatment.
Products we recommend excluding:
- Sour cream
- Mayonnaise
- Sauces
- Chips
- Salted nuts
- Cocoa and chocolate
- White butter bread
- Baked goods, biscuits, cakes, pastries
- Butter and sour creams
- Puddings and ice cream
- Cheese, margarine, dairy products
- Whole milk
- Coconut and palm oil
- Suet
- Butter, animal fats
- Pates, hams, smoked sausages
- Fat duck or goose
- By-products (brains, kidneys, liver)
- Fatty meat (pork, lamb, beef)
Foods that will help lower cholesterol levels:
- Green salads
- Garlic
- Onion
- Dill
- Parsley
- Legumes
- Fruits
- Lean meat
- Shellfish
- Wholemeal flour
- Oat groats
- Bran
- Fatty sea fish (herring, mackerel, sardines, salmon, tuna)
- Vegetable oils
Remember: the earlier aortic atherosclerosis is detected, the higher the chance of stopping the progression of this disease and preventing life-threatening complications. Therefore, do not delay your visit to the doctor. Make an appointment now.