Blood pressure indicators are considered the main ones in determining the quality of the cardiovascular system as a whole. Heart rate is equally assessed. With a more in-depth analysis, the doctor is able to characterize the patient’s general health condition and predict risks.
Blood pressure 160/90 mm Hg. Art. in adults this is a borderline indicator. It is certainly considered pathological, since the norm is set at 139 to 89, this is the possible maximum. The question is to determine the degree of development of the process.
In this case we are talking about the second stage of hypertension. Although diastolic (lower) values in the range of 100-110 are typical for it, the assessment, as a general rule, is based on a higher number. That is, by systolic (upper) pressure.
Arterial hypertension of the second degree is already considered developed: the risks of complications, as well as further progression, are high. The prognosis is serious. The outcome can be discussed taking into account the risk (there are 4 forms of such an indicator).
Treatment is carried out under the supervision of a cardiologist throughout life.
What does it mean
What does it mean when the tonometer shows the numbers 160 to 90? The regular appearance of such indicators indicates the transition of hypertension to the second stage. It is important to remember that for representatives of the older age group, blood pressure is 160/90 mmHg. Art. is an acceptable norm.
But only if the condition is not accompanied by the development of a clinical picture typical of hypertension. The reason is the general aging of the entire body and the vascular system in particular. The walls of the blood vessels become less elastic, which leads to an increase in blood pressure (blood pressure).
Important! Women's blood pressure levels are initially lower than men's. Therefore, blood pressure 160/90 is a sure sign of hypertension.
Home help
An attack of arterial hypertension or an episode of increased pressure is treated with great care. A sharp drop in the tonometer reading can lead to fatal consequences: cardiac arrest, heart attack or stroke.
The algorithm for reducing tonometer readings is as follows:
- Measure blood pressure and heart rate. As the rate increases, the rate of cardiac activity increases. Bradycardia is uncharacteristic and does not occur. Not counting emergency conditions, potentially fatal.
- Open a window or vent to provide fresh air. Excess carbon dioxide in the environment leads to further hypoxia and disruption of cellular respiration. The risk of complications increases.
- Take prescribed medications. If the patient has not yet been to a cardiologist, you can take Capotopril (there are several trade names). This remedy should be in the first aid kit of anyone who is prone to pathologies of the cardiovascular system in general. Quantity - no more than a quarter of a tablet at a time. It is also possible to use a beta blocker (for example, Anaprilin) together. Amount - 25 mg per dose.
- Lie down, calm down. Pay attention to how you feel. If after 30 minutes there is no effect, or even worse, call an ambulance.
Attention:
The use of baths, folk recipes, contrast showers, heating pads, and water procedures is generally strictly prohibited. Such amateur activity will result in at least a hypertensive crisis, and at maximum a dangerous condition with the prospect of death in the short term.
You can reduce the pressure of 160 to 90 on your own, the question is feasibility and safety. Emergency antihypertensive drugs are used. Beta blockers as needed.
Normal or pathological?
Blood pressure 160/90 mm Hg. Art. Is it the norm or a deviation? Most often, this level of blood pressure is considered by doctors as a pathology and indicates the development of the second degree of hypertension. The condition in this case is accompanied by characteristic symptoms and requires drug treatment.
Sometimes this blood pressure may be normal. This indicator can occur in men over 40 years of age or people with a large physique and tall stature. At the same time, there are no unpleasant manifestations characteristic of hypertension.
Diagnostics
The examination is carried out under the supervision of a group of specialists. The first is a cardiologist. As necessary (to study the origin of arterial hypertension).
List of activities in correct order:
- Oral questioning of the patient and collection of anamnesis. First of all.
- Measurement of pressure and heart rate.
- 24-hour Holter monitoring. The main indicators are recorded for 24 hours. Considered the gold standard, although little is known about etiology.
- Electrocardiography. Assessment of functional deviations. Variants of arrhythmias are possible, from typical sinus tachycardia to ventricular extrasystoles and others.
- Echocardiography. Visual technique. Aimed at identifying organic pathologies and defects. The classic sign of advanced hypertension is left ventricular hypertrophy.
- Load tests. Carefully.
Advanced diagnostics includes blood tests (general, biochemistry, hormones), urine (clinical, according to Zimnitsky).
