Atherosclerosis is characterized by impaired hemodynamics (blood movement) in the arteries due to narrowing of the vascular bed. The disease affects the cerebral vessels of the brain, carotid and coronary arteries, thoracic aorta, vessels of the lower extremities and kidneys.
Atherosclerosis of the coronary arteries develops in the main vessels that supply blood and, accordingly, oxygen to the heart muscle. Deficiency of blood supply is the key cause of the development of coronary heart disease (CHD), which threatens necrosis of the myocardium (infarction) and sudden cardiac arrest.
The left and right coronary (otherwise, coronary) arteries bear the main functional load in the vascular system, ensuring the smooth functioning of the heart. They are the only source of oxygenated arterial blood supply to the myocardium.
The coronary arteries arise from the root of the main vessel of the systemic circulation (aorta) and have a complex pattern of branches into capillaries and other small vessels. The right artery is responsible for delivering blood to the right ventricle (heart chamber) and the posterior wall of the left ventricle. The left coronary vessel is the source of blood supply to the rest of the heart.
Symptoms
Signs of atherosclerosis do not appear immediately. The first stages of atherosclerosis of the heart vessels are asymptomatic. The disease makes itself felt when the coronary artery becomes so blocked that it no longer supplies the heart with enough blood. A blood clot can completely block blood flow, causing a heart attack.
The main sign of severe atherosclerosis is burning or pressing pain in the chest, which initially bothers you during physical activity or in a stressful situation. This syndrome is called cardiac angina. Pain can be felt behind the sternum, radiating to the left arm, shoulder girdle and jaw. In addition to the feeling of constriction, a person is worried about shortness of breath, weakness, and excessive sweating. All these are signs of coronary heart disease (CHD). The nature of the load under which attacks occur varies. At later stages of development of coronary artery disease, the pain syndrome is no longer determined by any reasons; in this case, they speak of a type of angina called resting angina.
Treatment
Depending on the intensity of symptoms, the nature and scale of atherosclerotic changes in the arteries, conservative methods and surgical intervention are chosen (combined). When the diagnosis of coronary atherosclerosis is confirmed, it is necessary to immediately abandon nicotine and alcohol, as the main causes of damage to the intima of the vessel.
Conservative therapy
The use of medications to treat atherosclerotic changes in the coronary arteries is effective only in the initial stage of the disease. Groups of prescribed drugs:
- Statins. Designed to eliminate hypercholesterolemia by inhibiting the natural synthesis of cholesterol in the liver.
- Calcium channel blockers and agnioprotectors. They increase the tone of blood vessels and smooth muscles, strengthen the intima, and increase the elasticity of the arteries.
- Fibrates. Low and very low density lipoproteins are broken down and removed.
- Anticoagulants. Normalize blood clotting indicators.
- Bile acid sequitrants. Causes the liver to use excess LDL to produce bile.
At the same time, medications are prescribed to stabilize blood pressure, metabolic processes, and cardiac activity.
Diet therapy
Compliance with the special diet “Table No. 10” (according to the medical classification of V. Pevzner) is a prerequisite for both conservative and surgical treatment of atherosclerosis of any form. General rules for catering:
- control over the number of calories and the ratio of nutrients in dishes and products;
- adherence to a meal plan (every 3-4 hours in small portions);
- eliminating prohibited foods from the menu and introducing into the daily diet foods that help reduce blood cholesterol;
- refusal of dishes prepared by the culinary method of frying.
Product classification
As an additional therapy, traditional medicine is used that helps cleanse blood vessels from cholesterol (garlic, flaxseed oil, ginger, etc.).
Surgery for coronary atherosclerosis
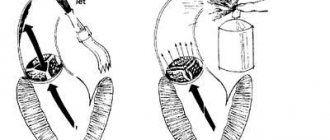
To restore hemodynamics, modern surgical methods are used - balloon angioplasty in combination with stenting and coronary artery bypass grafting.