Also assessment of the neurological status using routine methods, electroencephalography, MRI of the brain (rarely), scintigraphy of the liver, kidneys, and thyroid gland. It is possible to prescribe FVD and X-ray of pulmonary structures.
Possible reasons
There are a number of factors that provoke a significant increase in blood pressure levels.
Physiological
They are relatively rare. The person does not have any symptoms. Although short-term dizziness or increased heart rate may occur. The reasons may be:
- Puberty. The body of a teenager during the period of growing up - from approximately 12 to 19 years - undergoes powerful hormonal changes, which can provoke a significant increase in blood pressure. Hypertension in this case is secondary in nature and goes away after the root cause is eliminated. Isolated episodes of high blood pressure occur in most young people. Despite the natural causes of pressure surges - changes in hormonal levels - a teenager should be observed by a cardiologist.
- Pregnancy. In rare cases, blood pressure 160/90 is a variant of the physiological norm. But most often, an increase in pressure to such high levels indicates the development of late toxicosis.
- Stressful situation. The reason for the jump is the release of a large amount of hormones into the blood - adrenaline and cortisone. They cause vasoconstriction and stimulate the central nervous system.
- Increased physical activity. Typical for athletes and people whose work involves lifting heavy weights.
- Abuse of drinks containing caffeine. They provoke an increase in the tone of the walls of blood vessels, which causes a sharp jump in pressure. The effect can last two to three hours.
- Drinking large amounts of alcohol. The drink has two opposite effects. Initially, it dilates blood vessels, which causes a decrease in blood pressure. After 10–15 minutes, the vascular lumens, on the contrary, narrow. This causes an increase in blood pressure and an increase in heart rate.
- Smoking. Nicotine also has a very negative effect on the condition of blood vessels, causing not only a persistent increase in blood pressure, but also heart disease and atherosclerosis of the veins of the lower extremities.
- Oral contraception. Drugs in this group can cause persistent hormonal imbalances and, as a result, an increase in blood pressure. The condition is reversible as a woman can correct her condition on her own. Therefore, surges in blood pressure do not always result in the development of hypertension.
Pathological (heart)
The reasons in this case may be:
Diet for arterial hypertension
- Atherosclerosis of large vessels. Persistent increase in blood pressure to 160/90 mm Hg. Art. occurs against the background of complete/partial blockage of the lumen or its stenosis (narrowing). If left untreated, the condition leads to vascular obstruction.
- Heart defects (congenital/acquired). In most cases, this is valve insufficiency, dysfunction of the septum. Therapy is possible only surgically and consists of restoring normal heart function and lowering blood pressure levels.
- Diseases of the heart and pericardium of an inflammatory nature. They cause destruction of cardinal structures or accumulation of fluid and subsequent compression. The patient needs urgent hospitalization. Treatment is with antibiotics, corticosteroids, etc.
- Rheumatism, diseases of autoimmune origin.
- Heart attack or stroke. Pathologies are accompanied by impaired nutrition of myocardial or cerebral tissue (in case of stroke). Increased blood pressure is a symptomatic manifestation that lasts up to six months. Treatment is carried out with antihypertensive drugs.
Pathological (non-cardiac)
An increase in blood pressure to 160/90 can also be provoked by:
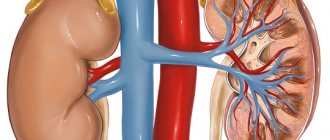
- Kidney diseases, in particular, renal failure (acute, chronic, in the stage of decompensation). Treatment should be carried out by a nephrologist.
- Liver failure. The reason for the increase in blood pressure is organic changes in organ tissue. Most often it is hepatitis or cirrhosis. More rarely, the provoking factor is oncopathology.
- Endocrine disorders – hyperthyroidism (overactivity of the thyroid gland), active production of the hormone cortisol by the adrenal cortex.
- Injuries, neurogenic conditions.
- Hormonal imbalances during gynecological diseases.
Consequences of hypertension
The higher your blood pressure, the harder the work your heart has to do to maintain normal blood circulation. Therefore, if hypertension is not treated, the walls of the heart first thicken or hypertrophy, which increases the risk of the heart working intermittently, and later the walls of the heart become thinner, which leads to disruption of the blood supply to the tissues and the heart itself and is accompanied by the appearance of shortness of breath, fatigue, and swelling in the legs. These signs often indicate the development of heart failure, which is the inability of the heart muscle to perform its normal pumping function.
High blood pressure accelerates a process known as atherosclerosis, which is the formation of fatty deposits on the walls of the arteries, causing them to harden, thicken, and reduce the lumen of the vessels. If the coronary arteries that supply blood to the heart are affected, angina pectoris or angina pectoris develops. As the process progresses, one of the arteries may become completely blocked, then part of the heart muscle stops receiving blood, and myocardial infarction develops. Atherosclerosis can affect any part of the arterial bed. If cerebral vessels are damaged, a patient with hypertension is highly likely to develop a cerebral stroke, which impairs motor abilities, speech and memory. When the blood vessels of the eyes, kidneys and lower extremities are affected, there is a high risk of developing blindness, renal failure and “intermittent claudication”.
Symptoms
Symptoms accompanying an increase in blood pressure to 160/90 mmHg. Art., will be the same for both men and women. Conventionally, they can be divided into two groups: basic and indicating the development of conditions requiring immediate medical attention.
Main manifestations:
- Headache. The main area of localization is the parietal and occipital zone. The pain is intense. Headaches in the second stage of hypertension are almost always constant. The intervals between attacks are very short – sometimes no more than a day. As the body gets used to the new blood pressure, the pain gradually disappears, leaving the patient with only a feeling of heaviness in the head. This significantly complicates the diagnosis of pathology, since the tonometer readings stabilize.
- Dizziness (poor orientation in space). A person experiences it during acute periods.
- Dyspnea. It is a consequence of a violation of the gas exchange process.
- Tachycardia (rapid heartbeat).
- Fainting states. They are rare. As a rule, fainting can occur at the stage of the body “getting used to” a new level of blood pressure or with the development of a hypertensive crisis.
- Noise in the ears, flickering of black flies in the field of vision, split images, etc.
- Feeling nauseous. May end with bouts of vomiting.
When cardinal problems (disturbances in the functioning of the myocardium) occur, the patient develops rhythm disturbances, blue discoloration appears in the area of the nasolabial triangle, and the entire surface of the skin becomes significantly paler. When emergency conditions occur, the symptoms not only intensify, but also get worse. The clinical picture develops very quickly.
A person experiences: an unbearable headache, complete disorientation - the patient cannot navigate in space, discomfort in the chest area - the person experiences a pressing pain that disrupts the breathing process, severe arrhythmia, paresis, paralysis, distortion of facial features.
Impaired vision, speech and hearing occur, dysuria - a person cannot empty the bladder, syncope - a short-term fainting, which is accompanied by impaired muscle tone, a malfunction of the myocardium and respiratory system, and the sensation of goosebumps running across the skin.
Important! If such symptoms develop, the patient must call an ambulance, since treatment should be carried out in a hospital setting.
Age norms of blood pressure: yesterday and today
You may not know, but the European Society of Cardiology has tightened blood pressure standards. The thing is that earlier recommendations “failed” to prevent complications of vascular diseases. And damage to the brain, heart, eyes and kidneys due to hypertension continues to be a serious medical problem. So what “numbers” are recommended by leading experts? And what can “spoil” blood pressure?
What changed
According to previously existing standards, the blood pressure (BP) of a healthy person at rest should not exceed the following values:
- 120/70 – 130/80 – for people aged 20-40 years,
- 140/90 – at the age of 40-60 years,
- and 150/90 for patients over 60 years of age.
New recommendations from European experts (2018) have significantly tightened the standards, and now the blood pressure “figures” should not exceed:
- 129/80 – for people under 65 years of age
- and 139/80 for older patients.
Which, by the way, corresponds to the recommendations of American cardiologists, adopted a year earlier than European ones.
As you can see, the changes concern not only the upper (systolic), but also the lower (diastolic) pressure. This means that the diagnosis of hypertension itself and the initiation of its treatment are now authorized much earlier.
What can spoil blood pressure?
Of course, one of the most significant risk factors for hypertension is heredity and age-related changes.