Surgical options
| Operation and Parameters | Balloon angioplasty with stenting (otherwise known as percutaneous transluminal coronary angioplasty) | Coronary artery bypass grafting (or CABG surgery) |
| Methodology | Endovascular X-ray surgery | Strip plastic modeling surgery |
| Performance technique | Through a tiny incision in the femoral artery, a thin catheter is inserted into the patient, equipped with a balloon, inside of which a special stent is located. Gradually moves towards the aorta and coronary arteries. Under X-ray control, the balloon is placed on the deformed area of the vessel and inflated. The stent adheres to the vascular walls, flattening the plaque. Blood flow is restored | Creation of an additional channel using a shunt (transplant) for cardiac blood flow, bypassing the area blocked by plaque (one end of the shunt is sewn into the coronary artery, below the affected area, the other directly into the aortic wall) |
| Statistics of postoperative relapses (probability of restenosis) | Up to 40% within 1-1.5 years | Up to 30% for 5 years |
| Rehabilitation period | 1-2 days in hospital, a week - outpatient | Hospitalization 7-10 days, followed by recovery at home |
| Contraindications | Bleeding disorders, allergic reactions to radiocontrast agents, pregnancy | Oncological diseases |
With a parallel aortic aneurysm, conservative treatment is not advisable. The patient requires surgery to bypass the main vessel or resection of part of the aorta with prosthetics.
Research and diagnostics
If you notice symptoms of atherosclerosis or in case of a hereditary predisposition, we recommend making an appointment with a cardiologist for a consultation and checking your blood cholesterol levels. Depending on the results of the examination, the doctor prescribes the following diagnostic tests:
- Lab tests. The patient will be asked to take a blood test to check their sugar and cholesterol levels. 9-12 hours before the procedure, do not eat or drink anything (except water).
- ECG. The examination helps to identify abnormalities in the functioning of the heart and previous heart attacks. If you complain of pain during physical activity, your doctor will prescribe a stress electrocardiogram (bicycle ergometry and treadmill test).
- Stress test. This is monitoring of heart function during physical activity, which is exercise on an exercise bike or walking on a treadmill. While you exercise, your doctor will take readings of your blood pressure and heart rate. If it is not possible to take the test in a standard way, you will be tested using a special medication, the effect of which simulates physical stress on the heart.
- Coronary angiography. With the help of this examination, it is possible to understand which coronary vessels are affected by atherosclerosis. The doctor injects a contrast agent through a catheter passed through an artery in the leg or arm to the heart. While the vessels are filled with it, the X-ray unit operates. An image of the coronary arteries is displayed on the monitor, and the specialist marks the affected areas. Watch the video of coronary angiography by following the link.
- Additional research. Your doctor will recommend a CT or MRI scan, as well as an ultrasound, to determine if you have an aneurysm and calcium deposits in your arterial walls.
Development mechanism
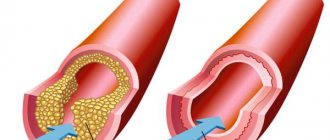
Pathological changes in blood flow in atherosclerosis of the coronary arteries are caused by deposits on the intima (inner surface of the vascular walls) of “bad” cholesterol, otherwise low and very low density lipoproteins (LDL and VLDL).
Cholesterol is one of the most important elements in the body. This is a lipophilic alcohol that is involved in the synthesis of hormones, maintaining interneuronal connections in the brain and spinal cord, fat metabolism and the absorption of vitamin D. About 20% of cholesterol enters the body with food, the rest is produced by hepatocytes (liver cells).
The combination of cholesterol with blood proteins forms lipoproteins:
- low and very low density - move endogenous fats from the liver through the bloodstream into the cells and tissues of the body;
- high density (HDL) – cleanse blood vessels from excess LDL and VLDL and deliver them to hepatocytes for further utilization.
High cholesterol levels (hypercholesterolemia) indicate an imbalance of lipoproteins of different densities - an increase in LDL and a decrease in HDL. Excess “bad” cholesterol settles on the walls of blood vessels, “caught” on microcracks in the intima.
Anatomical features of the coronary vessels
Cholesterol plaques form, which grow and harden over time, partially blocking blood flow. When the lumen of the coronary arteries narrows (stenosis), the heart does not receive the required volume of blood. Complete blocking of a vessel by an atherosclerotic plaque leads to cardiac arrest.