Thus, cases of vascular pathologies, especially with a disabling outcome in close relatives, are a serious reason to take the vessels under constant “control”.
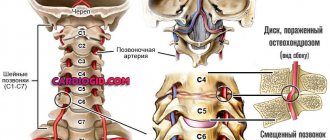
And with “age,” the vascular wall significantly loses its elasticity and ability to expand, because:
- firstly, the synthesis of collagen and elastin fibers decreases,
- and secondly, the thickened walls of blood vessels due to pressure changes (the vasoconstrictive effect of stress hormones, cigarettes and some other factors) do not have the ability to stretch.
So we can say that vascular pathologies have a “cumulative” nature, beginning to form at a young and active age.
In addition, with age, cholesterol deposition and the formation of plaques are observed, narrowing the diameter of blood vessels and further aggravating the problem.
Blood pressure "under control"
Taking into account the above factors, it is obvious that it is better to start paying attention to blood vessels at a young age and regularly.
The presence of regular and/or prolonged stress, smoking, drinking alcohol, a sedentary lifestyle, excess weight and diseases of the kidneys, heart or adrenal glands are reasons to periodically check the degree of damage to the vascular wall. And for this, a blood test for ultrasensitive C-reactive protein is suitable.
The marker reflects vascular damage long before the formation of atherosclerotic plaques and blood clots on the damage, as well as changes on ultrasound and any clinical signs. Therefore, it can be used for the earliest detection of the degree or risk of vascular pathologies.
In addition, it is worth taking control of cholesterol and its fractions, even outside of eating “fatty” foods. After all, lipid levels have a direct relationship with:
- liver health (since this is the place of its formation),
- level of sex hormones,
- overweight,
- as well as diseases that disrupt fat metabolism (diabetes mellitus, lack of “thyroid” hormones and some others),
and cholesterol “balance” disorders can be detected at absolutely any age.
Periodic “jumps” in pressure and the development of arterial hypertension can also be provoked by:
- imbalance of salts (sodium, potassium, chlorine),
- disorders of urinary function of the kidneys
- and excess renin.
And the latter also makes hypertension resistant to standard therapy. And assessment of the renin level is used to exclude the renal nature of the “pressure”.
Treatment
If we talk about what to do if a person’s blood pressure rises to 160/90, then it is first necessary to identify the cause of this condition. As a rule, hypertensive patients are well aware of their disease and the provoking factor is well known to them.
In all other cases, you should consult a doctor. The specialist will give all the necessary recommendations. If blood pressure increases very quickly and is accompanied by a significant deterioration in well-being, then the patient urgently needs to call a medical team.
When medication is not required
If the reason for the increase in blood pressure to 160/90 was an external factor - stress, physical overexertion - then no specific measures to stabilize it will be required. In this case, a person needs to create conditions for proper rest and relaxation. It is necessary to ensure a good flow of fresh air in the room by opening the window or the entire window.
Valerian tincture is used if blood pressure has increased due to a stressful situation
To relieve overexcitation from the central nervous system, doctors recommend taking any tincture with a calming effect. For example, valerian or motherwort. If the condition is accompanied by a severe headache, then you can take any painkiller.
Drug treatment
If blood pressure is constantly maintained at 160/90, then the person needs complex treatment. Therapy requires mandatory medication. The following types of medications are used in the process: diuretics, drugs that dilate the lumens of blood vessels, ACE inhibitors, neurotropic drugs, drugs to restore normal myocardial activity.
How can you reduce the pressure from 160 to 90 if you need to do it quickly? In this case, you can use the following medications:
- Captopril. The tablet is designed to dissolve slowly. To do this, place it under the tongue and wait for complete dissolution. As a rule, the patient's well-being improves over the next 15 minutes. Pathological symptoms go away. A contraindication is individual intolerance to the component composition of the medication.
- Nifedipine. It is also used to quickly lower high blood pressure. The tablet is placed under the tongue.
- Propranalol (modern beta blocker). The drug is recommended to be taken in critical situations. Contraindications: heart failure, bronchial asthma.
Classic drug treatment can be supplemented with folk recipes. But they should not cancel their prescribed medications.
Folk recipes
There are many folk recipes that will help reduce and stabilize blood pressure. Before starting treatment, you must consult with your doctor, since the chosen prescription may have its contraindications.