Reference! Intravascular growths (plaques) are not only “bad” cholesterol. They contain connective fibers, calcium salts, platelets and other blood cells.
Coronary atherosclerosis progresses slowly. From the moment of the first cholesterol deposits to the appearance of symptoms of the disease, more than a dozen years can pass. The main group of patients with primary manifestations of atherosclerosis are people aged 45+.
In elderly patients, atherosclerosis of the aorta and coronary arteries is often diagnosed simultaneously. Aneurysm of the thoracic aorta (expansion or stretching of its wall) is potentially dangerous due to the sudden rupture of the central vessel and the instant death of a person.
Treatment of atherosclerosis of heart vessels
The method of treating atherosclerosis of the heart vessels depends on the degree of vascular damage and the risks that the disease poses in each specific case. Often, to stop the development of the disease, it is enough to give up bad habits, start eating right and doing regular exercise. It is possible that medication or surgery will be needed.
Atherosclerosis is fought with:
- Cholesterol-lowering drugs. For example, fibrates and statins. They reduce the level of “bad” cholesterol—low-density lipoproteins—and increase “good” cholesterol—high-density lipoproteins. As a result, the process of fat accumulation in the arteries stops.
- Antiplatelet substances. For example, aspirin. It prevents platelets from sticking together in affected arteries, reducing the likelihood of blood clots forming.
- Beta blockers. Usually prescribed for the treatment of cardiac ischemia and angina. They weaken the pulse rate and lower blood pressure, thereby reducing cardiac stress and chest pain. Beta blockers minimize the risk of heart attack and heart rhythm problems. Read about what other medications are used to treat angina here.
- ACE inhibitors. Angiotensin-converting enzyme inhibitors reduce blood pressure and have a positive effect on the arteries of the heart, as a result of which the development of atherosclerosis stops and the risk of a recurrence of a heart attack is reduced.
- Calcium channel blockers - lower blood pressure.
- Diuretics. Diuretics fight high blood pressure.
If you have underlying medical conditions that increase your risk of developing atherosclerosis (for example, diabetes), your doctor will prescribe additional medications.
Ischemic (coronary) heart disease
In many countries of the world, coronary heart disease is called coronary heart disease - these are synonyms (ischemic or coronary heart disease). The coronary arteries arise from the aorta and carry oxygenated blood to the heart muscle.
ISCHEMIA is a condition when sufficient oxygenated blood does not flow to the heart muscle.
ANGINA - discomfort, pressure, pain or heaviness in the chest. It can radiate to the neck, arms, back. The cause of angina pectoris is most often ischemia.
Pain with angina pectoris has characteristic distinctive signs:
- Lasts several minutes (usually no more than 10)
- It is most often localized behind the sternum. Sometimes it can be in the left half of the chest and radiate to the left arm, shoulder, jaw, and stomach.
- The pain intensifies during physical activity, walking, emotional stress, after eating or when going out into the cold.
- Pain is alleviated or eliminated (relieved) by stopping exercise, resting, or taking specific medications such as nitroglycerin.
MYOCARDIAL INFARCTION can begin with such pain . If you experience at least some of the symptoms described, contact your cardiologist to discuss them.
If you have ANGINA , you should immediately do the following:
- Stop walking or any other activity you were doing during this time.
- Place a nitroglycerin tablet under your tongue. It should dissolve there. Instead of a tablet, you can use a form of nitroglycerin called SPREY. It must also be inhaled under the tongue. Wait 5 minutes.
- If you still have symptoms of angina, use a second nitroglycerin tablet or a second dose of nitrate spray. Wait another 5 minutes.
- If you have angina for more than 20 minutes and/or after taking 2 nitroglycerin tablets, CALL AMBULANCE IMMEDIATELY.
Under no circumstances should you drive yourself if you have angina. Even if you go to the doctor. Call an ambulance. The arriving doctor will begin to provide assistance to you at your home. Under no circumstances should you delay calling an ambulance if you yourself have not been able to eliminate the symptoms of angina.
How is MYOCARDIAL INFARCTION diagnosed?
Diagnostics begins immediately upon the arrival of the ambulance. First, the doctor will ask you about your symptoms, examine you and perform instrumental diagnostics.
1. Electrocardiogram. It helps to determine the depth of damage to the heart muscle, where this damage is located, which will determine the nature of the heart rhythm and the presence of arrhythmia.
2. Blood tests. The level of biochemical markers in the blood will be determined. They are called blood enzymes or enzymes. When heart muscle cells are damaged, enzymes are released into the blood. Their level in the blood increases sharply, sometimes several times. By determining this level, the doctor can judge the size of the myocardial infarction and approximately when it began. Carrying out other blood tests also provides additional information about the extent and timing of damage to the heart muscle and helps select adequate treatment.
Diagnosis of myocardial infarction is based on:
- Your symptoms; — ECG; — Blood test results.
How is myocardial infarction treated?
Interventional procedures in the treatment of myocardial infarction
Soon after admission to the hospital, you will be sent to the angiography laboratory. ANGIOGRAPHY is a test that shows the presence and extent of narrowing of your blood vessels by atherosclerotic plaques. At the same time as the condition of the coronary vessels is determined, you may receive treatment to open the narrowed or blocked artery. This procedure is called an interventional procedure or angioplasty.
Angioplasty includes 2 types of treatment – BALLONGING and STENTING. These are types of treatment when a balloon is placed at the site of narrowing in the coronary artery, which is subsequently inflated and thus expands the narrowed site of the vessel. This procedure is called ballooning. A stent is a small spring that keeps the vessel open. This procedure is called stenting.
Surgical treatment of coronary vessels - bypass surgery
If there are indications, cardiac surgery can be performed to restore blood flow through your coronary vessels - bypass surgery. This operation is performed in special surgical departments. The indication for it is a significant narrowing of 3 or more vessels or the main trunk of the left coronary artery.
Taking medications
Before leaving the hospital you must clearly understand:
- Name of all your medications
- What purpose do they serve?
- How often should they be taken?
- What side effects may there be?
Medicines that are prescribed after a myocardial infarction include:
- Antiplatelet agents (aspirin, clopidogrel, ticogrelol, prasugrel) are drugs to prevent future blood clots.
- Medicines that can: • reduce heart rate • lower blood pressure • eliminate angina • treat heart failure • lower blood cholesterol levels
Some medications may be prescribed for you for a short time, some for life.
Before discharge, your doctor will give you a statement that will tell you what medications, in what dose and for how long to take.
After a heart attack, your goal should be to maintain your health at an acceptable level and eliminate risk factors that could lead to heart problems in the future.
To prevent or reduce possible cardiac problems, follow these rules:
- Take prescribed medications
- Change your lifestyle
- Visit your cardiologist regularly
Surgery
If there is significant damage to the arteries of the heart, the doctor prescribes surgery. Interventions are performed as planned, and in acute coronary insufficiency and in the early stages of a heart attack, emergency surgery helps save lives.
Bypass surgery is an open operation that is performed using a synthetic prosthesis or other vessel that will allow blood flow to bypass the affected area.
Coronary angioplasty and stenting is an endovascular intervention that is performed under local anesthesia without incisions. The operation is minimally traumatic for the patient. The doctor inserts the first catheter through a puncture in a vessel of the leg or arm into the artery with an atherosclerotic plaque, and inserts the second, with a balloon at the end, into the narrowing of the coronary artery. The catheter with the balloon inflates and leads to an increase in the lumen. The surgeon installs a stent in the narrowed segment, which will maintain the artery in an open state.
Diagnostics
The basis for diagnosing coronary atherosclerosis is the hardware research protocol. The patient receives a referral for an extended examination upon presentation of symptomatic complaints characteristic of IHD, based on the results of a general lipid profile (cholesterol, low- and high-density lipoproteins, triglycerides) and a biochemical blood test.
The list of diagnostic procedures that can determine atherosclerosis of the coronary vessels includes:
- Echocardiography. Ultrasound examination of the heart. It is carried out in the following ways: transthoracic (with an external sensor), transesophageal (a tubular sensor is inserted into the esophagus), intravascular (insertion of a sensor through peripheral arteries into the cardiac cavities and large vessels), stress cardiography (a study with pharmacological or physical stress).