Among the most effective are the following:
- Pour crushed golden mustache (2 tbsp) with strong alcohol (500 ml). Leave in a dark place for 12 hours to infuse. Take 1 dessert spoon of the tincture in the morning immediately after waking up.
- Prepare oatmeal broth. To do this, boil 50 grams of grains in 5 liters of water for 5 minutes after boiling. Let the mixture stand for 4 hours and boil again. Leave for 2 hours and filter. Pour elecampane root (70 grams) with hot broth after crushing it. Bring to a boil and let cool to room temperature. Add 40 grams of honey. Drink a third of a glass three times a day.
- Pour boiling water (250 ml) over blackcurrant berries (2 tbsp). Boil the composition at a minimum boil for 10 minutes. Leave to infuse for 1 hour and filter. Take the resulting drink ¼ of a glass 4 times a day.
- Combine 1 glass of liquid honey with the same volume of fresh carrot and beet juice. Pour in a little lemon juice and stir. Take 1 tbsp. l. mixture once a day after meals, waiting 3 hours.
Treatment is carried out until the desired effect is achieved.
What to do if the pressure is 160 to 90
Treatment should be carried out using complex methods. If you have tinnitus, dizziness and a strong pulse, you should call an ambulance or, if possible, go to the hospital yourself. In addition to medications that normalize blood pressure, doctors recommend taking diuretics and vasodilators. It is impossible to normalize heart function without the use of sedatives.
In critical cases, urgent measures must be taken to prevent complications. If you have previously been diagnosed with hypertension, then your home medicine cabinet must contain medications that lower your blood pressure. They can be used when there is a sharp jump in indicators and a significant deterioration in the condition. In critical situations, medications must be taken immediately after an attack, and for this it is best to use:
- Captopril - the tablet is placed under the tongue and dissolved for rapid action. Over the course of a quarter of an hour, the condition improves and the main symptoms disappear. The medicine is prohibited for use by people with individual intolerance to substances.
- Nifedipine - a tablet that stops attacks very quickly. For quick action, the tablet is placed under the tongue.
- Propranalol is a modern beta blocker that reduces blood pressure and is used in critical cases. It is not recommended to use the drug in case of heart failure and asthma.
If, after using the described remedies, the pressure remains at the same level, then hospitalization is required, as well as calling an ambulance.
Prognosis and possible complications
The prognosis of hypertension depends on the dynamics of the process, as well as the presence of aggravating factors. The resistant form is difficult to cure. The probability of death in the next decade, according to medical statistics, is 35%. The indicator depends on the severity of damage to target organs.
Aggravating factors include age 45 years and older, alcohol abuse, nicotine addiction, heart disease, endocrine system disease now or in history, predisposition at the genetic level, poor response to drug treatment, advanced hypertension, incorrectly selected therapy, arrhythmias, cardiac deformities .
In the absence of treatment, the development of the following complications is possible:
- stroke;
- myocardial infarction;
- cardiogenic shock;
- heart failure;
- renal/liver failure;
- internal bleeding;
- dementia, ranging from mild cognitive impairment to profound mental retardation.
Almost all complications cause premature death of the patient.
Prevention
The following recommendations from doctors can be considered as preventive measures: adherence to the principles of proper nutrition, giving up alcohol and smoking, maintaining an active lifestyle, daily feasible physical activity, timely treatment of any identified diseases. And it is also important to avoid stressful and any other negative situations.
Regular increase in blood pressure to 160/90 mm Hg. Art. – a good reason to seek qualified medical advice. A person with the second stage of hypertension needs to receive medications.
Only timely diagnosis and appropriate therapy will prevent the development of life-threatening complications and significantly improve the quality of life.
Treatment of hypertension
Arterial hypertension cannot be left untreated. Normalizing high blood pressure can delay or even prevent serious illness. In past years, until the early 90s, hypertension was considered only as a problem of lowering blood pressure. Today it should be considered and treated in conjunction with risk factors for cardiovascular diseases. High blood pressure can be reduced without medication, especially in patients who are significantly overweight, heavy smokers and alcohol drinkers. But these cases are rare and are rather a happy exception, since the vast majority of patients require drug treatment.