- Echo-Dopplercardiography. Assessment of the work and condition of blood vessels, the speed of blood circulation in the coronary arteries, aorta and other vessels of the organ.
- 2D scintigraphy. Methods of radionuclide diagnostics for the study of pathological processes occurring at the molecular and cellular level. It is carried out in two stages: pictures at rest (regular study), pictures with natural or artificial physical activity (training on a cardio stepper or cycling).
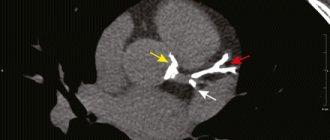
- Tomography (multispiral computed tomography and magnetic resonance imaging). The first visualizes atherosclerotic growths (shape, size, structure), the second evaluates vascular damage.
Hardware tests are selected individually, taking into account contraindications, hospital equipment, and the complexity of a particular case of illness. The most informative and accessible method is coronary angiography - x-ray of the coronary vessels with a radiopaque substance.
The procedure is minimally invasive and involves inserting a catheter into the patient's femoral or brachial artery and injecting contrast. X-rays are taken separately for the left and right coronary arteries.
How do lifestyle changes slow or prevent the development of atherosclerosis?
- To give up smoking. By getting rid of a bad habit, you will significantly reduce the likelihood of atherosclerosis.
- Regular physical activity. Daily physical exercise as part of the prevention of coronary heart disease will improve blood circulation, develop new blood vessels (collaterals) that form blood flow bypassing the affected area, and allow muscles to use oxygen more efficiently. In addition, you will get rid of high blood pressure and minimize the risk of developing diabetes. Exercise 30-60 minutes a day at least 4-5 times a week. The simplest effective physical activities: squats, push-ups and walking.
- Healthy eating. Follow a diet aimed at maintaining cardiovascular health.
- Weight control. Monitor your weight and maintain it at normal levels. If you are prone to obesity, losing 2-5 kg will reduce the risks of developing hypertension, diabetes and coronary artery disease.
If you suffer from hypertension, diabetes, high blood cholesterol or other chronic diseases, regularly undergo preventive examinations at the cardiology center and see a doctor: he will help normalize your health and avoid the development of serious illnesses.
Causes
An increase in cholesterol levels is the result of a malfunction of lipid metabolism in the body, provoked by the negative impact of the following factors:
- gastronomic addictions to fatty foods and sweets;
- hypodynamic lifestyle;
- diabetes;
- obesity;
- prolonged neuropsychological stress;
- chronic pathologies of the hepatobiliary system (liver and gallbladder);
- impaired absorption of nutrients and nutrients in the intestine (malabsorption).
Reference values for total cholesterol in the blood are 3.2-5.2 mmol/l (for adults). Hypercholesterolemia is considered to be > 7.7 mmol/l. The formation of cholesterol growths inside the vascular walls occurs when two factors are correlated: excess LDL (VLDL) and the presence of intimal microdamages.
Blood elements responsible for intimal protection and coagulation (platelets) accumulate in the injured area and attract “bad” cholesterol (LDL has the same charge as platelets). Causes of microcracks in the intima:
- nicotine addiction and alcohol abuse;
- incorrect therapy with certain types of medications;
- chronic blood diseases and hormonal pathologies associated with blood disorders;
- hypertonic disease.
Fragility of blood vessels occurs due to hypovitaminosis of vitamins B, C, D, E. By gender, atherosclerosis of the coronary vessels is more common in men. In women, the disease is diagnosed during menopause, when the production of sex hormones that protect the vascular walls during fertile age ceases.
Atherosclerosis of the coronary vessels - causes, symptoms, treatment
Vascular atherosclerosis is a systemic lesion of large arteries that occurs as a result of disturbances in lipid and protein metabolism. The condition is accompanied by the proliferation of fibrous tissue, the deposition of cholesterol plaques and a suspension of lipoproteins in the lumen of blood vessels, which leads to their sclerosis and calcification. The narrowing arterial lumen prevents normal blood supply to tissues and provokes damage to internal organs. There are atherosclerosis of coronary and renal vessels, vessels of the lower extremities, brain, abdominal aorta.